Fig. 2.
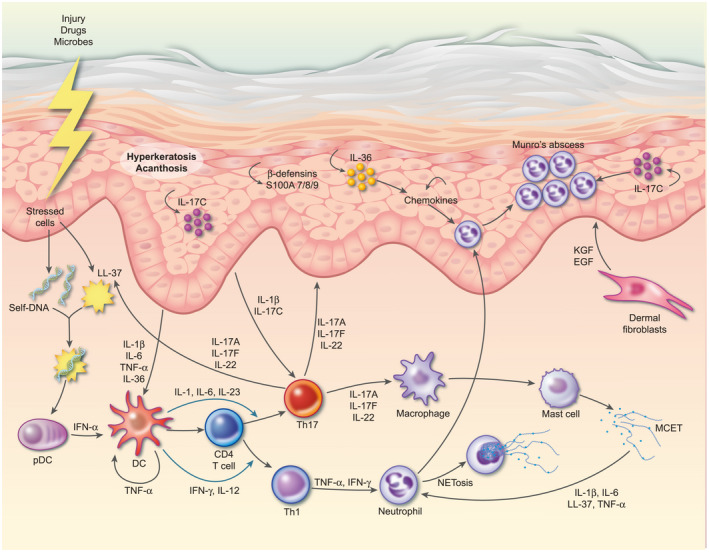
Schematic representation of psoriasis pathogenesis. Psoriasis is triggered in genetically susceptible individuals by environmental factors and/or breakdown of tolerance to self‐antigens. For example, release of self‐DNA molecules together with the anti‐microbial peptide LL‐37 activates plasmacytoid dendritic cells (pDC) to produce interferon (IFN)‐α. IFN‐α, together with tumour necrosis factor (TNF) activates myeloid DC which present self‐antigens to T cells, which then differentiate into T helper type 1 (Th1) and Th17 cells via IL‐12/IFN‐γ and IL‐23/IL‐1β/IL‐6, respectively. Th17 cells migrate to the dermis via the keratinocyte‐derived chemokines chemokine (C‐C motif) ligand 20 (CCL20) and chemokine (C‐X‐C motif) ligand (CXCL) 9/10/11, where they secrete homodimers or heterodimers of IL‐17A and IL‐17F and IL‐22. IL‐17A/F and IL‐22 bind to their receptors on both keratinocytes and fibroblasts and synergize with TNF to induce proliferation and expression of anti‐microbial peptides, such as β‐defensins and S100A7‐9, and a range of cytokines and chemokines. Chemokines such as IL‐8 and CXCL1/3/5/8 recruit neutrophils, whilst cytokines IL‐17C and IL‐36 induce further activation and proliferation of keratinocytes in an inflammatory loop. IL‐1β and TNF production by keratinocytes induces fibroblasts to release keratinocyte growth factor (KGF) and epidermal growth factor (EGF) which act back on keratinocytes, further contributing to their activation and proliferation. Meanwhile, keratinocyte‐derived IL‐1β, IL‐6 and IL‐17C feedback to further activate DC and Th17 cells.
