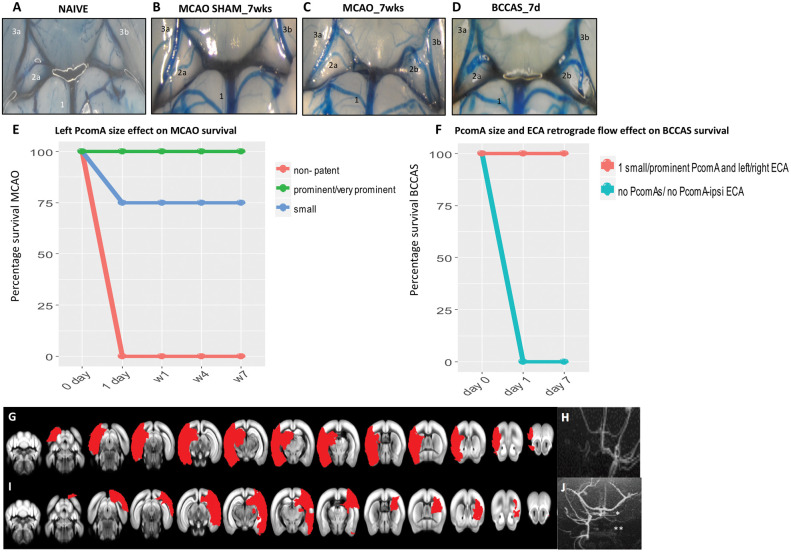
Figure 1.
PcomA and vascular phenotype effect in MCAO and BCCAS mouse models. (A–D). PcomA calibre in normal and ischemic conditions. (A) Non-patent right PcomA (2a), detected in a naïve mouse; (B) non-patent right PcomA (2a) and absence of left PcomA in MCAO sham; (C) prominent left PcomA (2b) and non-patent right PcomA (2a) in MCAO; (D) 2 prominent PcomAs in BCCAS (2a, 2b). 1, basilar artery (BA); 2a, right PcomA; 2b, left PcomA; 3a, right posterior cerebral artery (PCA); 3b, left posterior cerebral artery (PCA). The numbering of the vessels reflects the direction of the collateral blood flow following focal ischemia in the MCA or anterior brain areas: BA→PcomA→PCA, as already described in detail in the BCCAS and MCAO models in Figure S1(A) and (B). (E–F) Effect of left PcomA size and PcomA-ECA retrograde flow in MCAO and BCCAS survival. MCAO mice with non-patent left PcomA die few hours post-surgery. ≈ One-fourth of mice with small left PcomA die within one day post-surgery. The majority of MCAO mice with small left PcomA and all the MCAO with prominent/very prominent PcomA survive (E). Analogously, BCCAS mice with no PcomAs or no PcomA-no ipsilateral ECA retrograde flow die within few hours post-surgery. By contrast, BCCAS mice with at least one small to prominent PcomA and retrograde flow from left or right ECA do survive (F). (G–H) MCAO mice with non-patent left PcomA died within one day post-surgery with ischemic lesions affecting more than 35% of the left hemisphere and left PcomA and overall left blood flow were not identifiable on MRA one day post-surgery. (I–J) BCCAS with non-patent right PcomA (*) and absence of right ECA retrograde flow recruitment (**), presenting severe ischemic lesions affecting >20% of the right hemisphere.