Dear Editor,
Liang et al. report neurosensory dysfunction, such as hyposmia and hypogeusia, to be an early symptom of COVID-19 that could be used as a marker for early diagnosis (Liang et al., 2020). Data from our out-patient COVID-19 drive-through test center at the Research Center Borstel, Germany, support most of their findings. From March 19th until June 26th, 2020, we tested 1403 individuals (median age, 42 years; interquartile range, 30–54). All persons (42.6% male, 57.4% female) were tested by oropharyngeal and nasal swab for SARS-CoV-2 PCR. Tests were performed to confirm or rule out SARS-CoV-2 infection in symptomatic patients (n = 1272) as well as asymptomatic individuals (n = 131) who had been potentially exposed to SARS-CoV-2. In total, 115 persons tested positive (8.2%). Seven (6.1%) positive-test individuals were asymptomatic. Twenty one (18.2%) of positive-test patients had comorbidities.
A telephone follow-up was conducted 30 days after testing in 110 subjects with a positive swab result. The severity of disease was comparable to the cohort of Liang et al.: 106 subjects (96.3%) recovered from COVID-19 after mild disease (Liang et al.: 98.8%). While in the cohort of Liang et al. all patients were hospitalized, only four subjects (3.6%) of our group required hospital admission for severe disease. Three of them recovered (2.7%), and one person (0.9%) died. In Germany, mild cases are managed in domestic quarantine.
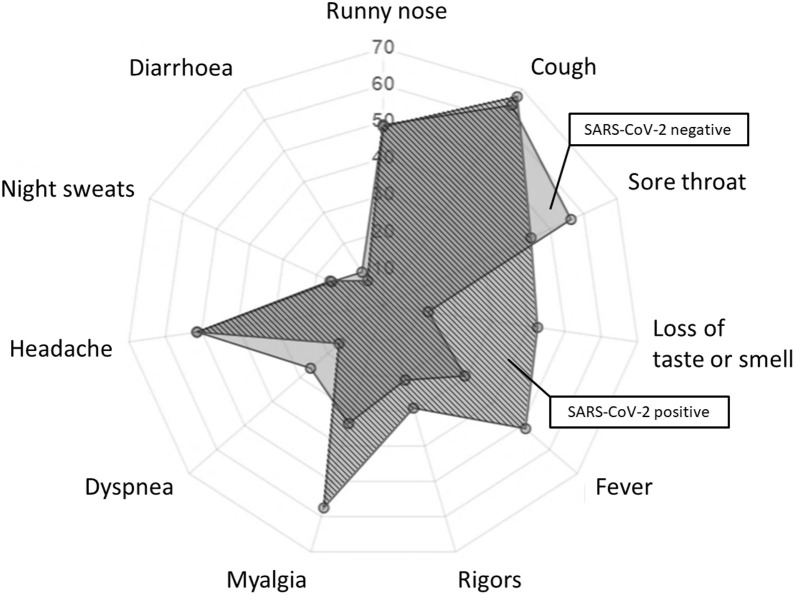
Among the presenting complaints in symptomatic patients, disturbances of taste or smell were the strongest predictors of SARS-CoV-2 infection (odds ratio, OR, 5.18; 95% confidence interval, CI, 3.43–7.79; p < 0.001) followed by myalgia (OR 2.67; 95% CI 1.81–3.97; p < 0.001). The presence of dyspnea (OR 0.53; 95% CI 0.31–0.87; p < 0.018) or a sore throat (OR 0.62; 95% CI 0.42–0.91; p < 0.0154) was associated with a negative SARS-CoV-2 test result (Figure 1 ).
Figure 1.
Frequency of symptoms in 115 patients with (dark, hatched) and 1288 patients without (monochrome light grey) SARS-CoV-2 infection in percent.
Although our cohorts are comparable in the severity of disease and frequency of neurosensory dysfunctions, we did not find that these complaints were more common in patients under 40 years (32.2% of all positive subjects) nor in women (50.4% of all positive subjects). In our 48 subjects with neurosensory dysfunction, 28 (58.3%) (OR: 0.57, 95% CI 0.27–1.22, p = 0.151) were female and 17 (42.5%) were under 40 years old (OR: 1.22, 95% CI 0.56–2.66, p = 0.620).
All data of this cohort are available online (www.covid-monitor.de). Our findings may help to better define the specificity of symptoms in the current pandemic.
Conflicts of interest
No authors report conflicts of interest.
Ethical approval
None.
Funding
The publication of this article was funded by the Open Access Fund of the Leibniz Association, Germany.
Reference
- Liang Y., Xu J., Chu M., Mai J., Lai N., Tang W., Yang T., Zhang S., Guan C., Zhong F., Yang L., Liao G. Neurosensory dysfunction: a diagnostic marker of early COVID-19. Int J Infect Dis. 2020 doi: 10.1016/j.ijid.2020.06.086. [DOI] [PMC free article] [PubMed] [Google Scholar]