Abstract
Background
Numerous studies use birth certificate data to examine the association between interpregnancy interval (IPI) and maternal and perinatal health outcomes. Substantive changes from the latest birth certificate revision have implications for examining this relationship.
Methods
We provide an overview of the National Vital Statistics System and recent changes to the national birth certificate data file, which have implications for assessing IPI and perinatal health outcomes. We describe the calculation of IPI using birth certificate information and related measurement issues. Missing IPI values by maternal age, race and education using 2016 birth certificate data were also compared. Finally, we review and summarise data quality studies of select covariate and outcome variables (sociodemographic, maternal health and health behaviours, and infant health) conducted after the most recent 2003 birth certificate revision.
Results
Substantive changes to data collection, dissemination and quality have occurred since the 2003 revision. These changes impact IPI measurement, trends and associations with perinatal health outcomes. Missing values of IPI were highest for older ages, lower education and non‐Hispanic black women. Minimal differences were found when comparing IPI using different gestational age measures. Recent data quality studies pointed to substantial variation in data quality by item and across states.
Conclusion
Future studies examining the association of IPI with maternal and perinatal data using vital records should consider these aspects of the data in their research plan, sensitivity analyses and interpretation of findings.
Keywords: birth certificate, birth spacing, interpregnancy interval, vital statistics
1. INTRODUCTION
The collection of vital statistics information is a foundation of our public health infrastructure. The measurement of livebirth intervals, or the time between a previous and current birth, has been based on information collected on U.S. birth certificates since 1968.1 Since that time, birth certificate data have been used to examine the association between birth or interpregnancy intervals (IPI), commonly defined as the interval between a livebirth and start of the next pregnancy, and maternal and infant health. Numerous studies using vital statistics data have shown a relationship between both short and long IPI and birth outcomes (14 out of 32 studies used vital records in a recent systematic review).2 While some studies have linked birth certificate records by maternal identifiers prospectively over time, most are cross‐sectional. Recently, the causal association of short IPI on birth and infant health outcomes has been questioned,3, 4, 5, 6 prompting a discussion of whether we need to move beyond cross‐sectional designs.
Other manuscripts in this supplemental issue address the strengths and weaknesses of these causal approaches for directly addressing this question. While there are inherent limitations with vital records data, they are useful for supporting hypothesis‐generating research. In fact, part of the motivation underlying this broader question stems from earlier studies using vital records data. Recent changes to the birth certificate provide new information for evaluating IPI; however, these changes also have implications for analysis and interpretation of findings.
Therefore, the objective of this study was to provide essential background on vital records data to aid in the analysis and interpretation of studies examining IPI using these data. We provide an overview of the National Vital Statistics System (NVSS) and birth certificate data collection, describe recent changes to address data quality and review the measurement and quality of data items to assess IPI and select pregnancy, birth and infant health outcomes. We conclude with recommendations for strengthening inferences from vital records.
2. THE NATIONAL VITAL STATISTICS SYSTEM: BIRTH CERTIFICATE DATA
The NVSS provides official data for reporting of birth and death statistics in the United States and is comprised of 57 vital registration areas (50 states, New York City, D.C., and 5 U.S. territories).1 Each vital registration area is independently responsible for collecting their own vital statistics data. While federal law does not require collection of vital statistics, all states mandate the recording of vital events. Under the Health Services Research and Evaluation and Health Statistics Act of 1974 (Public Health Law 93‐353), the National Center for Health Statistics (NCHS) is directed to compile, produce and disseminate national vital records data.
Uniformity in data collection and processing is achieved through U.S. Standard Certificates and Reports and through the Vital Statistics Cooperative Program (VSCP).1 The VSCP is a federal‐state partnership that has facilitated the production of national vital statistics data under the auspices of NCHS since 1973. Contracts through the VSCP provide funding support to vital registration areas and facilitate standardised data collection and improvement efforts. Since the 1990s, a focus of these contracts has been on automating data collection, improving timeliness and data quality, and enhancing data products.
Perinatal health data for the United States are derived from the birth certificate and foetal death report. In addition, NCHS produces infant mortality data files which are based on linking data for infant deaths (occurring in the first year of life) to the corresponding birth certificate.7 This linkage has been a component of the VSCP since the 1987 birth cohort.1 These data sources are used to monitor progress towards meeting health goals (e.g, Healthy People 2020)8 and facilitate national, state and local planning and development efforts. The items on the birth certificate generally represent the core set of items included on all 3 perinatal data files. Thus, we focus the remainder of this manuscript on the U.S. Standard Certificate of Live Birth. We note that the foetal death file includes substantially fewer data items, largely reflecting concerns about incomplete reporting and data quality.1
National birth certificate data are transmitted by states to NCHS and then compiled and disseminated for public use after removing identifiable information. The major advantage of birth certificate data is representativeness with 100% of all registered births each year (approximately 4 million per year). Annual data collection facilitates comparisons over time. The large size ensures sufficient numbers to examine more detailed subgroups, geographic units and rare outcomes. A main public health function of this data is population‐based monitoring of maternal and infant health outcomes, rather than clinical research. Therefore, caution is needed to not over‐interpret the data as clinical findings.9, 10 While key sociodemographic characteristics are collected (e.g, parental age, race, Hispanic origin and education), information on other potential confounders (e.g, income or prior pregnancy health) is limited. Finally, hospitals and states vary considerably in their vital records data collection processes and data quality, with substantial under‐reporting for some medical and health items (discussed in greater detail below).
3. 2003 U.S. STANDARD CERTIFICATE OF LIVE BIRTH REVISION
The birth certificate has been revised 11 times (12 versions in total) since its inception in 1900.1 The changes made between the 1989 and the most recent 2003 U.S. Standard Certificate of Live Birth (Appendix S1) have far exceeded those of previous revisions.11 We summarise the most pertinent changes from this latest revision. An outline of birth certificate data item changes over time is provided in Appendix S2 and reviewed elsewhere.1, 12 Most notably, several items were added to the 2003 revision to enhance the sociodemographic and health information provided, including but not limited to source of payment for delivery, Women, Infant, and Children supplemental food programme (WIC) use during pregnancy, paternity acknowledgement at the time of birth, pre‐pregnancy body mass index (BMI), pre‐pregnancy smoking, pre‐pregnancy hypertension and diabetes, maternal morbidities and neonatal intensive care unit (NICU) admission.11 Additionally, modifications were made to existing items, some of which made the data non‐comparable to data based on the 1989 birth certificate, compromising trend analysis. These non‐comparable data items included parental education, smoking during pregnancy, prenatal care, previous Caesarean delivery and previous preterm birth (see Appendix S3 for a more detailed list of comparable, non‐comparable and new data items for the 2003 revision).13
In addition to revised data items, a main focus of the 2003 revision was to improve the data collection process. This included the development of standardised worksheets for the mother and birth facility and a comprehensive guidebook that included detailed definitions, instructions and preferred data sources.12, 14 Information collected from the mother on the maternal worksheet included demographics, WIC use during pregnancy, smoking during pregnancy and pre‐pregnancy weight and height for calculating BMI. All other medical and health information is recommended to be collected from medical records using the facility worksheet.
Vital registration areas were also encouraged to switch to an automated, electronic data collection system with real‐time edit checks.15 These modifications were instituted to facilitate more timely and accurate data collection; however, this shift led to unprecedented delays in the adoption of the 2003 revised birth certificate by vital registration areas. The delay was primarily due to budget shortfalls at the state and national level and the need for states to update their registration systems. Figure 1 provides a timeline for the phased implementation of the 2003 revision for the United States.16
Figure 1.
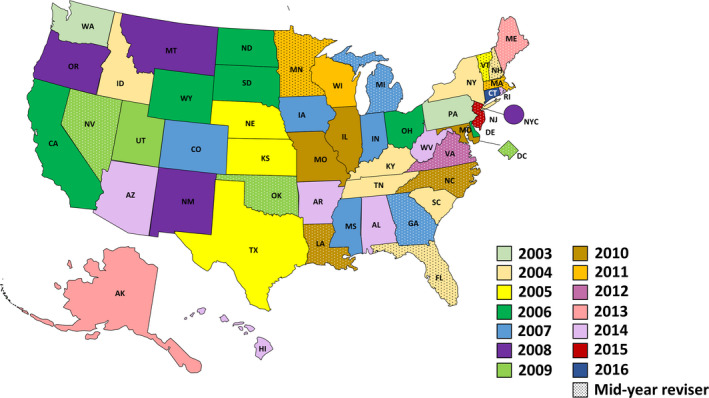
Timeline of the phased implementation of the 2003 revision for the United States
A significant implication of the delayed implementation was a lack of national data from 2003 to 2015 for certain data items. New or modified data items were only reported from the states that had revised the birth certificate by a given data year. The selection of states that had revised by a given year could not be considered representative of the United States as a whole, as illustrated in Figure 2 for a key demographic (Hispanic origin) and key health (preterm birth) variable. In addition, the revised states changed from year to year, limiting trend analyses. Because of these limitations, all revised items were not released on national data files until data year 2009, representing 66% of all U.S. births.17 In 2016, 50 states and D.C. had implemented the 2003 revisions, providing national data on all revised items.18
Figure 2.
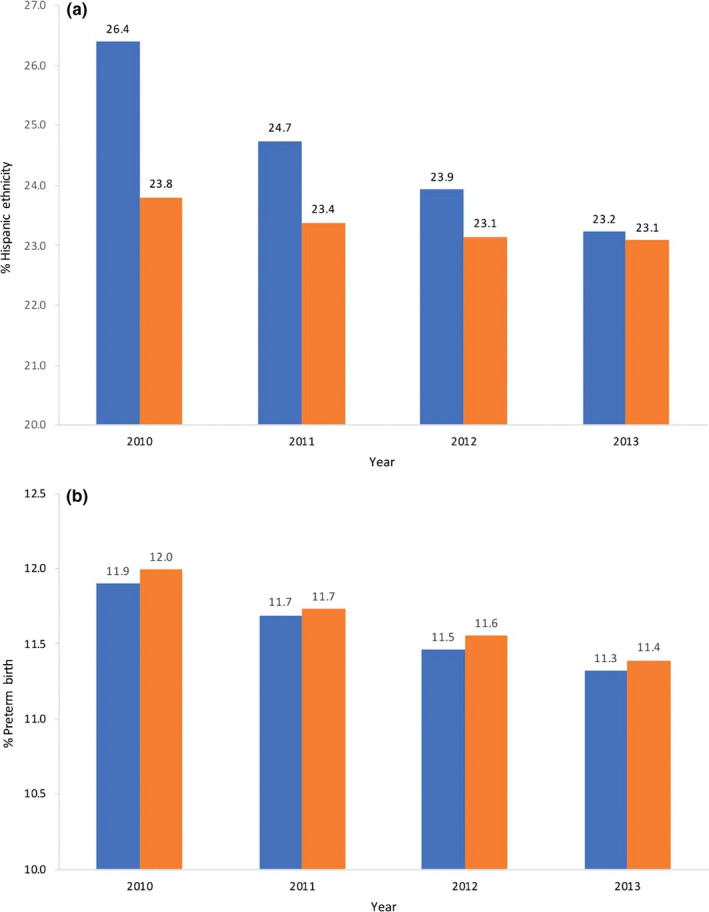
Comparison of the representativeness of select items from revised states (blue) versus the United States overall (orange), 2010‐2013. A, Per cent reporting Hispanic ethnicity. B, Preterm birth rates. Information is available in Table D of the User Guide to the Natality Public Use file for each corresponding year (www.cdc.gov/nchs/data_access/vitalstatisticsonline.htm)
4. RECENT INITIATIVES TO IMPROVE BIRTH CERTIFICATE DATA QUALITY
As vital registration areas moved towards adopting the 2003 birth certificate, NCHS and state vital records agencies turned their attention to evaluating and improving the quality of birth data. One important initiative was a validation study of several medical and health items from the 2003 revised birth certificate compared to medical records conducted in two states.19 Findings from this study along with more recent validation studies using the 2003 birth certificate are discussed in greater detail below. Additionally, NCHS conducted several studies to assess the comparability of items on the birth certificate to other national data sources, including source of payment at delivery,20 births resulting from assisted reproductive technologies21 and IPI.22
A number of efforts have been completed or are underway at NCHS to address the quality of vital statistics data.1 While these endeavours are too exhaustive to discuss in detail in this review, we highlight a few initiatives that have current and future implications for data users. In 2014 and 2015, several items that were considered poor data quality were cut from the national birth and foetal death data files.23 The rationale for these cuts was to focus on data items that could be collected with reasonable accuracy or had the potential for improvement. These changes along with improved instructions and definitions for data collection were updated in the “Guide to Completing the Facility Worksheet for the Certificate of Live Birth and Report of Fetal Death.”14 Improvements to the guide were based on interviews and inquiries from hospital staff on particular data items and the ongoing reVITALize initiative, which aims to develop standardised obstetric definitions for perinatal and women's health records.24
Finally, nationally accredited e‐learning training for clinical and non‐clinical hospital staff in completing medical and health data for birth certificates and foetal deaths was developed to improve the quality of information collected at the hospital level.25 A small study among nurses suggests improvement in knowledge of birth data collection after receipt of this new online training tool.26 Additional efforts to promote this training within hospitals and evaluate its effectiveness are currently underway.
Despite these efforts, the quality of vital statistics data is dependent upon the data collection processes in hospitals and states. The training of birth registrars, dissemination of new training tools and quality control rely primarily on the efforts of state vital statistics offices, impacting the variability and quality of reporting data items.27, 28 We therefore focus the next sections of this manuscript on the measurement and quality of information to assess IPI and select perinatal health outcomes, which have implications for assessing exposure‐outcome relationships.
5. MEASUREMENT OF INTERPREGNANCY INTERVAL ON THE BIRTH CERTIFICATE
5.1. Definition and measurement
Interpregnancy interval is commonly defined from a livebirth to the start of a subsequent pregnancy.8 The basis for beginning the interval at the start of a livebirth is, in part, due to the proposed causal mechanism for why IPI may influence maternal and infant health outcomes, which relates back to the physiological effects of delivering a baby and postpartum transition following a livebirth.29, 30 One point of differentiation in IPI definitions is how the subsequent pregnancy ended. Healthy People 2020 Family Planning objective 5, “Reduce the proportion of pregnancies conceived within 18 months of a previous birth,” assesses the time from a livebirth to a subsequent pregnancy, regardless of outcome (i.e, the pregnancy could have ended in pregnancy loss, abortion or livebirth).8 Most studies using birth certificate data define IPI more specifically as the time between a livebirth and the start of a subsequent pregnancy that ended in a livebirth.
These distinctions are important when comparing IPI measures across different population‐based data sources, as intervening pregnancy losses may be accounted for differently. Information on intervening pregnancy losses can be determined by the “Date of Last Other Pregnancy Outcome (spontaneous or induced losses or ectopic pregnancies)” on the birth certificate; however, this information has been shown to have a high amount of missing data and documented poor data quality.19 While these distinctions may impact prevalence, a recent study showed this may be less of a concern for researchers interested in the effects of IPI on subsequent livebirth outcomes (e.g, preterm birth), regardless of intervening losses.31
The calculation of IPI on the birth certificate relies on three data items—”The Date of last live birth,” “The Date of [current] Birth” and the “Obstetric estimate of gestation.” A livebirth interval is available as a recode on the national public‐use data file and is computed by subtracting the date of last livebirth from the date of the current birth (converted to months) (Figure 3).
Figure 3.
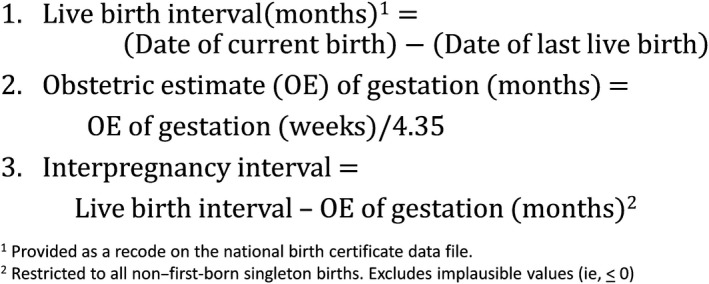
Steps for calculating the interpregnancy interval (IPI) using three data items on the birth certificate
The obstetric estimate of gestation is converted from weeks to months. Finally, IPI is calculated by subtracting the gestational age of the current birth (in months) from the livebirth interval. Because plural births may include information from the same pregnancy and not the prior pregnancy, the calculation of IPI is restricted to all non‐first‐born singleton births. Implausible values (i.e, ≤0 months) resulting from negative values after calculation are also excluded. A recent study found that estimates of IPI < 18 months using the 2011 birth certificate (29.6%) were comparable with the 2006‐2010 NSFG data (29.3%) when applying the same IPI definition.22
5.2. Data collection and quality
The birth certificate data items used to construct IPI have relevant historical context for interpreting IPI measures over time. The date of last livebirth has been included on the birth certificate since 1968.1 Due to resource constraints at the state and Federal levels, the collection of this information from vital registration areas was discontinued and no longer included on the national birth certificate data file after 1993.32 The collection of this data item was restored with the 2003 revision, and the birth certificate data on livebirth intervals is now available from 2009 onward.22, 33 Current NCHS guidelines recommend collecting this information from the prenatal care record, rather than maternal self‐report.14 An evaluation of the quality of the date (month) of last livebirth data item after the 2003 revision showed substantial to high (κ ≥ 75%) agreement when compared with medical records.19
Changes to the gestational age measure on the birth certificate could also impact IPI comparisons over time. From 1981 to 2014, the official measure of gestational age was based on the difference between the current date of birth and the mother's last menstrual period (LMP).34 In 2014, this changed to the obstetric estimate (OE) of gestation, which is defined as “the best estimate of the infant's gestation in completed weeks based on the birth attendant's final estimate of gestation.”14 The change was driven by many factors, including greater validity of the OE of gestational age compared with the LMP‐based measure and national availability of the OE of gestation.
The completeness and accuracy of these two data items impact IPI measurement. As such, we compared missing IPI values overall and across demographic characteristics using 2016 birth certificate data restricted to all non‐first‐born, singleton resident births. Missing values were relatively high for IPI (5.9%) compared with other data items. The majority of missing data was due to missing information on the livebirth interval (5.6%), rather than gestational age (1.13%) or implausible values (i.e, IPI ≤ 0 months) (0.23%) (not mutually exclusive). Births of mothers who were older, non‐Hispanic black and had lower educational attainment were more likely to be missing a value for IPI (Figure 4). Additionally, we compared IPI calculations based on the OE of gestation compared to the LMP‐based estimate of gestation. We found minimal differences between short IPI calculated using the obstetric estimate of gestation (IPI < 18 months: 29.3%) compared to the LMP‐based estimate (29.5%). Agreement between the two measures was 99.78%. Of the 0.22% that were discordant, 0.08% were classified as <18 months by OE and ≥18 months by LMP, whereas 0.14% were classified as <18 months by LMP and ≥18 months by OE. These comparisons are only for data year 2016 and may vary over time as well as by demographic and health characteristics.
Figure 4.
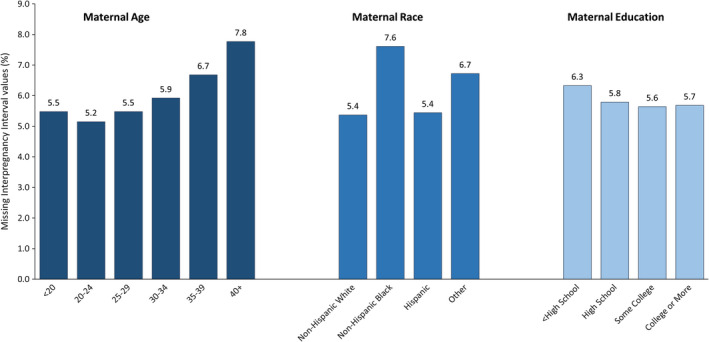
Per cent distribution of missing interpregnancy interval (IPI) information by categories of maternal age, race and education
6. DATA QUALITY OF SELECT MATERNAL AND INFANT HEALTH ITEMS ON THE BIRTH CERTIFICATE
The question of whether IPI influences maternal and infant health not only relies on accurate IPI measurement, but also on the accuracy and reliability of information on health outcomes and potential confounders. A review of data quality studies based on the 1989 U.S. Standard Certificate of Live Birth found that several of the medical and health items were under‐reported and that missing values varied systematically on the birth certificate.35 In contrast, the quality of sociodemographic information was generally well reported (e.g, agreement of 80% or greater for maternal age, race and plurality). Since the 1989 standard birth certificate, however, a number of initiatives have been established to improve data collection and quality with the 2003 revision. In this section, we summarise findings from studies evaluating the quality of select data items from the 2003 revision.
We conducted a literature search of validity and reliability studies of selected sociodemographic and medical and health items from the birth certificate. The items selected were based on covariate and outcome variables that have been examined or may be of interest in relation to IPI. Details of the literature search protocol and inclusion criteria are provided in Appendix S4. In brief, we combined search terms of “birth certificate” AND “valid*,” “reliab*,” “accuracy,” OR “data quality” AND “United States OR US” to identify studies. Studies using the 1989 birth certificate were excluded. Validity was assessed using sensitivity (Se). Specificity was recorded; however, not all studies provide estimates of specificity. Of those that did, all were found to have high specificity (>80%) and, therefore, did not contribute to variability in data quality across data items. Reliability was assessed using kappa statistics. When kappa values were unavailable, we used per cent agreement (PA).
Data comparison sources included medical records or biomarker information, maternal self‐report, linked birth certificates, hospital discharge data, health discharge data and Pregnancy Risk Assessment Monitoring System (PRAMS) data. Data quality rankings were based on the overall summary measures and classified as “High,” “Moderate” or “Low” accuracy or agreement with other data sources. A sensitivity between 80.0% to 100%, 60.0% to 79.9% and <60.0%, or per cent agreement or a κ between 0.80 to 1.00, 0.60 to 0.79 and <0.60 was ranked as high, moderate or low, respectively.35 In cases where validity or reliability measures were stratified by state or subgroup, a range of estimates was presented. Items were also classified as “unknown” if the quality of the specific data item was not evaluated after the 2003 revision. Table 1 presents findings from the literature review organised by type of variable on the birth certificate. We summarise our findings for sociodemographic information, maternal health outcomes (divided into sub‐sections of pre‐pregnancy and pregnancy health behaviours, pregnancy risk factors, and labour and delivery) and infant health outcomes.
Table 1.
Data quality measures and rankings for select variables on the 2003 revised national birth certificate data file
| Variables (recommended worksheet)a | Data quality rankingb | Data quality measures | Data comparison source (study population) | Referencesref# | |||
|---|---|---|---|---|---|---|---|
| High | Mod | Low | Unk | ||||
| Sociodemographic characteristics | |||||||
| WIC use during pregnancyc (maternal worksheet) | X |
Se = 90.8%; Sp = 90.6% κ = 0.81 |
2008 PRAMS (12 states) | Ahluwalia 201338 | |||
|
Source of payment at delivery (facility worksheet) Medicaidc |
X | X |
Se = 72.6% (B), 79.0% (A) κ = 0.70 (A and B) |
Medical records (States A and B) | Martin 201319 | ||
|
Se = 86.3%; Sp = 81.9% κ = 0.78 |
Medicaid claims (Iowa) | Kane 201340 | |||||
| Se = 82.4%; Sp = 85.6% | 2008 PRAMS (12 states) | Ahluwalia 201338 | |||||
|
Se = 93.2% (NYC), 97.8% (VT) Sp = 86.7% (NYC), 94.7% (VT) |
Medical records (NYC, VT) | Dietz 201539 | |||||
|
Source of payment at delivery (facility worksheet) Private Insurancec |
X | X |
Se = 82.3% (A), 85.8% (B) κ = 0.65 (A), 0.83 (B) |
Medical records (States A and B) | Martin 201319 | ||
|
Se = 86.7% (NYC), 94.7% (VT) Sp = 93.2% (NYC), 97.8% (VT) |
Medical records (NYC, VT) | Dietz 201539 | |||||
| Maternal aged (maternal worksheet) | X | ||||||
| Maternal race and Hispanic origind (maternal worksheet) | X | ||||||
| Maternal educatione (maternal worksheet) | X | ||||||
| Maternal health: pre‐pregnancy health/pregnancy behaviours | |||||||
| Pre‐pregnancy smokingc (maternal worksheet) | X | X | κ = 0.68 | 2008 PRAMS (8 states) | Tong 201346 | ||
|
κ (worksheet) = 0.92 κ (medical records) = 0.70 |
Maternal worksheet/medical records (NYC, VT) | Howland 201545 | |||||
| Smoking during pregnancye (maternal worksheet) | X | X | κ = 0.75 | 2008 PRAMS (8 states) | Tong 201346 | ||
| Se = 85% and 89% (self‐reported non‐smokers and smokers, respectively) | Newborn blood spot cotinine levels (WA) | Nielsen 201447 | |||||
|
κ (worksheet) = 0.89 κ (medical records) = 0.74 |
Maternal worksheet/medical records (NYC, VT combined) | Howland 201545 | |||||
| Pre‐pregnancy BMIc (maternal worksheet) | X | X | X | Se = 61.1%‐86.0%; Sp = 82.4%‐97.5% (underweight to obese) | Directly measured Values from WIC (Florida) | Park 201148 | |
| PA = 51.7%‐100% (underweight to obese, stratified by select subgroups) | Medical record (Pennsylvania) | Bodnar 201449 | |||||
| Prenatal care initiation (first trimester)e (facility worksheet) | X | PA = 83.0 (A), 89.5 (B) | Medical records (States A and B) | Martin 201319 | |||
| Total number of PNC visitse (facility worksheet) | X | PA = 47.8 (A), 22.1 (B) | Medical records (States A and B) | Martin 201319 | |||
| Within 2 visits | X | X | PA = 84.3 (A), 65.0 (B) | Medical records (States A and B) | Martin 201319 | ||
| Maternal health: pregnancy risk factors | |||||||
| Any diabetesd | X |
Se = 68.0% (NYC), 78.9% (VT) Sp = 99.6% (NYC), 99.6% (VT) |
Medical records (NYC, VT) | Dietz 201539 | |||
| Pre‐pregnancy diabetese (facility worksheet) | X |
Se = 52.0%; Sp = 99.0% κ = 0.57 |
Medical records (Florida) | Clayton 201351 | |||
| Gestational diabetese (facility worksheet) | X | X | κ = 0.53 | 2004‐2006 PRAMS (New York State) | Hosler 200952 | ||
|
Se = 57.7% (A), 58.6% (B) κ = 0.55 (A), 0.68 (B) |
Medical records (States A and B) | Martin 201319 | |||||
|
Se = 42.0%; Sp = 98.0% κ = 0.49 |
Medical records (Florida) | Clayton 201351 | |||||
|
Se = 70.3% (NYC), 75.7% (VT) Sp = 99.6% (NYC), 99.5% (VT) |
Medical records (NYC, VT) | Dietz 201539 | |||||
| Any hypertensiond | X | X |
Se = 38.7% (NYC), 75.5% (VT) Sp = 99.4% (NYC), 99.3% (VT) |
Medical records (NYC, VT) | Dietz 201539 | ||
| Pre‐pregnancy hypertensiond (facility worksheet) | X |
Se = 39.4% (A) κ = 0.50 (A) |
Medical records (State A) | Martin 201319 | |||
|
Se = 17.0%; Sp = 99.0% κ = 0.24 |
Medical records (Florida) | Clayton 201351 | |||||
| Gestational hypertensiond (facility worksheet) | X | X |
Se = 50.0% (A), 20.0% (B) κ = 0.50 (A), 0.24 (B) |
Medical records (States A and B) | Martin 201319 | ||
|
Se = 52.0%; Sp = 92.0% κ = 0.48 |
Medical records (Florida) | Clayton 201351 | |||||
|
Se = 33.4% (NYC), 75.5% (VT) Sp = 99.5% (NYC), 99.4% (VT) |
Medical records (NYC, VT) | Dietz 201539 | |||||
| Eclampsiad (facility worksheet) | X | ||||||
| Previous Caesarean deliverye (facility worksheet) | X | X |
Se = 82.1% (A), 62.5% (B) κ = 0.88 (A), 0.72 (B) |
Medical records (States A and B) | Martin 201319 | ||
|
Se = 63.3% (NYC), 91.0% (VT) Sp = 99.7% (NYC), 99.8% (VT) |
Medical records (NYC, VT) | Dietz 201539 | |||||
| Previous preterm birthe (facility worksheet) | X | X | Se = 65.5% | Linked birth certificates (Upstate NY) | Hackney 201254 | ||
|
Se = 22.0% (A), 20.6% (B) κ = 0.29 (A), 0.31 (B) |
Medical Records (States A and B) | Martin 201319 | |||||
| Maternal health: labour and delivery | |||||||
| Final route of delivery—Caesareand (facility Worksheet) | X |
Se = 97.9% (A), 91.8% (B) κ = 0.97 (A), 0.93 (B) |
Medical records (States A and B) | Martin 201319 | |||
|
Se = 97.2% (NYC), 99.4% (VT) Sp = 100.0% (NYC), 99.7% (VT) |
Medical records (NYC, VT) | Dietz 201539 | |||||
| Maternal morbidities: ICU admissionc (facility worksheet) | X | Se = 20.0% | Hospital discharge data (MA) | Luke 201855 | |||
| Maternal morbidities: blood transfusionc (facility worksheet) | X | Se = 12.0% | Hospital discharge data (MA) | Luke 201855 | |||
| Maternal morbidities: uterine rupturec (facility worksheet) | X | Se = 26.0% | Hospital discharge data (MA) | Luke 201855 | |||
| Infant health outcomes | |||||||
| Birthweightd (facility worksheet) | X |
Low birthweight: PA = 95.7%, 100% (B) |
Medical records (States A and B) | Martin 201319 | |||
| Gestational age based on OE of gestationd (Facility Worksheet) | X | X |
Preterm birth: PA = 95.3% (A), 72.5% (B) |
Medical records (States A and B) | Martin 201319 | ||
| Se = 74.9% | Medical records/ultrasound (CA) | Barradas 201357 | |||||
|
Se = 82.5% (NYC), 93.8% (VT) Sp = 99.8% (NYC), 100% (VT) |
Medical records/EDD (NYC, VT) | Dietz 201556 | |||||
| Gestational age based on last menstrual periodd | X | X |
Preterm birth: PA = 94.8% (A), 72.1% (B) |
Medical records (States A and B) | Martin 201319 | ||
| NICU admissionc (facility worksheet) | X | X |
Se = 95.1% (A), 45.1% (B) κ = 0.90 (A), 0.57 (B) |
Medical records (States A and B) | Martin 201319 | ||
| Apgar score (5‐min)d (facility worksheet) | X | ||||||
BMI, body mass index; CA, California; EDD, Estimated Date of Delivery; ICU, intensive care unit; MA, Massachusetts; Mod, Moderate; NY, New York; NYC, New York City; OE, obstetric estimate; PA, per cent agreement; PNC, prenatal care; PRAMS, Pregnancy Risk Assessment Monitoring System; Se, Sensitivity; Sp, Specificity; Unk, Unknown for 2003 birth certificate; VT, Vermont; WA, Washington; WIC, Women, Infant, and Children Supplemental Food program.
Recommended worksheet for collection of birth certificate information at the birthing facility. The maternal worksheet collects information from the mother at the time of birth. The facility worksheet collects information from medical records.
Data quality ranking based on kappa (agreement between birth certificate and data comparison source for a given condition or characteristic accounting for chance agreement), sensitivity (percentage of births with a given condition or characteristic on the birth certificate among births with the given condition or characteristic on the data comparison source) or per cent agreement (agreement between birth certificate and data comparison source). κ: High = 0.80‐1.00; Moderate = 0.60‐0.79; Low < 0.60; Sensitivity: High = 80.0%‐100%, Moderate = 60.0%‐79.9%, Low < 60%; PA: High = 80.0%‐100%, Moderate = 60.0%‐79.9%, Low < 60%.
New data item introduced with the 2003 U.S. birth certificate revision.
Data items are comparable between the 2003 and 1989 U.S. Standard Certificates of Live Birth. While some data items may have been modified, the information is still considered comparable across revisions. Additional considerations include the following: (a)multiple‐race data are bridged to the single race categories of the 1977 OMB standards for comparability with other states, (b) pre‐pregnancy and gestational diabetes may be combined to be consistent with the Diabetes item reported on the 1989 U.S. Standard Certificate of Live Birth, and (c) the “obstetric estimate of gestation” item on the 2003 revised standard birth certificate is comparable to the “clinical estimate of gestation” on the 1989 standard birth certificate.
Data items modified with the 2003 U.S. birth certificate revision, considered non‐comparable with the 1989 birth certificate item. All items not referenced in Table 1 as new or non‐comparable can be considered comparable to the 1989 certificate.
6.1. Sociodemographic information
Sociodemographic information is most often self‐reported by the mother on the maternal worksheet. Data quality studies on maternal age, race and education after the 2003 revision were not found; however, earlier comparisons of this information to medical records showed high‐quality data (i.e, sensitivity >90% or κ > 0.85).36, 37 Because the maternal education item was modified with the 2003 revision, future studies should evaluate the quality of this data item.
Two new data items, WIC use during pregnancy and source of payment at delivery, provide additional proxy information on socio‐economic status. WIC use during pregnancy is also recommended to be self‐reported by the mother and found to have high accuracy (Se 90.8%) and reliability (κ 0.81) with PRAMS data.38 Source of payment at delivery (e.g, Medicaid, private insurance), which is collected on the facility worksheet, was ranked as moderate or high data quality when compared with medical records (Se 72.6%‐97.8%; κ 0.65‐0.83);19, 39, 40 however, birth registrars have documented that the reporting of this information is not always straightforward.41, 42, 43, 44
6.2. Pre‐pregnancy and pregnancy health behaviours
Most of the pre‐pregnancy and pregnancy health behaviour items were new or modified in 2003 and ranked as having moderate or high data quality. High‐quality data were found in at least one study across each of these items, suggesting that this information can be collected with reasonable accuracy. Unlike the other variables in this category, pre‐pregnancy (i.e, 3 months before pregnancy) smoking and prenatal smoking are recommended to be collected from the mother. Pre‐pregnancy smoking was found to have moderate‐to‐high level of agreement with the maternal worksheet or other self‐reported data (κ 0.68‐0.92).45, 46 Prenatal smoking also showed moderate‐to‐high agreement when compared to other self‐reported information from PRAMS (κ 0.75) or maternal worksheet (κ 0.89) and slightly less agreement when compared with medical records (κ 0.74). While slightly under‐reported, prenatal smoking on the birth certificate had a high sensitivity when compared with biomarkers of newborn cotinine (Se 85.0%‐89.0%).47
The quality of data on pre‐pregnancy weight and height used to calculate BMI varied from low to high quality (PA 51.7%‐100%; Se 61.1%‐86.0%). While BMI was generally found to be under‐reported on the birth certificate, one study concluded that it was still a reliable measure for surveillance and research.48 In contrast, a study by Bodnar et al49 cautioned against the use of this variable, particularly at extreme BMI classifications.
Prenatal care items on the birth certificate depended on the specificity of the information evaluated. Martin et al found that receipt of prenatal care during the first trimester had a high level of agreement (PA 83.0%‐89.5%); however, the exact number of prenatal care visits was reported less reliably (PA 22.1%‐47.8%).19 When the number of visits was assessed within ±2 visits, there was much higher agreement (PA 65.0%‐84.3%), suggesting that general indicators of prenatal care on the birth certificate are reasonably reported.
6.3. Pregnancy risk factors
Previous studies using the 1989 birth certificate have shown pregnancy risk factors are often under‐reported.50 Modifications on the 2003 revision to diabetes during pregnancy required greater specificity (i.e, pre‐pregnancy and gestational), but limited improvement in data quality. Combined, information on diabetes during pregnancy is comparable to the 1989 birth certificate and was shown to be moderately accurate when compared with medical records (Se 68.0%‐78.9%).39 When partitioned, the quality of these data items was low for pre‐pregnancy diabetes (Se 52.0%; κ 0.57) and low to moderate for gestational diabetes (Se 42.0%‐75.7%; κ 0.49‐0.68).19, 39, 51, 52 Similarly, data quality was low for pre‐pregnancy hypertension (Se 17.0%‐39.4%; κ 0.24‐0.50) and low to moderate for gestational hypertension (Se 20.0%‐75.5%; κ 0.24‐0.48).19, 39, 51 For both diabetes and hypertension, there was significant variation in reporting depending on the item and vital registration area examined. For example, the sensitivity of gestational diabetes in New York City and Vermont was 70.3% and 75.7%, whereas gestational hypertension was 33.4% and 75.5%, respectively.39 Thus, the generalisability of these findings for national data is unclear. Eclampsia is a separate data item on the 2003 revised certificate and is considered comparable to the 1989 version. We did not find studies evaluating the quality of this item on the 2003 birth certificate; however, earlier studies from the 1989 birth certificate show both high and low quality for this item (Se 0%‐99.6%).36, 53
Previous Caesarean delivery and previous preterm birth were modified with the 2003 revision and considered non‐comparable to the 1989 birth certificate. Previous Caesarean delivery was reported with moderate‐to‐high data quality (Se 62.5%‐91.0%; κ 0.72‐0.88), but there was evident variability across vital registration areas (i.e, states A and B or New York City and Vermont).19, 39 On the other hand, previous preterm birth had low‐to‐moderate data quality (Se 20.6%‐65.5%; κ 0.29‐0.31).19, 54 This latter data item was under consideration to cut from the national file. A decision to continue to collect this information was made based on its public health importance and ability to improve this item through data quality efforts.
6.4. Labour and delivery
We examined only a few labour and delivery items—method of delivery and maternal morbidities. As with the 1989 birth certificate, the final route method of delivery was shown to be reported with high accuracy and reliability (Se 91.8%‐99.4%; κ 0.93‐0.97).19, 39, 50 Only one study has evaluated the accuracy of maternal morbidity information on birth certificates compared to hospital discharge data. They found substantial under‐reporting for maternal intensive care unit admission (Se 20%), blood transfusion (Se 12.0%) and uterine rupture (Se 26.0%).55
6.5. Infant health outcomes
Lastly, infant health outcomes were found to have moderate‐to‐high data quality. For birth outcomes, low birthweight was shown to be accurately reported using 2003 revised data (PA 95.7%‐100%),19 consistent with previous studies using the 1989 revision.50 The accuracy of preterm birth derived from the OE of gestation varied from moderate to high depending on the source of information for comparison. When compared with the gold‐standard “estimated date of delivery” on medical records, preterm birth was captured with a high degree of accuracy (Se 82.5%‐93.8%).56 Other studies showed more variation and slightly lower data quality when compared with medical records (PA 72.5%‐95.3%) or first ultrasound (Se 74.9%).19, 57 Preterm birth derived from the LMP‐based gestational age measure showed similar variability in the one study using 2003 revised birth certificate data (PA 72.1%‐94.8%); however, this measure has historically been shown to be less accurate than the OE of gestation.34
Finally, we examined two newborn health measures—the 5‐minute Apgar score and NICU admission. The Apgar score has been evaluated previously based on the 1989 birth certificate revision and shown to have good data quality (PA 97.5%‐98.3%; κ 0.91).36, 58 No new data quality studies have been examined after the 2003 revision. NICU admission was added to the birth certificate with the 2003 revision. Only one study evaluated this outcome and showed substantial variability by state with a sensitivity and κ of 95.1% and 0.90 in State A and 45.1% and 0.57 in State B, respectively.19
6.6. Data quality summary
While a number of changes have been made with the 2003 revision to improve data quality, some medical and health data items are under‐reported resulting in a moderate/low ranking of data quality. Improvements based on recent data quality initiatives, such as the e‐learning training, would not be reflected in this review. Another challenge for evaluating the quality of data items on the national file is state and hospital variation in data quality, which was demonstrated for some data items in the studies reviewed. Thus, it is hard to extrapolate findings from state‐based quality control reviews to a national level. On the other hand, the variability also suggests that some states and hospitals are collecting high‐quality data and that quality improvement efforts have the potential to improve data quality overall. Finally, validity and reliability studies are limited by smaller sample size or the source selected for data comparison. In particular, medical record abstraction may provide the gold standard for comparison, but is limited in size and the ability to examine rare outcomes. Alternatively, population‐based data sources, such as PRAMS or hospital discharge data, may provide a more feasible comparison to increase sample size, but are more susceptible to misclassification. Additional validity and reliability studies to assess systematic variation by key demographic characteristics and to triangulate findings from different comparison data sources are needed.
7. CONCLUSION AND RECOMMENDATIONS
In this review, we highlighted key considerations for the analysis and interpretation of studies using national vital records data to examine IPI and attendant perinatal health outcomes. The 2003 revision resulted in a number of substantive changes to data collection, dissemination and quality that impact the measurement of IPI, analysis of trends and examination of associations with maternal and perinatal health outcomes. Our review of recent data quality studies pointed to substantial variation in the quality of data by item and across states. Under‐reporting, particularly of pregnancy risk factors, was also found. While this may be problematic for obtaining accurate prevalence estimates, relative associations between IPI and perinatal outcomes may still be informative, assuming no systematic differences in reporting (i.e, non‐differential misclassification).
Numerous studies have examined the relationship between IPI and perinatal outcomes, yet there is a paucity of information on maternal and long‐term infant health outcomes. National vital records remain an important resource for examining these relationships, particularly for rare outcomes and within detailed subgroups. States have the potential to further enhance the utility of vital records through linkages, either by maternally linked birth records (i.e, sibling studies) or with other data sources (e.g, health discharge data) for validating health outcomes. Future studies examining the association of IPI with maternal and perinatal data using vital records should consider these aspects of the data in their research plan, sensitivity analyses and interpretation of findings.
Supporting information
ACKNOWLEDGEMENTS
We would like to acknowledge Ms. Stephanie Ventura for her valuable feedback on this manuscript and her dedicated service and contributions to the National Vital Statistics System. We gratefully acknowledge support from the Eunice Kennedy Shriver National Center for Child Health and Human Development grant P2C‐HD041041, Maryland Population Research Center.
Thoma ME, De Silva DA, MacDorman MF. Examining interpregnancy intervals and maternal and perinatal health outcomes using U.S. vital records: Important considerations for analysis and interpretation. Paediatr Perinat Epidemiol. 2019;33:O60–O72. 10.1111/ppe.12520
REFERENCES
- 1. Ventura SJ. The U.S. national vital statistics system: transitioning into the 21st century, 1990‐2017. 2018. [PubMed]
- 2. Ahrens KA, Nelson H, Stidd R, Moskosky S, Hutcheon JA. Short interpregnancy intervals and adverse perinatal outcomes in high‐resource settings: an updated systematic review. Paediatr Perinat Epidemiol. 2018; in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ball SJ, Pereira G, Jacoby P, de Klerk N, Stanley FJ. Re‐evaluation of link between interpregnancy interval and adverse birth outcomes: retrospective cohort study matching two intervals per mother. BMJ. 2014;349:g4333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hanley GE, Hutcheon JA, Kinniburgh BA, Lee L. Interpregnancy interval and adverse pregnancy outcomes: an analysis of successive pregnancies. Obstet Gynecol. 2017;129:408‐415. [DOI] [PubMed] [Google Scholar]
- 5. Klebanoff MA. Interpregnancy interval and pregnancy outcomes: causal or not? Obstet Gynecol. 2017;129:405‐407. [DOI] [PubMed] [Google Scholar]
- 6. Shachar B, Mayo J, Lyell D, et al. Interpregnancy interval after live birth or pregnancy termination and estimated risk of preterm birth: a retrospective cohort study. BJOG. 2016;123:2009‐2017. [DOI] [PubMed] [Google Scholar]
- 7. National Center for Health Statistics . Vital statistics data available online. https://www.cdc.gov/nchs/data_access/vitalstatsonline.htm. Accessed July 1, 2018.
- 8. Healthy people 2020. https://www.healthypeople.gov/. Accessed May 25, 2018.
- 9. Schoendorf KC, Branum AM. The use of United States vital statistics in perinatal and obstetric research. Am J Obstet Gynecol. 2006;194:911‐915. [DOI] [PubMed] [Google Scholar]
- 10. Cahill AG, Macones GA. Vital considerations for the use of vital statistics in obstetrical research. Am J Obstet Gynecol. 2006;194:909‐910. [DOI] [PubMed] [Google Scholar]
- 11. National Center for Health Statistics . U.S. standard certificate of live birth, 2003 revision. 2003. https://www.cdc.gov/nchs/data/dvs/birth11-03final-ACC.pdf. Accessed May 25, 2018.
- 12. National Center for Health Statistics . Revisions of the U.S. standard certificates and reports. https://www.cdc.gov/nchs/nvss/revisions-of-the-us-standard-certificates-and-reports.htm. Accessed May 25, 2018.
- 13. National Center for Health Statistics . User guide to the 2007 natality public use file. 2010. ftp://ftp.cdc.gov/pub/health_statistics/nchs/dataset_documentation/dvs/natality/userguide2007.pdf. Accessed May 25, 2018.
- 14. National Center for Health Statistics . Guide to completing the facility worksheet for the certificate of live birth and report of fetal death. 2016. https://www.cdc.gov/nchs/data/dvs/GuidetoCompleteFacilityWks.pdf. Accessed May 25, 2018.
- 15. National Center for Health Statistics . Specifications for collecting and editing the United States standard certificates of birth and death ‐ 2003 revision. 2001. https://www.cdc.gov/nchs/data/dvs/Guidelinesbirthspecs1101acc.pdf. Accessed May 25, 2018.
- 16. National Center for Health Statistics . Table C. The public use natality file ‐ 2015 update. 2016. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/DVS/natality/UserGuide2015.pdf. Accessed May 25, 2018.
- 17. National Center for Health Statistics . Addendum to the 2009 user guide to the natality public use file. 2011. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/DVS/natality/UserGuide2009_Addendum.pdf. Accessed May 25, 2018.
- 18. National Center for Health Statistics . User guide to the 2016 natality public use file. 2017. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/DVS/natality/UserGuide2016.pdf. Accessed May 25, 2018.
- 19. Martin JA, Wilson EC, Osterman MJK, Saadi EW, Sutton SR, Hamilton BE. Assessing the quality of medical and health data from the 2003 birth certificate revision: results from two states. Natl Vital Stat Rep. 2013;62:1‐19. [PubMed] [Google Scholar]
- 20. Curtin SC, Osterman MJK, Uddin SF, Sutton SR, Reed PR. Source of payment for the delivery: births in a 33‐state and District of Columbia reporting area, 2010. Natl Vital Stat Rep. 2013;62:1‐20. [PubMed] [Google Scholar]
- 21. Thoma ME, Boulet S, Martin JA, Kissin D. Births resulting from assisted reproductive technology: comparing birth certificate and National ART Surveillance System Data, 2011. Natl Vital Stat Rep. 2014;63:1‐11. [PubMed] [Google Scholar]
- 22. Copen CE, Thoma ME, Kirmeyer S. Interpregnancy Intervals in the United States: Data From the Birth Certificate and the National Survey of Family Growth. Natl Vital Stat Rep. 2015;64:1‐10. [PubMed] [Google Scholar]
- 23. National Center for Health Statistics . Deletion of data items from the birth and fetal death national files. https://www.cdc.gov/nchs/nvss/revisions-of-the-us-standard-certificates-and-reports.htm. Accessed May 25, 2018.
- 24. Menard MK, Main EK, Currigan SM. Executive summary of the reVITALize initiative: standardizing obstetric data definitions. Obstet Gynecol. 2014;124:150‐153. [DOI] [PubMed] [Google Scholar]
- 25. Centers for Disease Control and Prevention (CDC) . Applying best practices for reporting birth certificate medical and health information. http://www.cdc.gov/nchs/training/BirthCertificateElearning. Accessed May 25, 2018.
- 26. Williamson M. Nurses achieving best practices for birth reporting. PhD dissertation. Pittsburgh (PA): Carlow University; 2017. https://pqdtopen.proquest.com/doc/1910108896.html?FMT=ABS&pubnum=10277784. [Google Scholar]
- 27. Melnik TA, Guldal CG, Schoen LD, Alicandro J, Henfield P. Barriers in accurate and complete birth registration in New York State. Matern Child Health J. 2015;19:1943‐1948. [DOI] [PubMed] [Google Scholar]
- 28. Northam S, Polancich S, Restrepo E. Birth certificate methods in five hospitals. Public Health Nurs. 2003;20:318‐327. [DOI] [PubMed] [Google Scholar]
- 29. Ahrens KA, Hutcheon JA. Optimal birth spacing: what can we measure and what do we want to know? Paediatr Perinat Epidemiol. 2018;32:149‐151. [DOI] [PubMed] [Google Scholar]
- 30. Conde‐Agudelo A, Rosas‐Bermudez A, Castaño F, Norton MH. Effects of birth spacing on maternal, perinatal, infant, and child health: a systematic review of causal mechanisms. Stud Fam Plann. 2012;43:93‐114. [DOI] [PubMed] [Google Scholar]
- 31. Conzuelo‐Rodriguez G, Naimi AI. The impact of computing interpregnancy intervals without accounting for intervening pregnancy events. Paediatr Perinat Epidemiol. 2018;32:141‐148. [DOI] [PubMed] [Google Scholar]
- 32. Ventura . Chapter 2: vital statistics from the National Center for Health Statistics In: Douglas Besharov, ed. Data Needs for Measuring Family and Fertility Change After Welfare Reform. College Park, MD: Maryland School of Public Affairs Welfare Reform Academy; 2001: 21‐41. [Google Scholar]
- 33. Thoma ME, Copen CE, Kirmeyer SE. Short interpregnancy intervals in 2014: differences by maternal demographic characteristics. NCHS Data Brief. 2016;64:1‐8. [PubMed] [Google Scholar]
- 34. Martin JA, Osterman MJK, Kirmeyer SE, Gregory ECW. Measuring gestational age in vital statistics data: transitioning to the obstetric estimate. Natl Vital Stat Rep. 2015;64:1‐20. [PubMed] [Google Scholar]
- 35. McHugh ML. Interrater reliability: the kappa statistic. Biochemia Medica. 2012;22:276‐282. [PMC free article] [PubMed] [Google Scholar]
- 36. Zollinger TW, Przybylski MJ, Gamache RE. Reliability of Indiana birth certificate data compared to medical records. Ann Epidemiol. 2006;16:1‐10. [DOI] [PubMed] [Google Scholar]
- 37. Vinikoor LC, Messer LC, Laraia BA, Kaufman JS. Reliability of variables on the North Carolina birth certificate: a comparison with directly queried values from a cohort study. Paediatr Perinat Epidemiol. 2010;24:102‐112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ahluwalia IB, Helms K, Morrow B. Assessing the validity and reliability of three indicators self‐reported on the pregnancy risk assessment monitoring system survey. Public Health Rep. 2013;128:527‐536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dietz P, Bombard J, Mulready‐Ward C, et al. Validation of selected items on the 2003 U.S. standard certificate of live birth: New York City and Vermont. Public Health Rep. 2015;130:60‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kane DJ, Sappenfield WM. Ascertainment of medicaid payment for delivery on the iowa birth certificate: is accuracy sufficient for timely policy and program relevant analysis? Matern Child Health J. 2014;18:970‐977. [DOI] [PubMed] [Google Scholar]
- 41. Willson S. Exploring the 2003 revision of the U.S. standard certificate of live births: Results of cognitive interviews conducted in state one of four. 2009. http://wwwn.cdc.gov/QBANK/report/Willson_NCHS_2008_Birth%20Certificate%201.pdf. Accessed May 25, 2018.
- 42. Willson S. Exploring the 2003 revision of the U.S. standard certificate of live births: Results of cognitive interviews conducted in state two of four. 2009. http://wwwn.cdc.gov/QBANK/report/Willson_NCHS_2008_Birth%20Certificate%202.pdf. Accessed May 25, 2018.
- 43. Willson S. Exploring the 2003 revision of the U.S. standard certificate of live births: Results of cognitive interviews conducted in state three of four. 2009. http://wwwn.cdc.gov/QBANK/report/Willson_NCHS_2008_Birth%20Certificate%203.pdf. Accessed May 25, 2018.
- 44. Willson S. Exploring the 2003 revision of the U.S. standard certificate of live births: Results of cognitive interviews conducted in state four of four. 2009. http://wwwn.cdc.gov/QBANK/report/Willson_NCHS_2008_Birth%20Certificate%204.pdf. Accessed May 25, 2018.
- 45. Howland RE, Mulready‐Ward C, Madsen AM, et al. Reliability of reported maternal smoking: comparing the birth certificate to maternal worksheets and prenatal and hospital medical records, New York City and Vermont, 2009. Matern Child Health J. 2015;19:1916‐1924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Tong VT, Dietz PM, Farr SL, D'Angelo DV, England LJ. Estimates of smoking before and during pregnancy, and smoking cessation during pregnancy: comparing two population‐based data sources. Public Health Rep. 2013;128:179‐188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Searles Nielsen S, Dills RL, Glass M, Mueller BA. Accuracy of prenatal smoking data from Washington State birth certificates in a population‐based sample with cotinine measurements. Ann Epidemiol. 2014;24:236‐239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Park S, Sappenfield WM, Bish C, Bensyl DM, Goodman D, Menges J. Reliability and validity of birth certificate prepregnancy weight and height among women enrolled in prenatal wic program: Florida, 2005. Matern Child Health J. 2011;15:851‐859. [DOI] [PubMed] [Google Scholar]
- 49. Bodnar LM, Abrams B, Bertolet M, et al. Validity of birth certificate‐derived maternal weight data. Paediatr Perinat Epidemiol. 2014;28:203‐212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Northam S, Knapp T. The reliability and validity of birth certificates. J Obstet Gynecol Neonatal Nurs. 2006;35:3‐12. [DOI] [PubMed] [Google Scholar]
- 51. Clayton HB, Sappenfield WM, Gulitz E, et al. The Florida investigation of primary late preterm and cesarean delivery: the accuracy of the birth certificate and hospital discharge records. Matern Child Health J. 2013;17:869‐878. [DOI] [PubMed] [Google Scholar]
- 52. Hosler AS, Nayak SG, Radigan AM. Agreement between self‐report and birth certificate for gestational diabetes mellitus: New York State PRAMS. Matern Child Health J. 2010;14:786‐789. [DOI] [PubMed] [Google Scholar]
- 53. Roohan PJ, Josberger RE, Acar J, Dabir P, Feder HM, Gagliano PJ. Validation of birth certificate data in New York State. J Community Health. 2003;28:335‐346. [DOI] [PubMed] [Google Scholar]
- 54. Hackney DN, Durie DE, Dozier AM, Suter BJ, Glantz JC. Is the accuracy of prior preterm birth history biased by delivery characteristics? Matern Child Health J. 2012;16:1241‐1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Luke B, Brown MB, Liu C, Diop H, Stern JE. Validation of severe maternal morbidity on the us certificate of live birth. Epidemiology. 2018;29:e31‐e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Dietz PM, Bombard JM, Hutchings YL, et al. Validation of obstetric estimate of gestational age on US birth certificates. Am J Obstet Gynecol. 2014;210:335.e1‐335.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Barradas DT, Dietz PM, Pearl M, England LJ, Callaghan WM, Kharrazi M. Validation of obstetric estimate using early ultrasound: 2007 California birth certificates. Paediatr Perinat Epidemiol. 2014;28:3‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. DiGiuseppe DL, Aron DC, Ranbom L, Harper DL, Rosenthal GE. Reliability of birth certificate data: a multi‐hospital comparison to medical records information. Matern Child Health J. 2002;6:169‐179. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


