It has been suggested that “the most dramatic learning can come when it is a peer who is disabled, rather than a patient.” 1 The sentiment of Shakespeare, Iezzoni, and Groce are evident in innovations report by Jauregui and colleagues.2 In this invited commentary, the authors discuss how the team at The University of Washington moved beyond the legal mandates of the Americans with Disabilities Act (ADA) to capture the spirit of inclusion. We examine the benefits of training doctors and clinical researchers with disabilities and the potential impact on the health care system. We build on the work of Jauregui et al., applying their educational approach to an employment model and demonstrate, through our own case report, how these models can be scaled in clinical practice providing benefit to the medical education pipeline. We conclude with a review of the promising practices and contemplate the promise of “crowdsourcing” shared experiences toward creative approaches to the inclusion of medical students with disabilities.
The Value of Disability
There is incredible value in the message from Jauregui and colleagues. In sharing their experiences, and the multiple benefits of their model, they encourage a robust conversation about what is possible. Providers and researchers with disabilities remind us not to assume functionality or ability based solely on appearance or stereotype.3, 4 Through the article by Jauregui et al. and other first‐hand accounts there is an increased realization that the inclusion of individuals with disabilities in the biomedical workforce is valuable for health care through several mechanisms including increased empathy, increased rapport with patients, and informed care for individuals with disabilities that result in enhanced responsiveness to clinical recommendations.5, 6, 7, 8, 9, 10, 11, 12, 13
One might hypothesize that this is due, in no small part, to their experiences as a patient and a person who experienced the health care system as a consumer and provider of services. This unique lens brings a dual perspective on health care services and gives the provider insight into the barriers to navigating health care as a person with a disability. We know, for example, that many providers are not aware of the ADA, nor their responsibility for providing accessible care.14 Yet, failure to understand the law is only part of the problem. Legal mandates do not diminish stereotypes, which often fuel the assumptions about people with disabilities that lead to disparate care and health outcomes.15, 16, 17, 18, 19, 20, 21, 22, 23 Stereotypes about disability often lead to misperceptions about the ability of physicians with disabilities to practice and affect the satisfaction and quality of care received by patients with disabilities.16, 24, 25, 26, 27, 28 For example, the belief that women with physical disabilities are not sexually active leads to poorer health outcomes through attitudinal and clinical barriers, including lack of preventative services.21, 29, 30, 31, 32
Thinking about Disability Differently
Researchers and clinicians have proposed that the inclusion of physicians with disabilities would activate advanced understanding, increase empathy, reduce stereotypes of people with disabilities, improve communication, and spur technological advances for improved care.13, 27, 33, 34, 35, 36, 37, 38, 39, 40 This increased knowledge of disability may be activated through the framework of Contact Theory. Contact Theory suggests that negative attitudes and stigma stem from lack of personal and positive contact between groups.40, 41 According to Allport,40 this interaction must occur in a situation whereby the individuals maintain an equal status relationship, socioeconomic status is equalized, and members of the two groups share common goal and are working together to accomplish the same goal and where the interaction is part of the social norm. Jauregui and colleagues' approach meets all of the aforementioned criteria.
Given this, increased visibility and direct interactions with people with disabilities in health care as health professionals may significantly reduce negative stereotypes. Interactions between physicians, health care providers, and researchers with disabilities in the health care workforce might correct assumptions about disability that are critical to reducing the health care disparities caused by stigma and stereotype. If this occurs, it could create a positive outcome pathway (see Figure 1).
Figure 1.
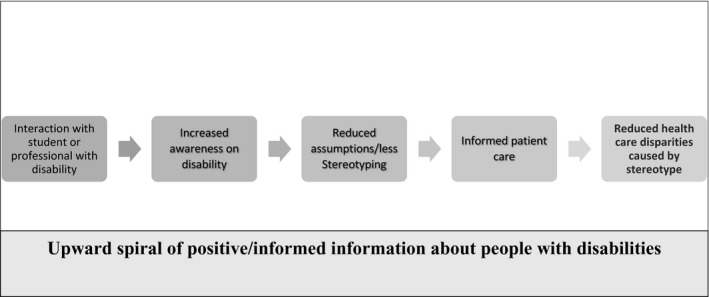
Pathway to positive outcomes.
Creative Inclusion
Medical education is becoming more inclusive, with schools revisiting their previously restricted views of what it means to be a physician with a disability. This is no doubt sparked, in part, by the increased national and international focus on disability inclusion and the sharing of personal accounts and successes by physicians, trainees, and students with disabilities.42, 43, 44, 45, 46, 47, 48, 49, 50
Jauregui and colleagues2 demonstrate the relative ease of inclusion when teams work together and are creative in their solutions for removing barriers. In this case, a student with a physical disability was faced with barriers in the environment that impacted his ability to take notes and meet standard clinical requirements. This model leveraged existing students in a creative manner that also provided educational benefits to second‐year students. An unintended, but impactful benefit of this model was the opportunity for close interaction with a person with a disability, potentially reducing stereotypes through shared experiences and peer‐to‐peer and student‐to‐faculty contact through the pathways mentioned above.
This model reduced the need for a full‐time scribe or intermediary, which resulted in significant cost savings. It also fostered a sense of community and connection, which has been shown to reduce burnout.51 The model of Jauregui and colleagues, while applied to a specific rotation, holds promise for scalability to an entire clerkship year and residency and into practice. Indeed, our own case report shows how these models can be scaled in clinical practice providing benefit to the medical education pipeline.
Case Report of Resident with Physical Disability
A gastroenterology fellow sustained a C3–C4 incomplete spinal cord injury. As a wheelchair user with limited hand function, he sought a path to practice in a nonprocedural specialty. With technological advances, such as Picture Archiving and Communications Systems (PACS), diagnostic radiology was increasingly computerized. Provided that one could meet the ACGME core competencies, and pass the licensing examinations, the essential tasks of viewing and reporting imaging examinations was within his ability.
While radiology appeared promising, the doctor would need to complete a new residency in radiology, 4 more years of training, and possibly an additional year of fellowship. The fellow matched into a residency in radiology. The program director worked closely with the him to create an environment and structure where the resident could thrive. He was not required to perform procedures, but was expected to know their indications, and contraindications, complications and to describe how to perform them. The program created a strict schedule that allowed the resident to perform necessary self‐care. In lieu of weeks of night call (night float), the resident took once weekly call from 5 PM until 10 PM. In this way, he completed approximately the same number of hours as his peers, but in a modified schedule. Finally, the resident was always on call with a second resident in the event that a procedure was required (e.g., ultrasound, place an IV, or perform a fluoroscopic procedure). The resident utilized dictation software to record impressions and was able to review the same number of images as his peers.
Cautions When Creating a Model for Inclusion
There are several cautions for creating a model that includes students as scribes and assistants. First, language is a crucial equalizer, and careful attention should be paid to the terms used to describe disability and the position (see Table 1).
Table 1.
Language/Terminology to Frame Student Positions
| Terms to Use | Term to Avoid |
|---|---|
| Student (resident/physician) with a disability or the person’s preferred terminology |
Student with special needs Student with special accommodations Student in wheelchair Handicapped student |
|
Scribe Intermediary Facilitator Volunteer |
Special Assistant Care provider Medical assistant (note, these are not medical assistants, they are merely facilitating the intellectual work of the physician) |
It is vital for attendings, preceptors, and others in positions of teaching to model respectful and inclusive behavior and to assume competence. Assuming competence is the idea that medical students are presumed to be competent to learn a skill or to provide basic care for patients. When working with a student with a disability, many faculty presume incompetence and ask or require that the individual with a disability prove their ability in advance of any instruction and in advance of the same expectations of their peer group. Faculty and administrators can model appropriate interactions with students by assuming competence and treating the student in an equivalent manner to his or her peers. Ensuring appropriate accommodations for students is also central to creating a model.
Scaling the Model of Jauregui and Colleagues
Programs may hesitate to attempt new models of inclusion at the undergraduate medical education level believing that the model is not scalable in training or practice. There is a concern that if a student graduates, he or she will face barriers in residency given the new responsibility of patient care and that the model will not be sustainable in those settings. However, the resident from our case study created a model similar to that of Jauregui et al. and is now an associate professor of radiology at an academic health system and co‐author of this paper (PP).
Working with volunteer services, the faculty member created a model that addresses his professional needs for assistance in navigating the clinic, while also meeting two growing demands: first, the need for international medical graduates to engage with medicine while they study for boards and apply for residency in the US. Through this program, international medical graduates benefit from ongoing mentoring, exposure to the U.S. medical system, assistance with the match, and potential letter of recommendation for residency. This position also affords them the opportunity to study for their board examinations, while staying connected to the hospital and medical care, keeping them engaged in the health care system. Second, this program affords an opportunity for up to 10 prehealth students to log hours shadowing for a physician, gaining exposure to radiology, and obtaining letters of recommendation. In addition to scribing, volunteers answer the telephone, help manage meals for the physician, and ensure accessible pathways. The volunteer services office chooses appropriate volunteers, maintains a formal description of the job duties, and handles all of the paperwork and training.
This model serves a need in the community for students and international graduates in the pipeline to health professions school and residency, while simultaneously serving the needs of the physician to navigate his clinical day. Similarly, to the unintended benefits experienced by Jauregui et al., this model provides multiple points of contact with a person with a disability that serve as opportunities to combat stereotype. Importantly, the contact is between the physician with a disability and the students and residents who will enter the health care field and ultimately oversee the care of patients with disabilities. Through the tenets of contact theory and the pathway for positive outcomes (Figure 1), it may be that this early contact with a high‐functioning physician with a disability reduces stereotypes and assumptions about the abilities of individuals with disabilities.
Crowdsourcing Creative Inclusion
The authors applaud Jauregui and colleagues for their innovation, commitment to supporting the student, and their commitment to sharing this case in the literature. Through this “crowdsourcing” of information (including models for accommodation), we can collectively move toward greater inclusion. The inclusion of students in medical education necessitates not only informed processes and policies, awareness of law, and a desire for diversity but also requires creative thinking and a willingness to do things differently as displayed by Jauregui and colleagues and the University of Washington. When medical educators are committed to inclusion for qualified learner, and their actions match the spirit of the ADA, the solutions are often limitless.
Conclusions
To achieve greater inclusion of persons with disabilities in medicine, creative approaches to inclusion and accommodations are needed. Jauregui and colleagues have highlighted an innovative approach to accommodations during medical training, which leverages a dynamic model that benefits students and their near peers. Additional innovative and successful examples of disability inclusion in medical settings are needed, as these approaches highlight opportunities for enhanced inclusion and the potential for medicine to shift broader societal paradigms about disability.
The authors thank Dr. Micheal McKee for his feedback on the original draft of the manuscript.
AEM Education and Training 2020;4:292–297
The authors have no relevant financial information or potential conflicts to disclose.
Author contributions: LMM, PP, BKW contributed to drafting of the manuscript, and critical revision of the manuscript for important intellectual content
A related article appears on page 275.
References
- 1. Jaregui J, Strote J, Addison C, Robins L, Shandro J. Model for a medical student with a disability during a required clinical clerkship. AEM Educ Train 2020;27:191–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Shakespeare T, Iezzoni LI, Groce NE. Disability and the training of health professionals. The Lancet 2009;374:1815–6. [DOI] [PubMed] [Google Scholar]
- 3. Gupta R. I solemnly share. JAMA 2018;319:549–50. [DOI] [PubMed] [Google Scholar]
- 4. Adashek J. Invisibly disabled. JAMA Oncol 2016;2:1265–6. [DOI] [PubMed] [Google Scholar]
- 5. Weed MA. A cure for the empathy gap? Experience and perspective of a chronically ill and disabled medical educator. Arch Ophthalmol 2012;130:263–4. [DOI] [PubMed] [Google Scholar]
- 6. Herzer KR. Moving from disability to possibility. JAMA 2016;316:1767–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Swenor B. Losing vision and gaining perspective. JAMA 2019;321:455–6. [DOI] [PubMed] [Google Scholar]
- 8. Schwarz CM, Zetkulic M. You belong in the room: addressing the underrepresentation of physicians with physical disabilities. Acad Med 2019;94:17–9. [DOI] [PubMed] [Google Scholar]
- 9. Silver JK, Bean AC, Slocum C, et al. Physician workforce disparities and patient care: a narrative review. Health Equity 2019;3:360–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Steinberg AG, Iezzoni LI, Conill A, Stineman M. Reasonable accommodations for medical faculty with disabilities. JAMA 2002;288:3147–54. [DOI] [PubMed] [Google Scholar]
- 11. Fergus KB, Teale B, Sivapragasam M, Mesina O, Stergiopoulos E. Medical students are not blank slates: positionality and curriculum interact to develop professional identity. Perspect Med Educ 2018;7:5–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Stergiopoulos E, Fernando O, Martimianakis MA. “Being on both sides”: Canadian medical students’ experiences with disability, the hidden curriculum, and professional identity construction. Acad Med 2018;93:1550–9. [DOI] [PubMed] [Google Scholar]
- 13. McKee MM, Smith S, Barnett S, Pearson TA. Commentary: what are the benefits of training deaf and hard‐of‐hearing doctors? Acad Med 2013;88:158–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Agaronnik ND, Pendo E, Campbell EG, Ressalam J, Iezzoni LI. Knowledge of practicing physicians about their legal obligations when caring for patients with disability. Health Aff 2019;38:545–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Chapman EN, Kaatz A, Carnes M. Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med 2013;28:1504–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Iezzoni LI. Eliminating health and health care disparities among the growing population of people with disabilities. Health Aff 2011;30:1947–54. [DOI] [PubMed] [Google Scholar]
- 17. Peacock G, Iezzoni LI, Harkin TR. Health care for Americans with disabilities—25 years after the ADA. N Engl J Med 2015;373:892–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Iezzoni LI, Wint AJ, Smeltzer SC, Ecker JL. “How did that happen?” Public responses to women with mobility disability during pregnancy. Disabil Health J 2015;8:380–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Iezzoni LI, Wint AJ, Smeltzer SC, Ecker JL. Effects of disability on pregnancy experiences among women with impaired mobility. Acta Obstet Gynecol Scand 2015;94:133–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Iezzoni LI, Kurtz SG, Rao SR. Trends in mammography over time for women with and without chronic disability. J Women's Health 2015;24:593–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wu J, McKee K, Meade M, McKee M, Sen A. Contraceptive use among women with vision or hearing loss: a secondary analysis of the National Survey of Family Growth, 2011–2013. Contraception 2016;94:431. [Google Scholar]
- 22. McKee MM, Winters PC, Sen A, Zazove P, Fiscella K. Emergency department utilization among deaf American Sign Language users. Disabil Health J 2015;8:573–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McDoom MM, Koppelman E, Drainoni ML. Barriers to accessible health care for Medicaid eligible people with disabilities: a comparative analysis. J Disabil Policy Stud 2014;25:154–63. [Google Scholar]
- 24. Aaberg VA. A path to greater inclusivity through understanding implicit attitudes toward disability. J Nurs Educ 2012;51:505–10. [DOI] [PubMed] [Google Scholar]
- 25. Breslin ML, Yee S. The Current State of Health Care for People with Disabilities. Washington, DC: National Council on Disability, 2009. [Google Scholar]
- 26. Breslin ML, Goode TD, Havercamp SM, Horner‐Johnson W, Iezzoni LI, Krahn G. Compounded Disparities: Health Equity at the Intersection of Disability, Race, and Ethnicity. Washington, DC: The National Academies of Sciences, Engineering, and Medicine, 2016. Available at: http://www.nationalacademies.org/hmd/~/media/Files/Activity%20Files/SelectPops/HealthDisparities/2016-JUN-14/Havercamp%20and%20Yee%20Presentation.pdf. Accessed December 16, 2019. [Google Scholar]
- 27. McKee M, Case B, Fausone M, Zazove P, Ouellette A, Fetters M. Medical schools’ willingness to accommodate medical students with sensory and physical disabilities: ethicalfoundations of a functional challenge to “organic” technical standards. AMA J Ethics 2016;18:993–1002. [DOI] [PubMed] [Google Scholar]
- 28. Meade MA, Mahmoudi E, Lee SY. The intersection of disability and healthcare disparities: a conceptual framework. Disabil Rehabil 2015;37:632–41. [DOI] [PubMed] [Google Scholar]
- 29. Signore C. Reproductive and sexual health for women with disabilities In: Miles‐Cohen SE, Signore C, editors. Eliminating Inequities for Women with Disabilities: An Agenda for Health and Wellness. Washington, DC: American Psychological Association, 2016. p. 93–113. [Google Scholar]
- 30. Mitra M, Long‐Bellil LM, Smeltzer SC, Iezzoni LI. A perinatal health framework for women with physical disabilities. Disabil Health J. 2015;8:499–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Iezzoni LI, McCarthy EP, Davis RB, Siebens H. Mobility impairments and use of screening and preventive services. Am J Public Health 2000;90:955–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lagu T, Iezzoni LI, Lindenauer PK. The axes of access—improving care for patients with disabilities. N Engl J Med 2014;370:1847–51. [DOI] [PubMed] [Google Scholar]
- 33. Iezzoni LI. Why increasing numbers of physicians with disability could improve care for patients with disability. AMA J Ethics 2016;18:1041–9 [DOI] [PubMed] [Google Scholar]
- 34. Kirschner KL, Curry RH. Educating health care professionals to care for patients with disabilities. JAMA 2009;302:1334–5. [DOI] [PubMed] [Google Scholar]
- 35. Mogensen L, Hu W. “A doctor who really knows...”: a survey of community perspectives on medical students and practitioners with disability. BMC Med Educ 2019;19:288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Meeks LM, Herzer K, Jain NR. Removing barriers and facilitating access: increasing the number of physicians with disabilities. Acad Med 2018;93:540–3. [DOI] [PubMed] [Google Scholar]
- 37. Iezzoni LI, Long‐Bellil LM. Training physicians about caring for persons with disabilities: “Nothing about us without us!”. Disabil Health J 2012;5:136–9. [DOI] [PubMed] [Google Scholar]
- 38. Swenor B, Meeks LM. Disability inclusion—moving beyond mission statements. N Engl J Med 2019;380:2089–91. [DOI] [PubMed] [Google Scholar]
- 39. Burke C. Diversity and inclusion: addressing underrepresentation of students with disabilities in health care education. J Physician Assist Educ 2019;30:61–3. [DOI] [PubMed] [Google Scholar]
- 40. Allport GW. The Nature of Prejudice. Cambridge/Reading, MA: Addison‐Wesley, 1954. [Google Scholar]
- 41. Pettigrew TF. Intergroup contact theory. Annu Rev Psychol 1998;49:65–85. [DOI] [PubMed] [Google Scholar]
- 42. Meeks LM, Liao P, Kim N. Using Twitter to promote awareness of disabilities in medicine. Med Educ 2019;53:525–6. [DOI] [PubMed] [Google Scholar]
- 43. Meeks LM, Jain N. Accessibility, Inclusion, and Action in Medical Education: Lived Experiences of Learners and Physicians With Disabilities. Washington, DC: Association of American Medical Colleges, 2018. Available at: https://store.aamc.org/accessibility-inclusion-and-action-in-medical-education-lived-experiences-of-learners-and-physicians-with-disabilities.html. Accessed December 16, 2019. [Google Scholar]
- 44. Singh SA. Medical Council of India’s new guidelines on admission of persons with specified disabilities: unfair, discriminatory and unlawful. Indian J Med Ethics 2019;4:29–34. [DOI] [PubMed] [Google Scholar]
- 45. Meeks LM. The new normal: disability inclusion in health science education. Disabil Compliance Higher Educ 2019;24:1–4. [Google Scholar]
- 46. Jain NR. Political disclosure: resisting ableism in medical education. Disabil Soc 2019;8:1–24. [Google Scholar]
- 47. Meeks LM, Herzer KR. Prevalence of self‐disclosed disability among medical students in US allopathic medical schools. JAMA 2016;316:2271–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Zazove P, Case B, Moreland C, et al. US medical schools’ compliance with the Americans with Disabilities Act: findings from a national study. Acad Med 2016;91:979–86. [DOI] [PubMed] [Google Scholar]
- 49. Kezar LB, Kirschner KL, Clinchot DM, Laird‐Metke E, Zazove P, Curry RH. Leading practices and future directions for technical standards in medical education. Acad Med 2019;94:520–7. [DOI] [PubMed] [Google Scholar]
- 50. General Medical Council . Welcome and Valued. Available at: https://www.gmc-uk.org/education/standards-guidance-and-curricula/guidance/welcomed-and-valued. Accessed December 16, 2019.
- 51. Sinsky CA, Willard‐Grace R, Schutzbank AM, Sinsky TA, Margolius D, Bodenheimer T. In search of joy in practice: a report of 23 high‐functioning primary care practices. Ann Fam Med 2013;11:272–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


