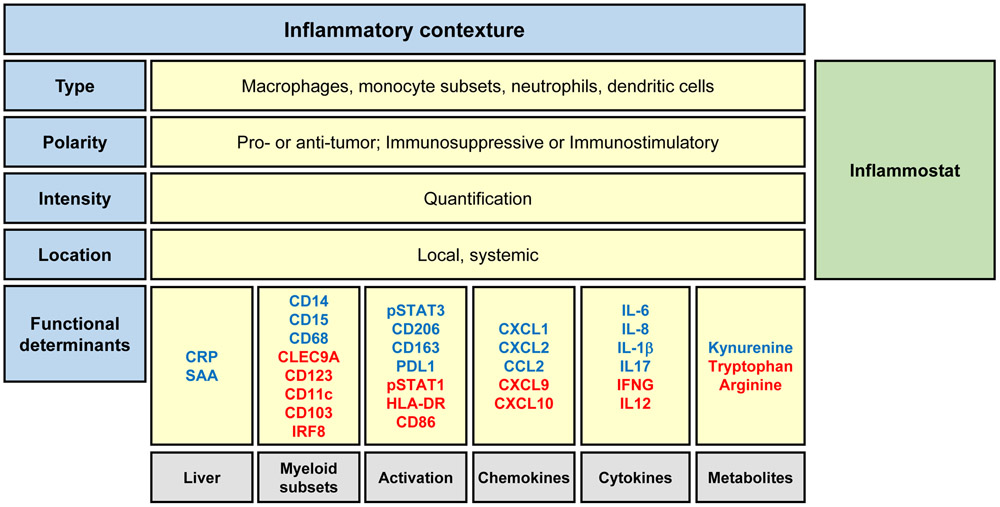
Figure 2. Graphical representation of the Inflammatory Contexture and Inflammostat.
The inflammatory contexture is defined as the type, polarity, intensity, and location of cancer inflammation. Parameters comprising the inflammatory contexture include myeloid cell subsets detected within the blood and tumor (type), the functional phenotype of myeloid cells (polarity), and the intensity of the inflammatory response (intensity) determined by cell density within tumors and the magnitude of inflammatory factors present within the bloodstream (location). The immunostat, a rheostat of the inflammatory reaction, is derived from the magnitude and polarity of the inflammatory contexture and serves as a fundamental regulator of immunosurveillance. A high inflammostat signifies an immunological state that is unlikely to respond to therapies that seek to solely engage T cell immunosurveillance by derailing immune checkpoints (e.g. CTLA4 and PD1/PDL1). The functional orientation of the inflammatory contexture is characterized by proteins and their activation status (e.g. phosphorylation) that predict the phenotype of inflammatory cells (e.g. immunostimulatory or immunosuppressive) and that associate with responses to immunotherapy. Shown are a select set of proposed determinants and their association with immune suppression (blue) or stimulation (red). Abbreviations: CRP, c-reactive protein; CXCL/CCL, chemokine motif ligands; IFNG, interferon gamma; IRF8, interferon regulatory factor 8; IL, interleukin; PDL1, programmed death-ligand 1; SAA, serum amyloid A; STAT, signal transducer and activator of transcription.