Abstract
Background:
Prior studies suggest exposure to oil and gas development (OGD) adversely affects birth outcomes, but no studies have examined flaring—the open combustion of natural gas—from OGD.
Objectives:
We investigated whether residential proximity to flaring from OGD was associated with shorter gestation and reduced fetal growth in the Eagle Ford Shale of south Texas.
Methods:
We conducted a retrospective cohort study using administrative birth records from 2012 to 2015 () and satellite observations of flaring activity during pregnancy within of maternal residence. Multivariate logistic and linear regression models were used to estimate associations between four outcomes (preterm birth, small-for-gestational age, continuous gestational age, and term birthweight) and exposure to a low (1–9) or high () number of nightly flare events, as compared with no exposure, while controlling for known maternal risk factors. We also examined associations with the number of oil and gas wells within using data from DrillingInfo (now Enverus).
Results:
Exposure to a high number of nightly flare events was associated with a 50% higher odds of preterm birth [ (95% CI: 1.23, 1.83)] and shorter gestation [ (95% CI: , ) d] compared with no exposure. Effect estimates were slightly reduced after adjustment for the number of wells within . In stratified models these associations were present only among Hispanic women. Flaring and fetal growth outcomes were not significantly associated. Women exposed to a high number of wells (fourth quartile, ) vs. no wells within had a higher odds of preterm birth [ (95% CI: 1.14, 1.49)], shorter gestation [ (95% CI: , ) d], and lower average birthweight [ (95% CI: , ) g].
Discussion:
Our study suggests exposure to flaring from OGD is associated with an increased risk of preterm birth. Our findings need to be confirmed in other populations. https://doi.org/10.1289/EHP6394
Introduction
Domestic oil production in the United States has nearly doubled in the last decade, whereas natural gas production has risen roughly 50% to an all-time historical high (EIA 2019c, 2019b). Unconventional techniques of directional drilling and hydraulic fracturing (fracking) have allowed for the exploration and extraction of oil and gas from areas that were previously inaccessible or uneconomic and, in many regions, brought oil and gas development (OGD) into closer proximity to homes. More than 17 million people currently live within of an oil or gas well in the United States, increasing the potential for exposure to contaminants associated with fossil fuel extraction (Czolowski et al. 2017). The potential health hazards associated with OGD activity include contamination of air (Adgate et al. 2014; Shonkoff et al. 2014; Werner et al. 2015) and water (Jackson et al. 2013) by hazardous chemicals and increased psychosocial stress as a result of noise, increased seismic activity, and social hazards associated with disruptions to the local social fabric (Allshouse et al. 2019; Richburg and Slagley 2019; Witter et al. 2013; Adgate et al. 2014). Fracking involves the injection of fluids, sands, and chemical additives into wells to reduce friction, decrease drill time, or stimulate production and include chemicals that are known carcinogens, mutagens, reproductive and developmental toxins, or endocrine disruptors (Webb et al. 2014; Kassotis et al. 2016; Yost et al. 2016; Stringfellow et al. 2017). These compounds can enter the nearby environment through spills, leaks, and volatilization and the disposal of wastewater.
Several recent studies have suggested that living near OGD during pregnancy may elevate the risk of adverse birth outcomes, including preterm birth (Casey et al. 2016; Whitworth et al. 2018), small-for-gestational age (SGA) birth (Stacy et al. 2015; Tran et al. 2020), low birth weight (Hill 2018; Tran et al. 2020), and neural tube defects (Janitz et al. 2019; Mckenzie et al. 2014). However, the findings have not been consistent across studies: McKenzie et al. (2014), Stacy et al. (2015), and Tran et al. (2020) found no association with preterm birth, and Casey et al. (2016) and Whitworth et al. (2018) found no association with SGA. Fetuses are considered to be highly vulnerable to a variety of toxicants because of their physiologic immaturity and developmental susceptibility (Perera et al. 1999). Preterm birth—which is a major predictor of perinatal mortality and may lead to long-term health problems—remains a major public health concern in the United States, where nearly 400,000 babies are born prematurely each year (Martin et al. 2019). Birthweight is also a significant predictor of later cognitive function and cardiovascular disease, even for infants within the normal weight range born at term (Barker 2006; Shenkin et al. 2004).
The exact exposures through which OGD may elevate the risk of adverse birth outcomes remain unclear. One pathway of exposure that has not yet been examined is flaring. Flaring in this context refers to the intentional, controlled combustion of natural gas during the exploration, production, and processing of natural gas, liquids, and oil. Flaring is used for several days or weeks during well production testing after an oil or gas well is initially drilled and hydraulically fractured. Flaring is also used while performing well maintenance and equipment repairs and as a safety measure at processing plants when equipment becomes overpressurized. In addition, flaring is commonly used to dispose of the natural gas that is dissolved in the oil recovered from oil wells. In the United States, hydraulic fracturing has enabled the development of previously inaccessible oil shale formations, resulting in the rapid construction of many widely dispersed oil wells in places that lack a pipeline and other infrastructure to economically collect the associated gas. When local opportunities to use the natural gas are also lacking—for example, for reinjection to enhance oil recovery or for electricity generation on site—it is either vented directly to the atmosphere or combusted in routine flaring that can operate continuously for days or months. Global estimates indicate that more than 139 billion of gas are flared annually, or about 4.6% of the world’s natural gas consumption (Elvidge et al. 2009). The United States has the largest number of flare sites globally, burning an estimated 6.5 billion of natural gas in 2012 (Elvidge et al. 2016). However, regulation and data on the location and timing of flaring is minimal. Monitoring studies indicate that incomplete combustion during the flaring process releases a variety of volatile organic compounds and polycyclic aromatic hydrocarbons along with carbon monoxide, nitrogen oxides, heavy metals, and black carbon (Ite and Ibok 2013; Kindzierski 2000; Leahey et al. 2001; Prenni et al. 2016; Strosher 1996, 2000). Although there have been no studies specifically examining health effects associated with flaring, several of these combustion-related pollutants have been associated with a higher risk of preterm and reduced birthweight in other contexts (Ballester et al. 2010; Brauer et al. 2008; Dadvand et al. 2013). Because flaring is very visible and audible and may produce odors, the practice may also impact fetal growth and development by adding to the anxiety of nearby residents or interrupting sleep (Hiller 2016).
In this study, we utilized satellite observations to characterize exposure to flaring in the Eagle Ford Shale play of south Texas among pregnant women giving birth between 2012 and 2015. The Eagle Ford Shale, which encompasses 27 counties in Southern and Eastern Texas, is one of the most productive oil and gas regions in the country and has experienced a recent boom in production (Figure 1). Due to a weakening of state regulations that previously banned flaring (Willyard 2019), a lack of pipeline capacity for transporting the volumes of natural gas being produced, as well as low gas prices, flaring is a routine practice here. According to the U.S. Energy Information Administration (EIA), Texas flares more natural gas than any other U.S. state (EIA 2019a). Our prior work identified over 43,000 nightly flare events in the region between 2012 and 2016, with a peak in flaring in 2014 and an estimated 4.5 billion of gas flared over the 5-y period (Franklin et al. 2019). Given the high frequency of flaring in the Eagle Ford Shale, we sought to characterize the effects of prenatal exposure to flaring on the risk of multiple adverse birth outcomes among pregnant women as a possible additional mechanism through which OGD may negatively impact the health of nearby communities.
Figure 1.
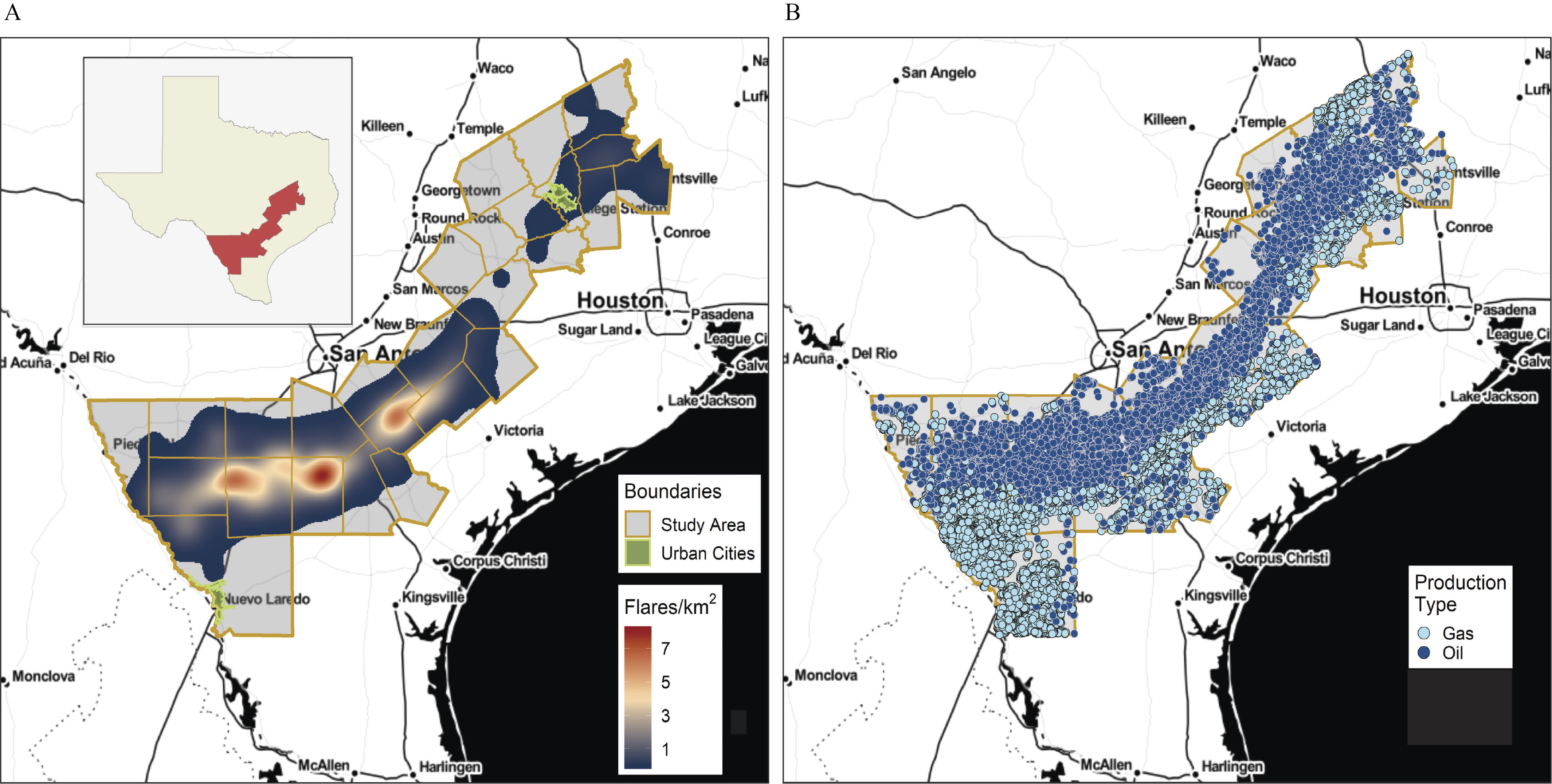
Density of (A) nightly flare events and (B) oil and gas wells across the 27-county Eagle Ford study area, excluding urban areas. Data sources: VIIRS Nightfire (https://www.ngdc.noaa.gov/eog/viirs/) and DrillingInfo (2018) (now Enverus). Counties are delineated in yellow. Green boundaries delineate cities with more than 75,000 people, which were excluded from the analysis. Note: VIIRS, Visible Infrared Imaging Radiometer Suite.
Methods
Study Population
Study protocols were approved by the institutional review boards of the University of Southern California (#HS-17-00652) and the Texas Department of State Health Service (#14-044). Geocoded administrative birth records were obtained from the Texas Department of State Health Services for the years 2012–2015. Our study population consisted of all singleton births lacking birth anomalies and born to women residing within rural areas of the 27 counties comprising the Texas Eagle Ford Shale play (Texas Railroad Commission 2019) between 19 July 2012 and 31 December 2015 (Figure 1). Women residing in cities with a population of more than 75,000 people were excluded because their exposure to other background sources of air pollutants likely differ from women residing in rural areas. This resulted in the exclusion of residents within the municipal boundaries of Laredo, College Station, and Bryan, Texas. The study start date was chosen because the satellite data used to characterize exposure to flaring became available only beginning 1 March 2012. As such, 19 July 2012 was the first possible birth date of an infant born at completed weeks (the shortest gestational age in our sample) and, hence, the earliest birth date for which we could assign complete prenatal exposure. The assembly of our study population is illustrated in Figure S1. Gestational age in days was calculated by taking the difference between recorded last menstrual period (LMP) and date of birth. Records missing the year of LMP, month of LMP, or both, were excluded (3.2% of observations); records missing only the day of LMP were recoded using the 15th of the month (2.3% of observations). We excluded a further 1% of births if their gestational age exceeded 44 completed weeks, they were missing gestational age or birthweight, or if they had an improbable combination of sex-specific birthweight for gestational age, following Alexander et al. (1996). Finally, we excluded 13.9% additional observations by restricting our population to women with an LMP between 1 March 2012 and 20 February 2015 to control for truncation or fixed cohort bias (Strand et al. 2011; Wolf and Armstrong 2012). This restriction ensured that all women pregnant during the study period were included in the analysis and resulted in a final sample of births. Controlling for truncation bias by restricting on LMP rather than date of birth is particularly important when the start and end day of the study period are not consecutive dates (e.g., 1 January and 31 December), as is the case in our study, and when the exposure of interest is seasonal (as was the case with flaring during our study period, which exhibited some seasonality and peaked in winter).
Oil and Gas Wells
The locations of oil and gas wells were obtained from DrillingInfo (2018) (now Enverus). Our analysis included any permitted well location that had an active lease between 1990 and 2016, excluding inactive wells with a plug date or last reported production date before 1 March 2012. We calculated the number of oil or gas wells within a radius of the maternal residence as recorded in the birth record and geocoded by the Texas Department of State Health Services. The number of wells within was then categorized as none, low (1–8), medium (9–26), or high (27–954); these cutoffs corresponded roughly to quartiles of exposure.
Flares
The Nightfire algorithm developed by the National Oceanic and Atmospheric Administration (https://www.ngdc.noaa.gov/eog/viirs/) Earth Observation Group (https://payneinstitute.mines.edu/eog/) detects subpixel () combustion sources at night based on multispectral observations obtained from the Visible Infrared Imaging Radiometer Suite (VIIRS) onboard the Suomi National Polar Partnership satellite (SNPP) (Elvidge et al. 2013). To characterize OGD-related flaring from these data we included only high-temperature observations of , removing lower temperature observations that are more typical of other industrial and biomass burning sources (Elvidge et al. 2016). Furthermore, we applied a hierarchical density-based spatial clustering method to differentiate flares—which tend to persist for many nights, sometimes for months—from aberrant observations, which we excluded. Details on the clustering method used to filter out aberrant observations are provided elsewhere (Franklin et al. 2019).
In the main analysis, exposure to flaring was estimated for all women residing within of an oil or gas well and was defined as the number of individual nightly flare events occurring during pregnancy within a radius of the maternal residence. Exposure to flaring was further categorized into two exposure levels based on the median of exposure among the exposed: low (1–9 flares) or high (10–562 flares). More fine-grained categorization of exposure was not possible due to the low prevalence of exposure in our population () which would have resulted in a small numbers of cases in each category of exposure and zero cells when including covariates. We also considered the total flared area (in meters squared) from all flares occurring during pregnancy within of the maternal residence and categorized this variable similarly based on the median of exposure among the exposed: low () vs. high (). We considered flared area because it may be a better proxy for the volume of gas flared and, hence, the quantity of air pollutant emissions. Unlike the estimates we previously derived for flared gas volume (Franklin et al. 2019)—which were derived in aggregate for the study region and rely upon field-level, monthly self-reported administrative data from the State of Texas—flared area is available for individual nightly flare observations directly from VIIRS. Using flared area thus avoids some of the uncertainty in our flared gas volume estimates at the individual flare level and also allows our method to be more easily reproduced in other areas where data on flared gas volume may not be available. Third, we considered the inverse squared distance-weighted sum of flares within , similarly categorized based on the median of exposure among the exposed: low () vs. high (). The inverse squared distance-weighted sum was calculated as follows:
where i indexes each nightly flare observation within , d is the distance between each nightly flare and the maternal residence in meters, and is the total number of nightly flares within .
Finally, we calculated trimester-specific estimates using our main exposure variable of the number of flares within . However, because trimester-specific and pregnancy-long exposure estimates were highly correlated (Spearman correlation coefficients of 0.73–0.79; see Figure S2), we did not conduct further analysis of trimester-specific exposures.
Outcome Measures
We investigated four outcomes: preterm birth ( of gestation), SGA, continuous gestational age in days, and birthweight among term births (tBW; completed weeks of gestation). SGA was defined as birthweight below the sex-specific 10th percentile of birthweight by gestational week based on the smoothed percentiles for U.S. singleton live births during 2009–2010 (Talge et al. 2014). SGA status was not determined for births at of gestation because the distributions provided in Talge et al. (2014) included only gestational ages between 22 and 44 weeks.
Statistical Analysis
We used separate multivariate linear or logistic regression models to estimate the association between flares and our four outcomes while adjusting for the following known risk factors: maternal age (in 5-y increments from to ), race/ethnicity (Hispanic, non-Hispanic white, other), nativity (U.S. or foreign born), educational attainment (, high school or equivalent, ), prepregnancy body mass index [BMI; underweight or normal (), overweight (), or obese ()], smoking (ever/never during pregnancy), insurance based on primary source of expected payment (private vs. Medicaid, self-pay, or other), parity (nulliparous vs. multiparous), high-risk pregnancy (any of the following: prepregnancy or gestational hypertension or diabetes, preeclampsia, or eclampsia), sex of infant, adequacy of prenatal care (no care, inadequate, intermediate, adequate, ), year of birth (to control for secular trends), and season of birth. Models of tBW were additionally adjusted for gestational age (in weeks). Maternal BMI was calculated from recorded maternal height and weight. Because the prevalence of underweight was very low in our population (3.2%), the categories of underweight and normal BMI were collapsed. Prenatal care was characterized using the Kotelchuck or Adequacy of Prenatal Care Utilization Index, which combines the initiation of prenatal care and the number of prenatal visits to derive a ratio of observed to expected visits, with the number of expected visits based on the American College of Obstetricians and Gynecologists prenatal care standards for uncomplicated pregnancies and adjusted for the gestational age when care began and for the gestational age at delivery (Kotelchuck 1994). Women with expected primary sources of payment of self-pay or other were categorized with the publicly insured due to their low counts and because they more closely resembled those with public insurance than they did women with private insurance with respect to education, nativity, race/ethnicity, and prenatal care. Of the 23,487 births in our sample population, 23,158 included nonmissing information for all covariates and constituted the sample for the multivariate regression analyses.
Because proximity to wells has been associated with adverse birth outcomes in prior studies, and flaring does not occur at all well sites, we conducted a secondary analysis in which we included the number of wells within as an additional covariate in our models. Because prior studies suggest that women of color may be more vulnerable to air pollutant exposures (Ito and Thurston 1996; Morello-Frosch et al. 2010), we conducted a stratified analysis to examine the effects of flaring among Hispanic women and non-Hispanic white women. There were too few women of other races or ethnicities to enable additional stratification. In a post hoc analysis, we also included an indicator variable for residence in a census-designated place (in our study area, a small town or settlement, as opposed to a more rural setting) to see if rurality confounded the association between flaring and the outcomes. All statistical modeling was conducted using Stata IC (release 15.1; StataCorp).
Results
The final sample population included 23,487 births, 10.6% of which were preterm. The majority (55%) of women in the study population identified as Latina or Hispanic, 37% as non-Hispanic white, with few women identifying as non-Hispanic black (6.5%) or Asian or Pacific Islander (0.66%). Nearly 60% of women were on public health insurance (Medicaid) and 17% were foreign born. Other characteristics of the sample population are given in Table 1.
Table 1.
Characteristics of the study population by degree of flaring within of the maternal residence, Eagle Ford Shale, Texas, births between 19 July 2012 and 31 December 2015 ().
| Variable | All () | No flaring () | Low flaring () | High flaring () | -Valuea |
|---|---|---|---|---|---|
| Age [y ()] | 0.032 | ||||
| Education [ (%)] | 0.15 | ||||
| 5,318 (23) | 4,907 (23) | 203 (22) | 208 (22) | ||
| High school diploma/GED | 7,776 (33) | 7,127 (33) | 306 (33) | 343 (37) | |
| Some college or more | 10,375 (44) | 9,583 (44) | 412 (45) | 380 (41) | |
| Missing | 18 (0.1) | 18 (0.1) | — | — | |
| Race/ethnicity [ (%)] | |||||
| Hispanic | 12,904 (55) | 11,853 (55) | 488 (53) | 563 (60) | |
| Non-Hispanic white | 8,704 (37) | 7,992 (37) | 388 (42) | 324 (35) | |
| Non-Hispanic black | 1,535 (6.5) | 1,470 (6.8) | 36 (3.9) | 29 (3.1) | |
| Non-Hispanic Asian/Pacific Islander | 156 (0.7) | 143 (0.7) | |||
| Other, including mixed race | 160 (0.7) | 153 (0.7) | |||
| Missing | 28 (0.1) | 24 (0.1) | — | ||
| Foreign born [ (%)] | |||||
| No | 19,539 (83) | 17,861 (83) | 822 (89) | 856 (92) | |
| Yes | 3,941 (17) | 3,768 (17) | 98 (11) | 75 (8.1) | |
| Missing | — | ||||
| BMI { [ (%)]} | 0.33 | ||||
| Underweight/normal | 10,026 (43) | 9,227 (43) | 416 (45) | 383 (41) | |
| Overweight | 6,185 (26) | 5,689 (26) | 227 (25) | 269 (29) | |
| Obese | 7,106 (30) | 6,559 (30) | 270 (29) | 277 (30) | |
| Missing | 170 (0.7) | 160 (0.7) | |||
| Prenatal care [ (%)] | |||||
| None | 1,858 (7.9) | 1,708 (7.9) | 62 (6.7) | 88 (9.5) | |
| Inadequate | 4,227 (18) | 3,834 (18) | 190 (21) | 203 (22) | |
| Intermediate | 1,994 (8.5) | 1,807 (8.4) | 87 (9.5) | 100 (11) | |
| Adequate | 7,531 (32) | 6,951 (32) | 291 (32) | 289 (31) | |
| 7,877 (34) | 7,335 (34) | 291 (32) | 251 (27) | ||
| Smoking during pregnancy [ (%)] | 0.69 | ||||
| No | 22,226 (95) | 20,479 (95) | 867 (94) | 880 (95) | |
| Yes | 1,183 (5.0) | 1,082 (5.0) | 51 (5.5) | 50 (5.4) | |
| Missing | 78 (0.3) | 74 (0.3) | |||
| Insurance [ (%)] | 0.02 | ||||
| Public | 13,808 (59) | 12,695 (59) | 566 (61) | 547 (59) | |
| Private | 7,690 (33) | 7,068 (33) | 296 (32) | 326 (35) | |
| Self-pay | 963 (4.1) | 910 (4.2) | 23 (2.5) | 30 (3.2) | |
| Other | 994 (4.2) | 931 (4.3) | 36 (3.9) | 27 (2.9) | |
| Missing | 32 (0.1) | 31 (0.1) | — | ||
| High-risk pregnancy [ (%)] | 2,240 (10) | 2,045 (9.5) | 99 (11) | 96 (10) | 0.32 |
| Parity | 0.56 | ||||
| Nulliparous | 8,243 (35) | 7,611 (35) | 320 (35) | 312 (34) | |
| Multiparous | 15,237 (65) | 14,017 (65) | 601 (65) | 619 (65) | |
| Missing | — | — | |||
| Year of birth [ (%)] | |||||
| 2012 | 698 (3.0) | 655 (3.0) | 14 (1.5) | 29 (3.1) | |
| 2013 | 7,471 (32) | 6,765 (31) | 444 (48) | 262 (28) | |
| 2014 | 8,088 (34) | 7,474 (35) | 316 (34) | 298 (32) | |
| 2015 | 7,230 (31) | 6,741 (31) | 147 (16) | 342 (37) | |
| Season of birth [ (%)] | 0.38 | ||||
| Spring (MAM) | 5,443 (23) | 5,002 (23) | 218 (24) | 223 (24) | |
| Summer (JJA) | 6,229 (27) | 5,727 (26) | 268 (29) | 234 (25) | |
| Fall (SON) | 5,974 (25) | 5,505 (25) | 218 (24) | 251 (27) | |
| Winter (DJF) | 5,841 (25) | 5,401 (25) | 217 (24) | 223 (24) | |
| Residence in census-designated place [ (%)] | 11,883 (51) | 10,809 (50) | 475 (52) | 599 (64) |
Note: Cells with counts have been suppressed. Percents may not sum to 100 due to rounding. Exposure to flaring was defined based on the median number of flares within during pregnancy among the exposed (low: 1–9, high: ). —, No data; BMI, body mass index; DJF, December, January, February; GED, general education development; JJA, June, July, August; MAM, March, April, May; SD, standard deviation; SON, September, October, November.
Pearson’s chi-square test or F-test by level of flaring exposure.
Most women (92%) were not exposed to flares within of their residence during pregnancy, whereas 74% were exposed to at least one oil or gas well within . Women who were exposed to flaring were slightly younger, less likely to be African American, less likely to be foreign born, and received lower levels of prenatal care than women who were not exposed to flaring (Table 1). The unadjusted preterm birth rate, mean gestational age, and tBW varied between women exposed to flaring and those who were not (, and , respectively, Pearson’s chi-square or F-test), with women exposed to high levels of flaring having a higher preterm birth rate and lower mean gestational age and tBW compared with those who were not exposed (Table 2). Similar patterns were observed with respect to residential proximity to oil and gas wells (higher preterm birth rate, ; shorter gestational age, ; and lower tBW, compared with the unexposed). As expected, our outcomes also varied by the risk factors we identified a priori, including maternal age, education, race/ethnicity, prenatal care, smoking, insurance, high-risk pregnancy status, and parity (see Table S1).
Table 2.
Birth outcomes by degree of flaring during pregnancy and number of oil and gas wells within of the maternal residence, Eagle Ford Shale, Texas, 2012–2015 ().
| Flares within | -Valuea | Wells within | -Valuea | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 0 () | Low () | High () | 0 () | Low () | Medium () | High () | |||
| Preterm birth [ (%)] | 2,269 (10.5) | 81 (8.8) | 131 (14.1) | 598 (9.7) | 656 (10.6) | 618 (11.3) | 609 (10.9) | 0.04 | |
| Small for gestational age [ (%)] | 2,224 (10.3) | 86 (9.3) | 94 (10.1) | 0.65 | 635 (10.3) | 648 (10.4) | 574 (10.5) | 547 (9.7) | 0.56 |
| Gestational age [weeks ()] | 0.02 | 0.0005 | |||||||
| Term birthweight [g ()] | 0.06 | 0.007 | |||||||
Note: Exposure to flaring was defined based on the number of nightly flares (low: 1–9, high: 10–562), with the cutoff corresponding to the median of exposure among the exposed. The number of wells was categorized as zero, low (1–8), medium (9–26), or high (27–524), with cutoffs corresponding roughly to quartiles of exposure. SD, standard deviation.
Pearson’s chi-square test or F-test by level of exposure.
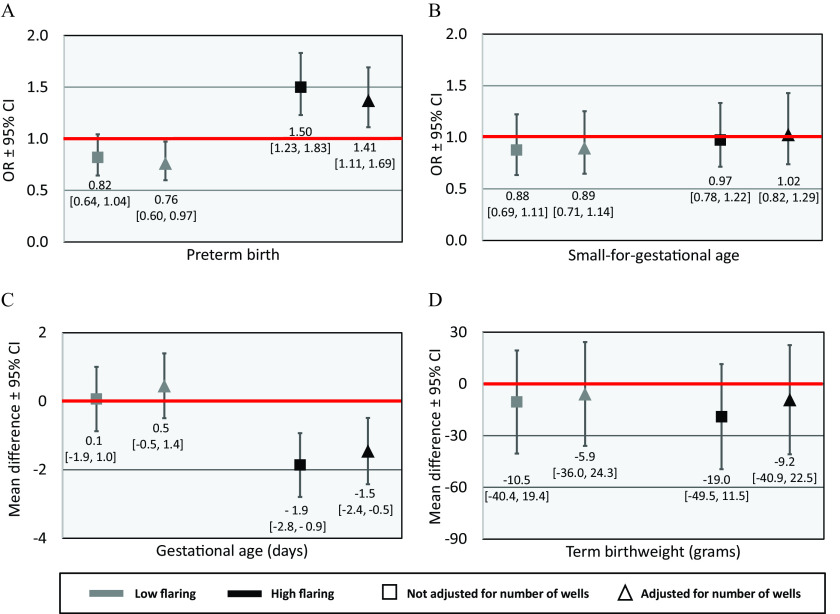
In multivariate models, exposure to a high level of flaring was associated with a 50% higher odds of preterm birth { [95% confidence interval (CI): 1.23, 1.83]} and shorter gestation [mean difference of (95% CI: , ) d] compared with no exposure (Figure 2A,C). Adjusting for the number of wells within reduced the effect estimates slightly [ (95% CI: 1.11, 1.69); mean difference of (95% CI: , ) d] and also suggested that exposure to low levels of flaring (1–9 flares) was associated with a reduced odds of preterm birth [ (95% CI: 0.60, 0.97)] (Figure 2A,C). Associations between flaring and fetal growth outcomes (SGA and tBW) were not statistically significant at (Figure 2B,D). In models that included both the number of flares and wells within , the number of wells was a significant predictor of a higher odds of preterm birth [ (95% CI: 1.14, 1.49) comparing the highest quartile vs. no exposure], shorter gestational age [mean difference of (95% CI: , ) d comparing the highest quartile vs. no exposure], as well as reduced tBW [mean difference of (95% CI: , ) g comparing the highest quartile vs. no exposure and controlling for gestational age] (see Tables S2 and S3). All other covariates generally had effect estimates in the expected direction.
Figure 2.
Estimated associations between the number of flares within of maternal residence and (A) the odds of preterm birth, (B) the odds of small-for-gestational age birth, (C) gestational age, and (D) term birthweight, Eagle Ford Shale, Texas, 2012–2015 (). Full numeric data for models that are unadjusted (Model 1) and adjusted (Model 2) for the number of oil and gas wells within are provided in Tables S2 and S3. Figures show effect estimate and 95% CIs comparing infants with prenatal exposure to a low (1–9) and high (10–562) number of nightly flare events within of the maternal residence to unexposed infants. All estimates are adjusted for maternal age, race/ethnicity, nativity, education, prepregnancy BMI, smoking, insurance, parity, high-risk pregnancy, infant sex, prenatal care, year of birth, and season of birth. Models of term birthweight additionally controlled for gestational age. Red lines indicate the null. Note: BMI, body mass index; CI, confidence interval; OR, odds ratio.
When we modeled exposure to flaring as flared area within , rather than counts, results were generally consistent: Exposure to a high-flared area was associated with a 47% increased odds of preterm birth [ (95% CI: 1.20, 1.79)] and a reduction in mean gestational age [ (95% CI: , ) d] compared with the unexposed in models that did not adjust for the number of wells within (see Tables S4 and S5). Including the number of wells in the models again reduced these effects estimates slightly [ (95% CI: 1.08, 1.65); mean difference of (95% CI: , ) d] (see Tables S4 and S5). Associations between exposure to a high-flared area and SGA or tBW were not statistically significant. Exposure to a low-flared area was associated with a reduced odds of preterm birth, but the association was not statistically significant at in models with or without adjustment for the number of wells within . The number of wells remained a significant predictor of higher odds of preterm birth [ (95% CI: 1.14, 1.49) comparing the highest quartile vs. no exposure], shorter gestational age [mean difference of (95% CI: , ) d comparing the highest quartile vs. no exposure], and reduced tBW [mean difference of (95% CI: , ) g comparing the highest quartile vs. no exposure and controlling for gestational age] in models of flared area. Multivariate models using our third exposure metric of inverse squared distance-weighted sum of flares within also resulted in very similar effect estimates for the associations between high exposure to flares and our four outcomes (see Tables S6 and S7).
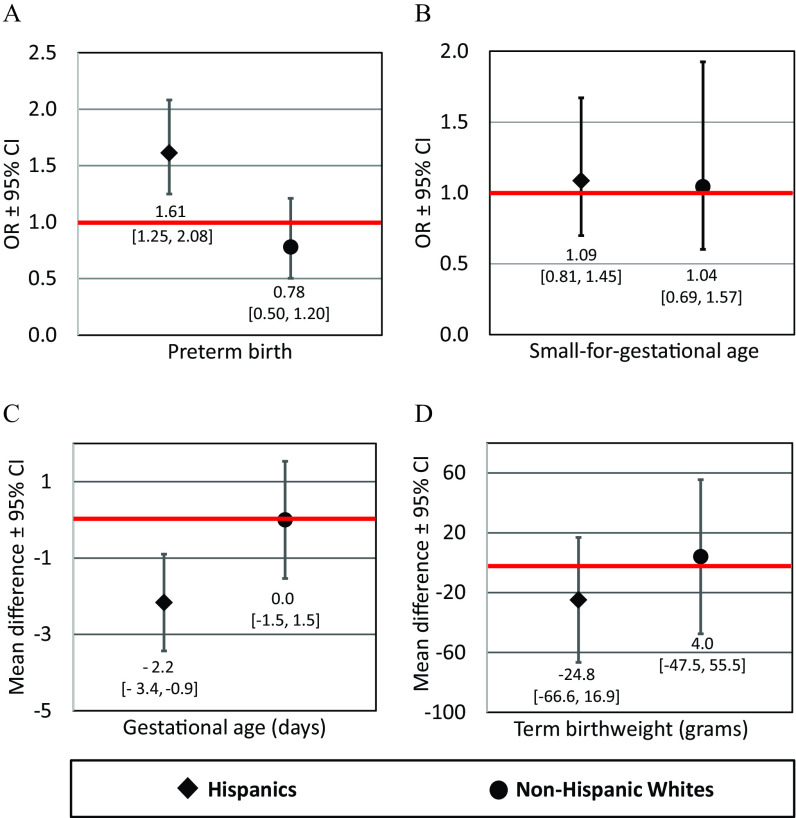
Stratified models using our primary exposure metric suggested that the association between the number of flares within and preterm birth was present only among Hispanic women. Among Hispanics, exposure to a high level of flaring was associated with a 61% higher odds of preterm birth [ (95% CI: 1.25, 2.08)] and shorter gestation [ (95% CI: , ) d] in models that controlled for the number of wells within (Figure 3A,C; see also Tables S8 and S9). Among non-Hispanic white women, the corresponding (95% CI: 0.50, 1.20); the corresponding mean differences in gestational (95% CI: , 1.5) d (Figure 3A,C; see also Tables S8 and S9). Associations between flaring and SGA or tBW were not statistically significant in stratified models of Hispanic or non-Hispanic white women (Figure 3B,D).
Figure 3.
Estimated associations from models stratified by ethnicity between the number of flares within of maternal residence and (A) the odds of preterm birth, (B) the odds of small-for-gestational age birth, (C) gestational age, and (D) term birthweight, Eagle Ford Shale, Texas, 2012–2015 (, Hispanic women and non-Hispanic white women). Full numeric data are provided in Tables S8 and S9. Figures show effect estimates and 95% CIs comparing infants with prenatal exposure to a low (1–9) and high (10–562) number of nightly flare events within of the maternal residence to unexposed infants. All estimates are adjusted for the number of oil and gas wells within , maternal age, nativity, education, prepregnancy BMI, smoking, insurance, parity, high-risk pregnancy, infant sex, prenatal care, year of birth, and season of birth. Models of term birthweight additionally control for gestational age. Red lines indicate the null. Note: BMI, body mass index; CI, confidence interval; OR, odds ratio.
Our post hoc sensitivity analysis including residence in a census-designated place in the main preterm birth model did not change the magnitude, direction, or statistical significance of effect estimates. The coefficients for census-designated place was also not statistically significant (see Table S10).
Discussion
As far as we are aware, this is the first study to examine the potential effects of flaring from oil and gas extraction on human health. Our retrospective cohort study of births between 2012 and 2015 in the Eagle Ford Shale region of south Texas suggests that prenatal exposure to flaring from OGD is associated with a significant increase in the risk of preterm birth and a shorter length of gestation among pregnant women living nearby. Because we included the number of oil and gas wells in our models, our findings suggest the effects of flaring on the length of gestation are independent of other potential exposures related to oil and gas wells.
Our stratified analysis suggested that Hispanic women were vulnerable to the effects of flaring on preterm birth, whereas non-Hispanic white women were not. As far as we are aware, this is the first study to document greater health impacts associated with OGD among women of color. A history of government-sanctioned discrimination in housing, employment, and education have led Hispanics in Texas to be socioeconomically disadvantaged, with a 2014 median household income of compared with for non-Hispanic whites and with a greater proportion living below the federal poverty level (23% vs. 9.3% among non-Hispanic whites) (Texas Health and Human Services Commission 2014). Reasons why women of color and lower socioeconomic status may experience greater vulnerability to flaring could relate to differences in preexisting health status (because income and education are directly related to health); greater co-exposures to other pollutants (e.g., because pollution sources are disproportionately located in communities of color); a compromised ability to cope with the adverse effects of pollution due to poor nutrition or limited access to health care, preventative or social services; and modifying effects of psychosocial stress associated with living in poverty or experiencing discrimination. Belonging to a racial or ethnic group that experiences systemic discrimination may confer greater vulnerability due to the physiological effects of chronic psychosocial stress (Geronimus 1992). Evidence suggests that chronic stress can result in physiological wear and tear on the body that can increase vulnerability to environmental stressors by impairing immune function, increasing the absorption of toxicants (McEwen 1998), by compromising the body’s defense systems, or by directly causing illness or affecting the same physiological process as the environmental toxicant (Clougherty and Kubzansky 2009; Gee and Payne-Sturges 2004; Gordon 2003; Morello-Frosch and Shenassa 2006). Although we were not able to directly examine stress or say why Hispanic women in our study were more vulnerable, our findings are consistent with prior studies that found socially disadvantaged women—including African Americans and residents of socioeconomically disadvantaged neighborhoods—are more vulnerable to the impacts of ambient air pollution, including larger reductions in birth weight associated with exposure to particulate matter (Erickson et al. 2016; Morello-Frosch et al. 2010; Westergaard et al. 2017). In addition, it is possible there is a threshold effect of flaring and that the lack of an association among non-Hispanic white women that we observed may have been the result of the fact that they were exposed to a lower average number of nightly flare events than Hispanic women (mean of 24.1 vs. 36.3 among the exposed).
We found no evidence of an association between flaring and SGA or reduced birthweight among term infants when controlling for gestational age. The lack of strong associations with these outcomes may be due to a lack of a true effect on fetal growth independent of gestational age or to power limitations resulting from the low prevalence of exposure to flaring in our study population. For example, given the prevalence of SGA (10.2%) and exposure to flaring (7.9%) in our study population, we estimate that we had power of only 0.52 to detect a true OR of 1.2 at .
We found that women exposed to low levels of flaring had a reduced odds of preterm birth compared with women with no exposure in models that controlled for well density. This counterintuitive finding was no longer statistically significant when we measured exposure to flaring on the basis of flared area or the inverse squared distance-weighted sum of nightly flare events, which may better approximate the quantity and proximity of flared gas than the number of flares, suggesting the association may have been spurious, or the result of a threshold or nonlinear effect that we were not able to estimate given the small number of exposed women in our sample (). It is also possible that low levels of flaring may appear protective because women exposed to low levels of flaring live in more rural settings than those exposed to no flaring [median (mean) (699) people per square kilometer for the low-flare group vs. 452 (1,063) for the no-flare group] and are, therefore, less exposed to other pollutants such as traffic-related air pollution, resulting in residual confounding. However, a lack of regulatory air pollution monitoring in our study region prohibits us from being able to further assess this potential source of bias. Adding an indicator variable for residence in a census-designated place (in our study area, a small town, as opposed to a more rural setting) to our models in a post hoc analysis did not change the magnitude, direction, or statistical significance of effect estimate for the association between low levels of flaring and preterm birth (see Table S9).
In addition to flaring, we also found that living within of oil and gas wells was independently associated with adverse birth outcomes, including a higher odds of preterm birth, reduced gestational age, and reduced tBW, controlling for gestational age. The association with preterm birth is consistent with previous studies from Pennsylvania and Northern Texas in areas of OGD but absent of significant flaring activity (Casey et al. 2016; Whitworth et al. 2018). Other studies from Southwest Pennsylvania, Colorado, and California have found no evidence of such an association with preterm birth (Mckenzie et al. 2014; Stacy et al. 2015; Tran et al. 2020). In contrast to our findings, the majority of previous studies have found little evidence of an association between residential proximity to OGD and birthweight, with the exception of Stacy et al. (2015) and Tran et al. (2020). Our contrasting findings could be related to differences in our study design and the nature of OGD in the Eagle Ford Shale, which includes significant oil as well as gas production and conventionally drilled as well as unconventionally drilled wells. (With the exception of the California study, prior studies have focused on natural gas wells that were unconventionally drilled.)
Our findings hold broader implications for other populations exposed to flaring from OGD. Flaring activity has increased dramatically in the United States over the last five years, spiking by nearly 50% in 2018 from the previous year, the largest absolute gains of any country (World Bank 2019). Beyond the Eagle Ford Shale, flaring is common in the Permian Basin of West Texas and Eastern New Mexico as well as the Bakken Shale of North Dakota and Western Montana. In fact, a recent study suggests that as of 2015, the Permian Basin has had more flare activity and appears to flare larger volumes, on average, than the Eagle Ford play (Willyard and Schade 2019). In the Bakken Shale play, it is estimated that 28% of North Dakota’s total produced natural gas was flared (Gvakharia et al. 2017). The health impacts of flaring therefore warrant additional study, and our findings require replication in other populations. Prior work has demonstrated associations between flaring and increased risk of stillbirth among cattle as well as increased risk of calf mortality (Bamberger and Oswald 2012). However, we are unaware of any previous studies assessing the health impacts of flaring from OGD among humans.
We utilized a novel exposure metric derived from infrared satellite observations that provides an objective, highly spatially and temporally resolved measure of flaring activity. In places such as our study region, where industrial activity is minimal, combustion sources detected using this method are unlikely to come from sources other than flaring. This approach provides distinct advantages over alternative available measures of flaring, including self-reported regulatory data, which is likely to underestimate the magnitude of flaring and is provided only in the aggregate (monthly, lease-level). However, our measure only indirectly reflects potential exposures, including air pollutant emissions. We are, therefore, unable to determine the mechanism(s) through which flaring may adversely affect birth outcomes. Monitoring studies have indicated that incomplete combustion during the flaring process can release a variety of air pollutants, including particulate matter, which has been linked to preterm birth and reduced fetal growth in other contexts (Ballester et al. 2010; Brauer et al. 2008; Dadvand et al. 2013). However, there is a lack of air pollutant monitoring data in areas with flaring due to OGD, which are primarily rural.
Because we relied on live birth records, we were unable to assess potential effects of flaring on the risk of miscarriage. We were also unable to examine critical windows of exposure due to the high correlation between pregnancy-long and trimester-specific estimates of exposure to flaring in our population. Another limitation of our study is that we were unable to capture maternal mobility because only the birth mother’s place of residence at the time of birth is recorded in the birth records. Prior studies have suggested that ignoring residential mobility may bias associations toward the null due to nondifferential exposure misclassification, and that moving distances during pregnancy are typically relatively short and within the same county (Bell and Belanger 2012; Chen et al. 2010; Hodgson et al. 2015; Lupo et al. 2010; Miller et al. 2010; Pennington et al. 2017).
Together, our findings suggest that living within of OGD wells and flaring activity may have had a significant adverse effect on birth outcomes among pregnant women in the Eagle Ford region. The fact that much of the region is low income and approximately 50% of residents living within of an oil or gas well are people of color raises environmental justice concerns about the potential health impacts of the oil and gas boom in south Texas (Johnston et al. 2016). Measures to minimize flaring—such as more stringent regulation of flaring or investments in renewable energy and energy efficiency measures that reduce reliance on fossil fuels overall—could protect the health of infants.
Supplementary Material
Acknowledgments
This work was supported by a grant from the National Institutes of Health/National Institute of Environmental Health Sciences (R21-ES028417). The source of data for this analysis was 2012–2015 birth records provided by the Texas Department of State Health Services, Center for Health Statistics. All interpretations drawn from these data are those of the authors and not the Texas Department of State Health Services.
References
- Adgate JL, Goldstein BD, McKenzie LM. 2014. Potential public health hazards, exposures and health effects from unconventional natural gas development. Environ Sci Technol 48(15):8307–8320, PMID: 24564405, 10.1021/es404621d. [DOI] [PubMed] [Google Scholar]
- Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M. 1996. A United States national reference for fetal growth. Obstet Gynecol 87(2):163–168, PMID: 8559516, 10.1016/0029-7844(95)00386-X. [DOI] [PubMed] [Google Scholar]
- Allshouse WB, McKenzie LM, Barton K, Brindley S, Adgate JL. 2019. Community noise and air pollution exposure during the development of a multi-well oil and gas pad. Environ Sci Technol 53(12):7126–7135, PMID: 31136715, 10.1021/acs.est.9b00052. [DOI] [PubMed] [Google Scholar]
- Ballester F, Estarlich M, Iñiguez C, Llop S, Ramón R, Esplugues A, et al. . 2010. Air pollution exposure during pregnancy and reduced birth size: a prospective birth cohort study in Valencia, Spain. Environ Health 9:6, PMID: 20113501, 10.1186/1476-069X-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bamberger M, Oswald RE. 2012. Impacts of gas drilling on human and animal health. New Solut 22(1):51–77, PMID: 22446060, 10.2190/NS.22.1.e. [DOI] [PubMed] [Google Scholar]
- Barker DJP. 2006. Adult consequences of fetal growth restriction. Clin Obstet Gynecol 49(2):270–283, PMID: 16721106, 10.1097/00003081-200606000-00009. [DOI] [PubMed] [Google Scholar]
- Bell ML, Belanger K. 2012. Review of research on residential mobility during pregnancy: consequences for assessment of prenatal environmental exposures. J Expo Sci Environ Epidemiol 22(5):429–438, PMID: 22617723, 10.1038/jes.2012.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brauer M, Lencar C, Tamburic L, Koehoorn M, Demers P, Karr C. 2008. A cohort study of traffic-related air pollution impacts on birth outcomes. Environ Health Perspect 116(5):680–686, PMID: 18470315, 10.1289/ehp.10952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey JA, Savitz DA, Rasmussen SG, Ogburn EL, Pollak J, Mercer DG, et al. . 2016. Unconventional natural gas development and birth outcomes in Pennsylvania, USA. Epidemiology 27(2):163–172, PMID: 26426945, 10.1097/EDE.0000000000000387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L, Bell EM, Caton AR, Druschel CM, Lin S. 2010. Residential mobility during pregnancy and the potential for ambient air pollution exposure misclassification. Environ Res 110(2):162–168, PMID: 19963212, 10.1016/j.envres.2009.11.001. [DOI] [PubMed] [Google Scholar]
- Clougherty JE, Kubzansky LD. 2009. A framework for examining social stress and susceptibility to air pollution in respiratory health. Environ Health Perspect 117(9):1351–1358, PMID: 19750097, 10.1289/ehp.0900612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czolowski ED, Santoro RL, Srebotnjak T, Shonkoff SBC. 2017. Toward consistent methodology to quantify populations in proximity to oil and gas development: a national spatial analysis and review. Environ Health Perspect 125(8):086004, PMID: 28858829, 10.1289/EHP1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dadvand P, Parker J, Bell ML, Bonzini M, Brauer M, Darrow LA, et al. . 2013. Maternal exposure to particulate air pollution and term birth weight: a multi-country evaluation of effect and heterogeneity. Environ Health Perspect 121(3):367–373, PMID: 23384584, 10.1289/ehp.1205575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DrillingInfo. 2018. Enverus. Energy industry solutions. https://www.enverus.com/ [accessed 17 September 2018].
- EIA (U.S. Energy Information Administration). 2019a. Natural gas vented and flared. https://www.eia.gov/dnav/ng/ng_prod_sum_a_EPG0_VGV_mmcf_a.htm [accessed 25 July 2019].
- EIA. 2019b. U.S. dry natural gas production (million cubic feet). https://www.eia.gov/dnav/ng/hist/n9070us2a.htm [accessed 25 July 2019].
- EIA. 2019c. U.S. field production of crude oil (thousand barrels). https://www.eia.gov/dnav/pet/hist/LeafHandler.ashx?n=PET&s=MCRFPUS1&f=A [accessed 25 July 2019].
- Elvidge CD, Zhizhin M, Baugh K, Hsu F-C, Ghosh T. 2016. Methods for global survey of natural gas flaring from visible infrared imaging radiometer suite data. Energies 9(1):14, 10.3390/en9010014. [DOI] [Google Scholar]
- Elvidge CD, Ziskin D, Baugh KE, Tuttle BT, Ghosh T, Pack DW, et al. . 2009. A fifteen year record of global natural gas flaring derived from satellite data. Energies 2(3):595–622, 10.3390/en20300595. [DOI] [Google Scholar]
- Elvidge CD, Zhizhin M, Hsu F-C, Baugh KE. 2013. VIIRS nightfire: satellite pyrometry at night. Remote Sens 5(9):4423–4449, 10.3390/rs5094423. [DOI] [Google Scholar]
- Erickson AC, Ostry A, Chan LHM, Arbour L. 2016. The reduction of birth weight by fine particulate matter and its modification by maternal and neighbourhood-level factors: a multilevel analysis in British Columbia, Canada. Environ Health 15:51, PMID: 27079512, 10.1186/s12940-016-0133-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklin M, Chau K, Cushing LJ, Johnston J. 2019. Characterizing flaring from unconventional oil and gas operations in south Texas using satellite observations. Environ Sci Technol 53(4):2220–2228, PMID: 30657671, 10.1021/acs.est.8b05355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, Payne-Sturges DC. 2004. Environmental health disparities: a framework integrating psychosocial and environmental concepts. Environ Health Perspect 112(17):1645–1653, PMID: 15579407, 10.1289/ehp.7074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT. 1992. The weathering hypothesis and the health of African-American women and infants: evidence and speculations. Ethn Dis 2(3):207–221, PMID: 1467758. [PubMed] [Google Scholar]
- Gordon CJ. 2003. Role of environmental stress in the physiological response to chemical toxicants. Environ Res 92(1):1–7, PMID: 12706749, 10.1016/S0013-9351(02)00008-7. [DOI] [PubMed] [Google Scholar]
- Gvakharia A, Kort EA, Brandt A, Peischl J, Ryerson TB, Schwarz JP, et al. . 2017. Methane, black carbon, and ethane emissions from natural gas flares in the Bakken Shale, North Dakota. Environ Sci Technol 51(9):5317–5325, PMID: 28401762, 10.1021/acs.est.6b05183. [DOI] [PubMed] [Google Scholar]
- Hill EL. 2018. Shale gas development and infant health: evidence from Pennsylvania. J Health Econ 61:134–150, PMID: 30114565, 10.1016/j.jhealeco.2018.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiller J. 2016. Is Eagle Ford oil boom making people sick? San Antonio Express-News, 5 August 2016 https://www.mysanantonio.com/business/eagle-ford-energy/article/Is-Eagle-Ford-oil-boom-making-people-sick-9125789.php [accessed 22 June 2020].
- Hodgson S, Lurz PWW, Shirley MDF, Bythell M, Rankin J. 2015. Exposure misclassification due to residential mobility during pregnancy. Int J Hyg Environ Health 218(4):414–421, PMID: 25845985, 10.1016/j.ijheh.2015.03.007. [DOI] [PubMed] [Google Scholar]
- Ite AE, Ibok UJ. 2013. Gas flaring and venting associated with petroleum exploration and production in the Nigeria’s Niger Delta. Am J Environ Prot 1(4):70–77, 10.12691/env-1-4-1. [DOI] [Google Scholar]
- Ito K, Thurston GD. 1996. Daily PM10/mortality associations: an investigations of at-risk subpopulations. J Expo Anal Environ Epidemiol 6(1):79–95, PMID: 8777375. [PubMed] [Google Scholar]
- Jackson RE, Gorody AW, Mayer B, Roy JW, Ryan MC, Van Stempvoort DR. 2013. Groundwater protection and unconventional gas extraction: the critical need for field‐based hydrogeological research. Ground Water 51(4):488–510, PMID: 23745972, 10.1111/gwat.12074. [DOI] [PubMed] [Google Scholar]
- Janitz AE, Dao HD, Campbell JE, Stoner JA, Peck JD. 2019. The association between natural gas well activity and specific congenital anomalies in Oklahoma, 1997–2009. Environ Int 122:381–388, PMID: 30551805, 10.1016/j.envint.2018.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston JE, Werder E, Sebastian D. 2016. Wastewater disposal wells, fracking, and environmental injustice in Southern Texas. Am J Public Health 106(3):550–556, PMID: 26794166, 10.2105/AJPH.2015.303000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassotis CD, Iwanowicz LR, Akob DM, Cozzarelli IM, Mumford AC, Orem WH, et al. . 2016. Endocrine disrupting activities of surface water associated with a West Virginia oil and gas industry wastewater disposal site. Sci Total Environ 557–558:901–910, PMID: 27073166, 10.1016/j.scitotenv.2016.03.113. [DOI] [PubMed] [Google Scholar]
- Kindzierski WB. 2000. Importance of human environmental exposure to hazardous air pollutants from gas flares. Environ Rev 8(1):41–62, 10.1139/a00-005. [DOI] [Google Scholar]
- Kotelchuck M. 1994. An evaluation of the Kessner Adequacy of Prenatal Care Index and proposed Adequacy of Prenatal Care Utilization Index. Am J Public Health 84(9):1414–1420, PMID: 8092364, 10.2105/ajph.84.9.1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leahey DM, Preston K, Strosher M. 2001. Theoretical and observational assessments of flare efficiencies. J Air Waste Manag Assoc 51(12):1610–1616, PMID: 15666465, 10.1080/10473289.2001.10464390. [DOI] [PubMed] [Google Scholar]
- Lupo PJ, Symanski E, Chan W, Mitchell LE, Waller DK, Canfield MA, et al. . 2010. Differences in exposure assignment between conception and delivery: the impact of maternal mobility. Paediatr Perinat Epidemiol 24(2):200–208, PMID: 20415777, 10.1111/j.1365-3016.2010.01096.x. [DOI] [PubMed] [Google Scholar]
- Martin JA, Hamilton BE, Osterman MJK, Driscoll AK. 2019. Births: final data for 2018. Natl Vital Stat Rep 68(13):1–47, PMID: 32501202. [PubMed] [Google Scholar]
- McEwen BS. 1998. Protective and damaging effects of stress mediators. N Engl J Med 338(3):171–179, PMID: 9428819, 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- McKenzie LM, Guo R, Witter RZ, Savitz DA, Newman LS, Adgate JL. 2014. Birth outcomes and maternal residential proximity to natural gas development in rural Colorado. Environ Health Perspect 122(4):412–417, PMID: 24474681, 10.1289/ehp.1306722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller A, Siffel C, Correa A. 2010. Residential mobility during pregnancy: patterns and correlates. Matern Child Health J 14(4):625–634, PMID: 19568920, 10.1007/s10995-009-0492-z. [DOI] [PubMed] [Google Scholar]
- Morello-Frosch R, Jesdale BM, Sadd JL, Pastor M. 2010. Ambient air pollution exposure and full-term birth weight in California. Environ Health 9:44, PMID: 20667084, 10.1186/1476-069X-9-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morello-Frosch R, Shenassa ED. 2006. The environmental “riskscape” and social inequality: implications for explaining maternal and child health disparities. Environ Health Perspect 114(8):1150–1153, PMID: 16882517, 10.1289/ehp.8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pennington AF, Strickland MJ, Klein M, Zhai X, Russell AG, Hansen C, et al. . 2017. Measurement error in mobile source air pollution exposure estimates due to residential mobility during pregnancy. J Expo Sci Environ Epidemiol 27(5):513–520, PMID: 27966666, 10.1038/jes.2016.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perera FP, Jedrychowski W, Rauh V, Whyatt RM. 1999. Molecular epidemiologic research on the effects of environmental pollutants on the fetus. Environ Health Perspect 107(suppl 3):451–460, PMID: 10346993, 10.1289/ehp.99107s3451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prenni AJ, Day DE, Evanoski-Cole AR, Sive BC, Hecobian A, Zhou Y, et al. . 2016. Oil and gas impacts on air quality in federal lands in the Bakken region: an overview of the Bakken Air Quality Study and first results. Atmos Chem Phys 16(3):1401–1416, 10.5194/acp-16-1401-2016. [DOI] [Google Scholar]
- Richburg CM, Slagley J. 2019. Noise concerns of residents living in close proximity to hydraulic fracturing sites in Southwest Pennsylvania. Public Health Nurs 36(1):3–10, PMID: 30298676, 10.1111/phn.12540. [DOI] [PubMed] [Google Scholar]
- Shenkin SD, Starr JM, Deary IJ. 2004. Birth weight and cognitive ability in childhood: a systematic review. Psychol Bull 130(6):989–1013, PMID: 15535745, 10.1037/0033-2909.130.6.989. [DOI] [PubMed] [Google Scholar]
- Shonkoff SB, Hays J, Finkel ML. 2014. Environmental public health dimensions of shale and tight gas development. Environ Health Perspect 122(8):787–795, PMID: 24736097, 10.1289/ehp.1307866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stacy SL, Brink LL, Larkin JC, Sadovsky Y, Goldstein BD, Pitt BR, et al. . 2015. Perinatal outcomes and unconventional natural gas operations in Southwest Pennsylvania. PLoS One 10(6):e0126425, PMID: 26039051, 10.1371/journal.pone.0126425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strand LB, Barnett AG, Tong S. 2011. Methodological challenges when estimating the effects of season and seasonal exposures on birth outcomes. BMC Med Res Methodol 11:49, PMID: 21501523, 10.1186/1471-2288-11-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringfellow WT, Camarillo MK, Domen JK, Sandelin WL, Varadharajan C, Jordan PD, et al. . 2017. Identifying chemicals of concern in hydraulic fracturing fluids used for oil production. Environ Pollut 220(pt A):413–420, PMID: 27743793, 10.1016/j.envpol.2016.09.082. [DOI] [PubMed] [Google Scholar]
- Strosher M. 1996. Investigations of Flare Gas Emissions in Alberta. EUG/AGS Special Rep 5. Calgary, AB, Canada: Environment Canada Conservation and Protection and Alberta Energy and Utilities Board; [accessed 22 June 2020]. [Google Scholar]
- Strosher MT. 2000. Characterization of emissions from diffusion flare systems. J Air Waste Manag Assoc 1995 50(10):1723–1733, PMID: 28076230, 10.1080/10473289.2000.10464218. [DOI] [PubMed] [Google Scholar]
- Talge NM, Mudd LM, Sikorskii A, Basso O. 2014. United States birth weight reference corrected for implausible gestational age estimates. Pediatrics 133(5):844–853, PMID: 24777216, 10.1542/peds.2013-3285. [DOI] [PubMed] [Google Scholar]
- Texas Health and Human Services Commission. 2014. Hispanic or Latino Profile in Texas. https://hhs.texas.gov/sites/default/files/documents/about-hhs/process-improvement/cedd/fact-sheets/hispanic-profile-texas.pdf [accessed 28 June 2020].
- Texas Railroad Commission. 2019. Eagle Ford Shale Information. https://www.rrc.state.tx.us/oil-gas/major-oil-and-gas-formations/eagle-ford-shale-information [accessed 26 July 2019].
- Tran KV, Casey JA, Cushing LJ, Morello-Frosch RA. 2020. Residential proximity to oil and gas development and birth outcomes in California: a retrospective cohort study of 2006–2015 births. Environ Health Perspect 128(6):67001, PMID: 32490702, 10.1289/EHP5842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb E, Bushkin-Bedient S, Cheng A, Kassotis CD, Balise V, Nagel SC. 2014. Developmental and reproductive effects of chemicals associated with unconventional oil and natural gas operations. Rev Environ Health 29(4):307–318, PMID: 25478730, 10.1515/reveh-2014-0057. [DOI] [PubMed] [Google Scholar]
- Werner AK, Vink S, Watt K, Jagals P. 2015. Environmental health impacts of unconventional natural gas development: a review of the current strength of evidence. Sci Total Environ 505:1127–1141, PMID: 25461113, 10.1016/j.scitotenv.2014.10.084. [DOI] [PubMed] [Google Scholar]
- Westergaard N, Gehring U, Slama R, Pedersen M. 2017. Ambient air pollution and low birth weight—are some women more vulnerable than others? Environ Int 104:146–154, PMID: 28390661, 10.1016/j.envint.2017.03.026. [DOI] [PubMed] [Google Scholar]
- Whitworth KW, Marshall AK, Symanski E. 2018. Drilling and production activity related to unconventional gas development and severity of preterm birth. Environ Health Perspect 126(3):037006, PMID: 29578659, 10.1289/EHP2622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willyard KA. 2019. An historical political economy analysis and review of Texas oil and gas well flaring laws and policy. Energy Policy 128:639–647, 10.1016/j.enpol.2019.01.046. [DOI] [Google Scholar]
- Willyard KA, Schade GW. 2019. Flaring in two Texas shale areas: comparison of bottom-up with top-down volume estimates for 2012 to 2015. Sci Total Environ 691:243–251, PMID: 31323570, 10.1016/j.scitotenv.2019.06.465. [DOI] [PubMed] [Google Scholar]
- Witter RZ, McKenzie L, Stinson KE, Scott K, Newman LS, Adgate J. 2013. The use of health impact assessment for a community undergoing natural gas development. Am J Public Health 103(6):1002–1010, PMID: 23597363, 10.2105/AJPH.2012.301017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf J, Armstrong B. 2012. The association of season and temperature with adverse pregnancy outcome in two German states, a time-series analysis. PLoS One 7(7):e40228, PMID: 22792247, 10.1371/journal.pone.0040228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank. 2019. Increased shale oil production and political conflict contribute to increase in global gas flaring. Press release. 12 June 2019. https://www.worldbank.org/en/news/press-release/2019/06/12/increased-shale-oil-production-and-political-conflict-contribute-to-increase-in-global-gas-flaring.print [accessed 22 June 2020].
- Yost EE, Stanek J, DeWoskin RS, Burgoon LD. 2016. Overview of chronic oral toxicity values for chemicals present in hydraulic fracturing fluids, flowback, and produced waters. Environ Sci Technol 50(9):4788–4797, PMID: 27050380, 10.1021/acs.est.5b04645. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.