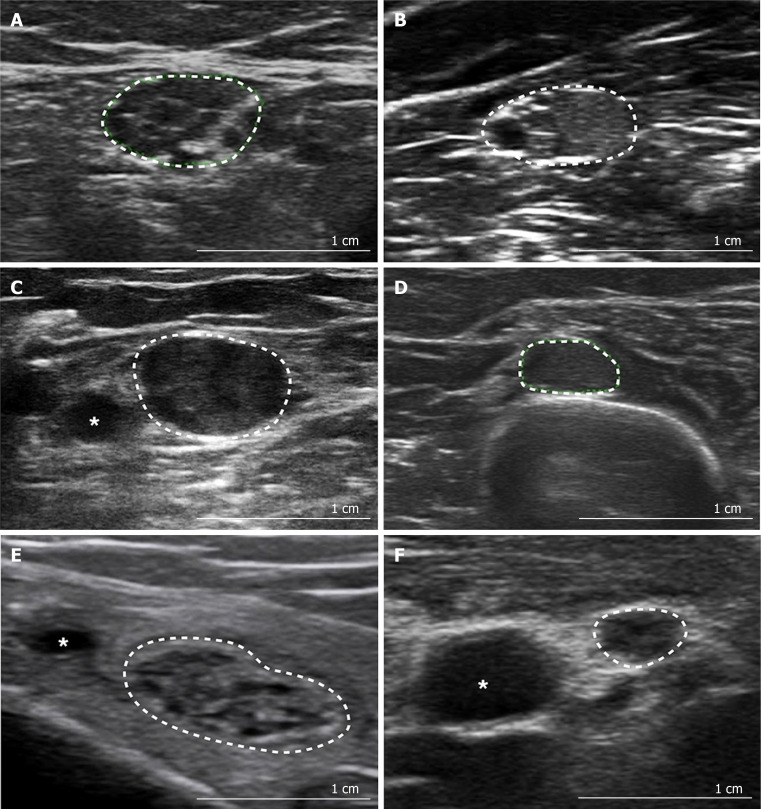
Figure 2.
Patterns of neuromuscular ultrasound in peripheral neuropathy. A: Non-homogenously enlarged, hypoechoic fascicles in Charcot Marie Tooth disease type 1A [tibial nerve at the ankle, cross-sectional area (CSA) 49 mm2]; B: Hyperechoic and hypoechoic fascicles in chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) (median nerve in the forearm, CSA 65 mm2); C: Interruption of the fascicular structure in multifocal acquired demyelinating sensory and motor neuropathy (median nerve at the elbow, CSA 91 mm2); D: Enlarged CSA, in a region normally associated with mono- or oligo-fascicular appearances, in a patient with CIDP (radial nerve at the spiral groove, CSA 27 mm2); E: Enlarged CSA, with reasonably normal fascicular architecture, due to increased perineurial connective tissue in hypertrophic neuropathy (tibial nerve at the ankle, CSA 95 mm2); F: Normal CSA with distorted fascicular architecture in amyloid neuropathy (median nerve at midpoint of the arm, CSA 8 mm2). Citation: Gallardo E, Noto Y, Simon NG. Ultrasound in the diagnosis of peripheral neuropathy: structure meets function in the neuromuscular clinic. J Neurol Neurosurg Psychiatry 2015; 86: 1066-1074. Copyright© The Authors 2020 with permission from BMJ Publishing Group Ltd.