Abstract
Background: The recurrence of urothelial carcinoma in orthotopic ileal neobladder is an extremely rare entity. We present a case of a patient who developed urothelial carcinoma in a robotically formed ileal neobladder (Studer), 10 years after primary surgery, who was managed with robotic neocystectomy.
Case Presentation: A 56 year-old patient presented with gross hematuria 10 years after robotic cystoprostatectomy, lymphadenectomy, and intracorporeal formation of Studer ileal neobladder. After surgery the patient was closely followed up using cytology testing, cystoscopy, and imaging at regular intervals. Ten years later the patient presented gross hematuria. Cystoscopic examination with biopsies was performed, revealing the presence of high-grade urothelial carcinoma. The patient under general anesthesia was placed in a position similar to robotic prostatectomy and robotic neocystectomy with bilateral ureterostomy was performed.
Conclusion: Although urothelial carcinoma in an orthotopic neobladder is unusual, recurrence should be considered in patients with hematuria who underwent radical cystoprostatectomy and orthotopic ileal neobladder formation. However, those patients can be managed safely and effectively, performing robotic neocystectomy.
Keywords: urothelial carcinoma recurrence, urinary diversion, robotic neocystectomy
Introduction
It is well known that urothelial carcinomas are multifocal and as a result 70% of the patients will develop recurrence, which in an orthotopic neobladder is a rare entity. Only a few cases have been reported in the literature.1
We present a case of a patient who developed urothelial carcinoma recurrence in a robotically formed ileal (Studer) neobladder, 10 years after surgery.
Case Presentation
In 2008, a 56 year-old man had been diagnosed with pT1 grade III in situ urothelial carcinoma of the bladder with lamina propria invasion. He underwent robotic radical cystoprostatectomy, bilateral extended lymphadenectomy, and creation of Studer orthotopic neobladder. The histopathologic findings suggested urothelial carcinoma (T1, grade III, in situ) without lymph node metastasis and prostate adenocarcinoma with a Gleason score of 6.
After surgery the patient was closely followed up using urine cytology, imaging, and cystoscopy at regular intervals (Figs. 1 and 2).
FIG. 1.
Postoperative IVP 8 years after surgery showed normal upper tract and neobladder. IVP, intravenous pyelography.
FIG. 2.
Postoperative CT urography at 2 years. CT, computed tomography.
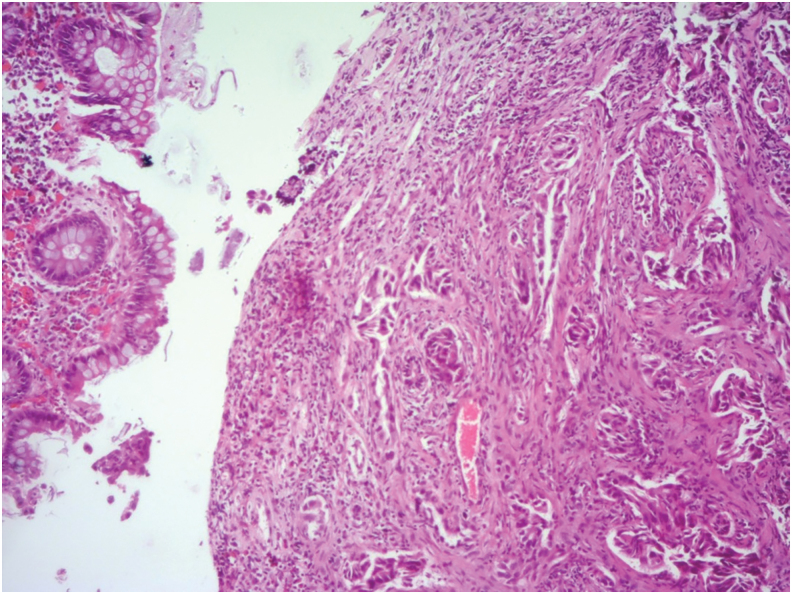
Ten years after uneventful follow-up the patient reported macroscopic hematuria. Cytology test of the urine as well as imaging (CT urography) were negative; therefore, cystoscopy with biopsies was performed according to the existing guidelines. The histopathologic examination of the biopsies revealed the presence of an invasive urothelial carcinoma with granular metaplasia, which invades the muscularis propria of the ileal neobladder (Fig. 3).
FIG. 3.
Histopathology report from biopsy.
Ten years after the primary surgery, a robotic neocystectomy was scheduled.
With the patient in the Trendelenburg position similar to robotic prostatectomy, a robotic platform of da Vinci Si system was used and trocars placed in the same incision sites, done 10 years ago. The intraperitoneal pressure was set at 9 mm Hg and three robotic instruments (a Maryland bipolar forceps, a Cadiere forceps, and a monopolar curved scissor) were used for the procedure.
During the operation there were multiple adhesions at the space of Retzius formed from the previous surgery, needing meticulous dissection to avoid tumor spillage. The ureters were dissected free and frozen sections were sent, which were negative for recurrence. The entire neobladder with the mesentery detached easily from the intraperitoneal structures, except of the ureteral anastomosis area, whose excessive adhesions needed vigorous adhesiolysis. The neobladder specimen was finally removed en bloc and placed in a laparoscopic sac. At the end of the procedure there was a mild difficulty observed in terms of ureteral shortening and so for the ureters were exited in two separate sites of the abdominal wall, in the middle of the line between anterior superior iliac spine and umbilicus.
There were no intraoperative complications. The total operative time was 168 minutes with an estimated blood loss of 120 mL. The patient reported minimal postoperative pain, resumed regular diet on the first postoperative day, and was discharged from the hospital on post operative day 3.
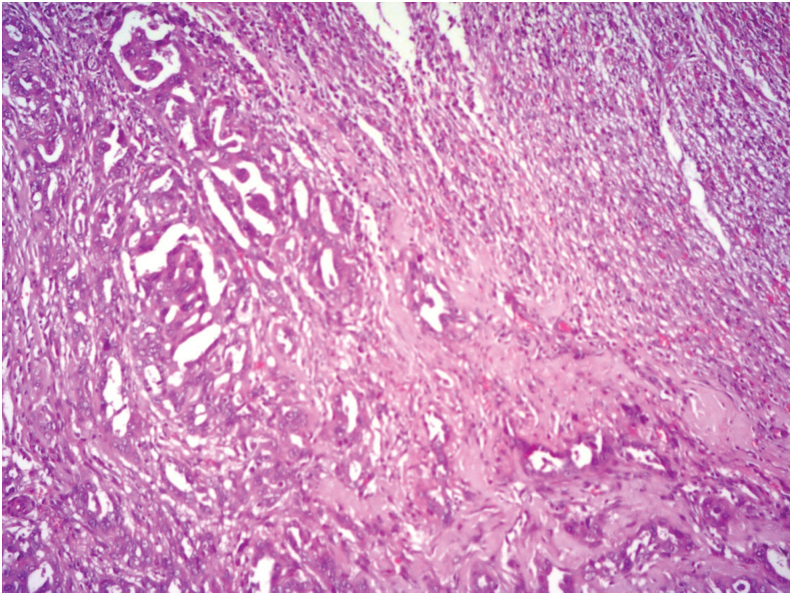
Histopathologic examination of the neobladder specimen revealed urothelial carcinoma with extensive granular differentiation and moderate peritumoral fibrosis (Fig. 4).
FIG. 4.
Final pathology report.
The patient followed up by an oncologist for a four-cycle adjuvant chemotherapy and after a year there is no local recurrence or distant metastasis.
Discussion
We described a rare case of recurrent urothelial carcinoma in an ileal neobladder 10 years after radical cystoprostatectomy.
In our knowledge there are only a few reports in the current literature, concerning urothelial recurrence after radical cystoprostatectomy with orthotopic ileal neobladder substitution.1,2
There are two theories regarding the mechanism of urothelial recurrence. The first theory is “field carcinogenesis” according to which tumor cells exist in the normal urothelium, where they eventually and independently may develop into tumors.
The second one is “seed and implantation” according to which papillary tumors of the upper urinary tract frequently recur in the bladder (15%–50%) and has been proven that urothelial tumor cells originated from the renal pelvis, which is the source of this theory (seed and implantation).
In our case the urothelial carcinoma recurred in the intestinal mucosa, which can be explained by the “seed and implantation” theory. It is claimed that droplets of tubular cells (seeds) find bladder or nonurothelial surfaces compatible for both implantation and growth. Intraluminar tumor cell seeding appears to be an important mechanism of metachronous transitional cell carcinoma recurrence and, therefore, can be considered as one of the potential factors that contribute to multifocal recurrence of TCC in tissues other than urothelium.3
Conclusion
Although urothelial carcinoma in an orthotopic neobladder is unusual, recurrence should be considered in patients with hematuria who underwent prior radical cystectomy with ileal neobladder formation.
No guidelines exist regarding the management of urothelial carcinoma recurrence.
However, surgical management of tumors in orthotopic neobladder is possible and feasible if diagnosed in time and can be managed safely and effectively performing minimally invasive techniques such as robotic neocystectomy.4
Abbreviations Used
- CT
computed tomography
- IVP
intravenous pyelography
Disclosure Statement
No competing financial interests exist.
Cite this article as: Pardalidis PN, Andriopoulos NA, Kosmaoglou EV, Pardalidis VN, Pardalidis NP (2020) Urothelial carcinoma recurrence in an ileal orthotopic neobladder 10 years after primary robotic radical cystoprostatectomy, Journal of Endourology Case Reports 6:1, 16–18, DOI: 10.1089/cren.2019.0055.
References
- 1. Cherbank F, Prod'homme M, Pazzetta E, et al. . Urothelial carcinoma recurrence in an ileal neobladder 9 years after primary surgery with Muir-Torre syndrome. Case Rep Urol 2016;2016:4762514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Herawi M, Leppert JT, Thomas GV, et al. . Implants of noninvasive papillary urothelial carcinoma in peritoneum and ileocolonic neobladder: Support for seed and soil hypothesis of bladder recurrence. Urology 2006;67:746–750 [DOI] [PubMed] [Google Scholar]
- 3. Groen VH, Lock TM, Keizer B, et al. . Urothelial carcinoma in an orthotopic neobladder: An unusual pattern of recurrence and metastasis. BMJ Case Rep 2017;2017:bcr-2017-221052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Schumacher MC, Jonsson MN, Pardalidis NP, et al. . Surgery-related complications of robot-assisted radical cystectomy with intracorporeal urinary diversion. Urology 2011;77:871–876 [DOI] [PubMed] [Google Scholar]