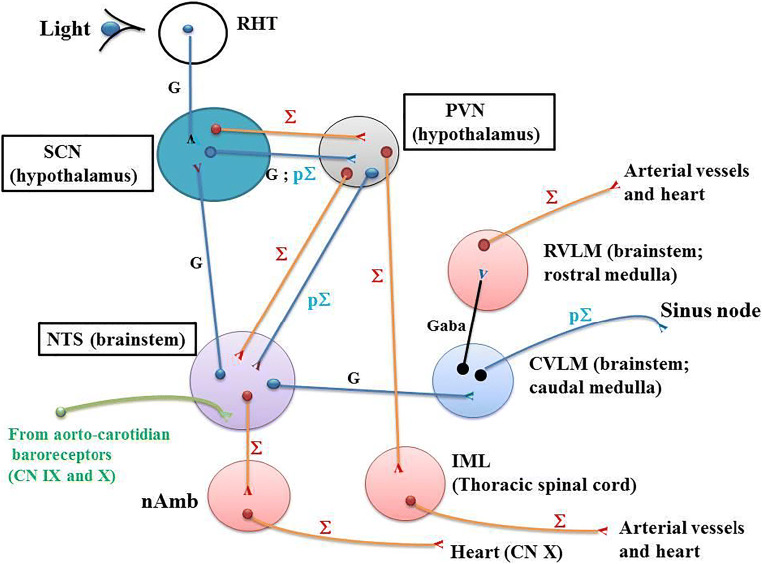
Fig. 1.
Neuroanatomical network involved in the CR of BP. RHT: the retinohypothalamic tract (RHT) originates in the intrinsically photosensitive retinal ganglion cells (ipRGC) which project directly via monosynaptic and glutamatergic transmission to the ventrolateral SCN through the optic nerve and the optic chiasma. ipRGC relay photic information from the eyes to the SCN. SCN: the suprachiasmatic nucleus (SCN) receives glutamatergic neurons from both RHT and nucleus tractus solitarius (NTS). SCN projects glutamatergic pre-autonomic parasympathetic neurons to the PVN. Separate pre-autonomic sympathetic or parasympathetic neurons project to pre-autonomic neurons of the PVN. PVN: paraventricular nucleus (PVN) receives pre-autonomic sympathetic and parasympathetic neurons from the SCN. PVN projects pre-ganglionic sympathetic neurons in the IML. Moreover, pre-autonomic sympathetic neurons in the PVN present axon collaterals to pre-autonomic parasympathetic neurons in the PVN itself and to the NTS [47•, 55]. NTS: nucleus tractus solitarius (NTS) which is located in the brainstem receives neuronal informations from the aortic and carotid baroreceptors which are stimulated after a rapid increase in BP. The carotid sinus baroreceptor axons travel within the glossopharyngeal nerve. The aortic arch baroreceptor axons travel within the vagal nerve. Baroreceptor activity travels along these nerves directly to the NTS. Then, the neuronal activity flows from NTS to both parasympathetic and sympathetic neurons within the brainstem. The NTS neurons send glutamatergic excitatory fibers to the caudal ventrolateral medulla (CVLM). The GABAergic activated CVLM then sends inhibitory fibers to the rostral ventrolateral medulla (RVLM), thus inhibiting the RVLM. The sympathetic and parasympathetic branches of the autonomic nervous system have opposite effects on BP. When the aortic and carotid baroreceptors are activated by an increase in BP, NTS activates CVLM, which in turn inhibits the RVLM. This decreases the activity of the sympathetic branch of the autonomic nervous system, leading to a decrease in BP. Conversely, a decrease in BP decreases baroreceptor activation and induces an increase in sympathetic tone via “disinhibition” of the RVLM. CVLM: caudal ventrolateral medulla (CVLM). The ventrolateral medulla consists of the caudal ventrolateral medulla (CVLM) and the rostral ventrolateral medulla (RVLM). The ventrolateral medulla, part of the medulla oblongata of the brainstem, plays a major role in regulating arterial BP. CVLM receives neurons from the NTS and projects GABA fibers towards RVLM, which in turn inhibits the activity of the RVLM. RVLM: rostral ventrolateral medulla (RVLM). Neurons in the RVLM project directly to pre-ganglionic neurons in the spinal cord (intermediolateral nucleus: IML) which maintain tonic activity of the sympathetic vasomotor nerves. The RVLM is the primary regulator of the sympathetic nervous system, sending glutamatergic excitatory fibers to the sympathetic pre-ganglionic neurons located in the IML of the spinal cord. IML: the intermediolateral nucleus (IML) is located in the lateral grey column of the spinal cord and mediates the entire sympathetic innervation of the body. It receives neurons from the RVLM. nAmb: the nucleus ambiguus (nAmb) is located in the medullary reticular formation and gives rise to efferent motor fibers of the vagal nerve (CN X). These fibers are cardio-inhibitory allowing rapid BP changes in response to fast increases in BP. The parasympathetic outflow arising from nAmb acts to decrease cardiac activity in response to fast increases in BP. nAmb receives fibers from NTS. Symbols: Σ; sympathetic (red); pΣ: parasympathetic (blue); G: glutamatergic neurons