Abstract
The identification of oncogenic drivers, and the subsequent development of targeted therapies established biomarker-based care for metastatic non-small cell lung cancer (NSCLC). Biomarker testing is standard of care in NSCLC patients with adenocarcinoma because multiple targeted therapies are available. Rearranged during transfection (RET) rearrangements were identified as oncogenic drivers in NSCLC, and are more common among younger patients, adenocarcinoma histology, and patients with a history of never smoking. The prevalence is estimated to be 1–2% among patients with adenocarcinoma histology. The most common rearrangement is between intron 11 of the RET gene and intron 15 of the KIF5B gene, and the next most frequent rearrangement is with the CCDC6 gene. RET rearrangements lead to constitutive activation of the RET tyrosine kinase and increased cell proliferation, migration, and survival. Phase II studies investigated the activity of multi-targeted tyrosine kinase inhibitors in patients with NSCLC with a confirmed RET rearrangement. These agents have limited potency against RET, and activity against the epidermal growth factor receptor and vascular endothelial growth factor pathways. These agents revealed modest activity, and were poorly tolerated due to the off-target toxicities. These struggles contributed to the development of more potent and specific RET tyrosine kinase inhibitors. Preliminary results from early phase trials of selpercatinib (LOXO-292) and pralsetinib (BLU-667) revealed promising efficacy and improved tolerability. The availability of these agents will make routine testing for RET rearrangements a priority.
Keywords: biomarker, comprehensive genomic profiling, non-small cell lung cancer, precision medicine, selpercatinib, pralsetinib, targeted therapy
Lung cancer is the leading cause of cancer-related mortality in the United States, and one of the leading causes globally.1,2 The majority of cases of lung cancer are the non-small cell lung cancer (NSCLC) subtype, and the majority of patients present with locally advanced or metastatic disease.3 NSCLC is further subdivided based on histology (e.g. adenocarcinoma, squamous, or large cell carcinoma). Historically, patients with metastatic NSCLC were treated with a platinum-doublet and the specific histology did not influence treatment selection. However, in an early trial of bevacizumab a higher rate of pulmonary hemorrhage was observed among patients with NSCLC with squamous histology, and the use of bevacizumab was restricted to patients with non-squamous histology.4,5 The activity of pemetrexed was found to be restricted to patients with non-squamous histology.6 The development of these agents contributed to the development of histology-based selection of therapy for NSCLC.
Epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) were initially developed in unselected patients, but patients with a history of never or light smoking, Asian ethnicity, and adenocarcinoma histology were observed to have a higher response rate. These clinical characteristics were associated with a higher prevalence of EGFR activating mutations, and patients with EGFR mutant NSCLC experienced greater clinical benefit from EGFR TKIs. Conversely patients without an EGFR mutation experience limited benefit from EGFR TKIs.7 The development of EGFR TKIs established a biomarker-driven care for NSCLC. Subsequently, anaplastic lymphoma kinase (ALK) rearrangements were observed to be oncogenic drivers in NSCLC, and ALK TKIs were developed only in patients with an identified ALK rearrangement.8,9 The activity observed in early phase trials led to the rapid approval of this class of agents. The development of targeted therapies in a biomarker selected patient populations became the preferred paradigm for novel targeted therapies.
The success of these targeted therapies combined with the increased availability and affordability of comprehensive genomic profiling changed the clinical research focus in thoracic oncology to developing novel agents in specific molecular subgroups. Targeted therapies were subsequently developed for patients with ROS1 rearrangements, BRAF V600E mutations, MET exon 14 alterations, and NTRK rearrangements.10–14 These agents were approved based on a single arm phase II trials which only enrolled patients with the specific biomarker of interest. The prevalence of these molecular alterations is approximately 1–3%, and the successful development of targeted therapies encouraged drug development in other rare molecular subtypes. The clinical impact of having multiple ‘actionable alterations’ is that many centers have adopted broad testing panels rather than using single gene tests.15
Rearranged during transfection (RET) gene rearrangements were identified as oncogenic drivers in NSCLC, and there has been a long-standing interest in developing a targeted therapy for this molecular alteration.16,17 RET rearrangements are more common in patients with a history of never or light smoking, adenocarcinoma histology, and younger patients. RET rearrangements are mutually exclusive with other oncogenic drivers.18,19 The estimated prevalence of RET rearrangements observed in NSCLC with adenocarcinoma is 1–2%, and when patients without another oncogenic driver mutation are examined the prevalence of RET rearrangements is approximately 5%.17–21 The initial research focus investigated the activity of multi-targeted TKIs which had shown activity in other malignancies. Recently, early phase trials have demonstrated activity of RET-specific TKIs which will fundamentally change the clinical management of RET + NSCLC.
Molecular biology
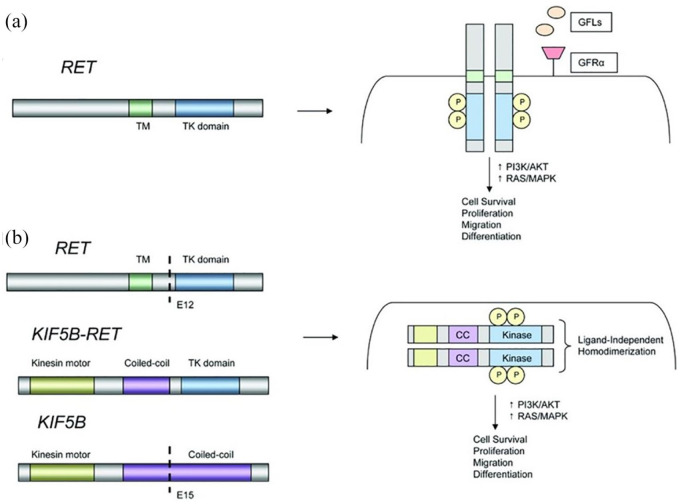
The RET tyrosine kinase is a transmembrane glycoprotein, and RET does not bind directly to the receptor ligands. The glial-derived neurotrophic factor ligands (GFLs) bind to glial-derived neurotrophic factor family receptors (GFRα), which act as co-receptors for RET. The GFL–GFRα complex leads to RET homodimerization and subsequent autophosphorylation of the intracellular domain of the tyrosine kinase (Figure 1).22 The oncogenic event in NSCLC is a chromosomal rearrangement which produces a RET fusion protein.17,20,21,23 The RET gene is located on chromosome 10, and the pathogenic event is an intrachromosomal rearrangement. The most common partner genes are KIF5B, CCDC6, and NCOA4. KIF5B is the most common rearrangement observed in NSCLC (approximately 70% of cases), and the most common fusion is intron 11 of the RET gene and intron 15 of KIF5B.17,20,21,24,25 Numerous other gene rearrangements have also been reported (e.g. MYO5C, EPHA5, TRIM24, and TRIM33).23,26 The RET rearrangement is a combination of the RET intracellular kinase domain and the coiled coil domain of the partner gene, which results in ligand independent homodimerization and activation of the RET tyrosine kinase by autophosphorylation.26,27 This leads to constitutive activation of the RET tyrosine kinase and increased cell proliferation, survival, migration and differentiation by activation of the phosphoinositide 3-kinases (PI3K)/AKT, mitogen-activated protein kinase (MAPK), and Signal transducer and activator of transcription 3 (STAT3) pathways (Figure 1).22,23,28
Figure 1.
Mechanism of RET rearrangements.22
Models of RET rearrangements. (A) Schematic representation of the RET proto-oncogene (left). RET activation typically involves ligand binding, interactions with a co-receptor, and homodimerization leading to formation of a multiprotein complex (right). (B) Schematic representation of a KIF5B–RET fusion (left). The coiled-coil domain of KIF5B promotes ligand-independent homodimerization of RET, leading to constitutive activation of downstream growth signaling.
CC, coiled-coil domain; GFL, glial cell line-derived neurotrophic factor family ligand; GFRα, GDNF family receptor α; KIF5B, kinesin family member 5B; P, phosphorylated tyrosine residue; RET, rearranged during transfection; TK, tyrosine kinase; TM, transmembrane.Used with permission from AlphaMed Press from Justin F Gainor and Alice T Shaw.22 Permission conveyed through Copyright Clearance Center, Inc.
Diagnostic testing
A variety of molecular testing methods has been employed to detect RET rearrangement in retrospective studies including whole exome sequencing, next generation sequencing (NGS), reverse transcription polymerase chain reaction (RT–PCR), fluorescence in situ hybridization (FISH), and immunohistochemistry (IHC). IHC testing is efficient and convenient, but the sensitivity and specificity are inadequate for routine clinical use.17,26,29 In order to improve the performance IHC future studies will need to develop a more specific antibody and define the optimal cut-off for positive values. Most RET FISH tests use a dual color break apart probe and examine 50 tumor cells, and classify positive cases as having split signals or an isolated 3' prime signal.19,30 In previous studies, the RET FISH break apart probe-positive cases underwent an additional FISH break apart probe for KIF5B and CCDC6 to confirm a RET rearrangment.19,30 The cut-off of tumor cells demonstrating a signal to be considered positive has varied, with most studies using a cut-off between 10% and 20% of cells.19,29–31 FISH testing is highly sensitive, but the concerns are the technical expertise required and the test is not widely available. Reverse transcriptase polymerase chain reaction (RT–PCR) was used in RET screening studies, and used predefined primers to detect RET fusions.19,25,32 The strength is the ability to identify the specific RET fusion; however, RT–PCR will not detect unknown fusion partners or variants, and poor preservation of RNA in the tumor sample can reduce the sensitivity. Many of the studies which used RT–PCR also used a second test to confirm the presence of a RET rearrangement.19,20,26
Hybrid capture-based NGS allows the assessment of multiple molecular alterations and potential concurrent mutations in a single test. Overall the last several years NGS testing has become more widely available for routine clinical care. The disadvantages are the detection of alterations of uncertain clinical significance, and concerns about the variation in the testing methods (i.e. whether RET is included in the testing panel). RET rearrangements can also be detected using circulating tumor DNA (ctDNA).33 The primary advantages of ctDNA testing are the ability to test for a broad panel of molecular alterations simultaneously and the shorter turnaround time compared to tumor testing. The primary concern is the lower sensitivity, especially in patients with fewer extra-thoracic metastatic lesions or lower disease burden.33 If a ctDNA test reveals a RET rearrangement or another oncogenic driver (e.g. EGFR, BRAF V600E, ALK, ROS1 molecular alterations) then the results can be acted on clinically. However, if there is no detectable DNA (i.e. an ‘uninformative’ test result) or an oncogenic driver is not identified (i.e. ‘mutation negative’) a tumor biopsy should be performed.
Preliminary studies suggest RNA sequencing when integrated with DNA sequencing on tumor samples in which DNA fails to detect an oncogenic driver has the potential to detect additional gene fusions.34,35 However, RNA sequencing is not widely available for clinical use.
RET FISH testing and NGS panels are the most commonly used clinical tests to identify RET rearrangements.
Clinical data with multi-targeted TKIs
The initial attempts to develop a targeted therapy for RET rearrangements focused on the use of multi-targeted TKIs with indications in others solid tumors such as renal cell carcinoma, hepatocellular carcinoma, or thyroid cancer. These drugs inhibit the RET tyrosine kinase but had limited potency for RET as they were not developed as RET-specific inhibitors, and had activity against the vascular endothelial growth factor (VEGF) receptors and/or the EGFR pathway.36 Many of the adverse events observed were related to the activity of these agents on the EGFR (e.g. dermatologic toxicities and diarrhea) or VEGF pathways (e.g. hypertension), and these adverse events frequently required dose reduction, interruption, or treatment discontinuation. These off-targeted toxicities may have led to dose reduction below the dose required to effectively inhibit RET. The combination of the low potency and frequent dose reduction contributed to the lower objective response rate (ORR) and progression-free survival (PFS) with these agents compared to targeted therapies in patients with EGFR, ALK, and ROS1 alterations.
The clinical data available on the activity of multi-targeted TKIs are a combination of retrospective cases series, and small prospective single arm phase II trials. The prospective studies provide the most accurate data about the drug activity, adverse events, and tolerability (Table 1). Vandetanib is a multi-targeted TKI with activity against the VEGF receptors, EGFR, and RET. The study by Yoh et al. of vandetanib screened patients with EGFR mutation-negative NSCLC using RT–PCR and FISH testing was used to confirm RT–PCR positivity.18 Of the 1536 patients who were screened, 34 patients were RET positive, and 19 patients were enrolled in the trial. Vandetanib demonstrated activity (Table 1), but grade 3 or 4 adverse events were common. The most common grade 3 or 4 adverse events were hypertension (n = 11, 58%), diarrhea (n = 2, 11%), rash (n = 3, 16%), dry skin (n = 1, 5%), and QT prolongation (n = 2, 11%). Four of the 19 patients discontinued therapy related to adverse events. A second trial by Lee et al. recruited patients with NSCLC without EGFR mutations or ALK rearrangements, and screened patients with FISH; FISH RET positive results were confirmed with IHC, RT–PCR, or NGS.37 Of the 315 patients recruited, 26 patients (8.3%) were positive by FISH testing, and 18 patients were enrolled in the study. Vandetanib demonstrated activity (Table 1), and the grade 3 adverse events observed were hypertension (n = 3, 17%) QT prolongation (n = 2, 11%) and elevated liver tests (n = 1, 6%).
Table 1.
Select prospective phase II trials of multi-targeted tyrosine kinase inhibitors in RET rearranged non-small cell lung cancer.
| Agent | No. of patients | Objective response rate | Progression-free survival (median in months) | Median overall survival (median in months) | Dose reduction |
|---|---|---|---|---|---|
| Vandetanib18 | 19 | 9/19 (47%) | 4.7 | 11.1 | 10/19 (53%) |
| Vandetanib37 | 18 | 3/17 (18%) | 4.5 | 11.6 | 4/18 (22%) |
| Cabozantinib38 | 26 | 7/25 (28%) | 5.5 | 9.9 | 19/26 (73%) |
| Lenvatinib39 | 36 | 4/25 (16%) | 7.3 | NA | 16/25 (64%) |
| RXDX-10540 | 31 | 6/31 (19%)a | NA | NA | 19/62 (31%)a |
| Alectinib41 | 25 | 1/25 (4%)b | 3.4b | 19b | NA |
NE, not evaluable.
The response data are for patients with RET rearrangement who are RET tyrosine kinase inhibitor naïve. The dose reduction values are for the patients included in the phase Ib part of the trial treated at the recommended phase II dose.
Data are the efficacy results in the phase II part of the trial.
Cabozantinib is a multi-targeted TKI with activity against RET as well as ROS1, MET, VEGF receptors, AXL, TIE2 and KIT. A single arm phase II trial enrolled patients with RET rearrangement detected on FISH or NGS testing (Table 1).38 The most common grade 3 treatment-related adverse events were asymptomatic elevation of lipase (n = 4, 15%), increased alanine aminotransferase (ALT) (n = 2, 8%) increased aspartate aminotransferase (AST) (n = 2, 8%), thrombocytopenia (n = 2, 8%), and hypophosphatemia (n = 2, 8%). Nineteen patients (73%) required a dose reduction related to an adverse event. Lenvatinib is a multi-targeted TKI with activity against VEGF receptors, fibroblast growth factor receptors, platelet-derived growth factor receptor alpha, RET and KIT. Tumor samples underwent tumor testing at the central laboratory using NGS, and 536 patients were screened and 25 (5%) were eligible. A single arm phase II trial revealed modest activity (Table 1).39 The most common grade ⩾ 3 treatment-emergent adverse events were hypertension (n = 14, 56%), hyponatremia (n = 5, 20%), proteinuria (n = 4, 16%), pneumonia (n = 4, 16%), and nausea (n = 3, 12%). Six patients experienced treatment-related adverse events leading to treatment discontinuation.
RXDX-105 differs from the other multi-targeted TKIs because it has RET activity, and limited activity against the VEGF receptors.40 A phase I/Ib trial investigated the activity of RXDX-105 in patients who were RET TKI naive and in patients previously treated with multi-targeted TKI. In the RET TKI naive patients, the drug revealed modest activity (Table 1). A subset analysis revealed that the response rate varied by fusion partner. The ORR in the RET-KIF5B rearrangement subset, the most common rearrangement, was 0% (0/20), and the RET-non-KIF5B rearrangement subset was 67% (6/9) (p < 0.001). The reason for the difference in the ORR based on the type of RET rearrangement is unclear.40 In the patients who were previously treated with a multi-targeted (vandetanib or cabozantinib) TKI the response rate was 0% (0/9). The median duration of response, PFS and overall survival (OS) are not available. The most common adverse events at the recommend phase II dose (n = 74) were rash (n = 7, 10%), elevated ALT (n = 6, 8%), hypophosphatemia (n = 5, 7%), and elevated AST (n = 4, 5%). At this time no further trials are planned with this agent.42
A case series of four patients revealed activity of alectinib, an ALK TKI, at a dose of 600 or 900 mg twice daily.43 The activity of alectinib was investigated in patients who were RET TKI treatment naive in a phase I/II trial. The phase II dose was 450 mg BID, and alectinib had limited activity (Table 1).41 The grade ⩾ 3 adverse events at the 450 mg BID dose level were increased creatinine phosphokinase, increased bilirubin, diarrhea, hyponatremia, neutropenia, and pneumonitis (all in one patient, 4%).
Sorafenib was investigated in a study which enrolled three patients, and no responses were observed, and in the global registry two patients were treated and the best response was stable disease.25,44 Ponatinib is a multi-targeted TKI with RET activity, and demonstrated activity in xenograft models of RET rearrangements.45 In the global registry two patients were treated with ponatinib and the best response was stable disease, and a clinical trial was initiated and enrolled nine patients, and the results are not available at this time.25
Additional clinical information is available from a global registry of RET + NSCLC patients treated outside a clinical trial.25 Patients were required to have a RET rearrangement based on RT–PCR, FISH, NGS and the individual patient data were collected. This registry collected data on 165 RET + NSCLC from 29 centers. The majority of patients were never smokers (63%), had adenocarcinoma (98%), and KIF5B-RET rearrangement (72%). Fifty-three TKI naive patients received a multi-targeted TKI as part of their therapy. The best response rate with cabozantinib (n = 21), vandetanib (n = 11) and sunitinib (n = 10) was 37% (7 of 19 evaluable patients), 18% (2 of 11 evaluable patients), and 22%, (2 of 9 evaluable patients), respectively. As a formal response assessment was not possible, an ORR was not calculated. No differences in response or PFS-related RET rearrangement type were observed (KIF5B versus other partner). In all patients the median PFS and OS were 2.3 and 6.8 months, respectively. The median PFS observed with cabozantinib, vandetanib, and sunitinib was 3.6 months, 2.9 months, and 2.2 months, respectively and the median OS observed with cabozantinib, vandetanib, and sunitinib was 4.9 months, 10.2 months, and 6.8 months, respectively.
In summary, the multi-targeted TKIs demonstrated modest activity with poor tolerability due to off-targeted activity. With the exception of RXDX-105 the specific RET rearrangement has not been associated with efficacy. However, these analyses were subset analyses, and the number of patients with non-KIF5B rearrangements and benefiting from the therapy were small. Consequently, the relationship between the specific RET rearrangement and efficacy cannot be definitively determined.
Chemotherapy and chemotherapy and immunotherapy combinations
Many patients with RET + NSCLC are initially treated with first-line chemotherapy because molecular testing for RET rearrangements is not routine at the time of diagnosis, and there is not an established targeted therapy for RET + NSCLC. Patients with RET + NSCLC have clinical characteristics associated with better outcomes with chemotherapy. A retrospective study of pemetrexed alone (n = 1) or in combination (n = 17) in patients with RET + NSCLC (n = 18) revealed an ORR of 45% (5 of 11 patients) and a median PFS of 19 months.46 In the global registry, 84 patients received platinum-based chemotherapy in the first line setting, 65 were evaluable for response, and the best response was 51% (33 of 65 patients).25 The median PFS was 7.8 months, and median OS was 24.8 months. In the subset of 66 patients who received platinum and pemetrexed the best response was 49% (27 of 55 patients), the median PFS was 6.4 months, and the median OS was 23.6 months.
Single agent immunotherapy is available as a first-line option for patients with a programmed death-ligand 1 (PD-L1) expression ⩾1% or as second line therapy. Unfortunately, we do not have the outcomes specific to RET + NSCLC from these trials because RET status was not prospectively collected. A retrospective registry included 16 patients (3%) with RET rearrangements who were treated with single agent immunotherapy in the second or third line.47 The best response in the RET + NSCLC cohort was 6% (1 of 16 patients), and the median PFS was 2.1 months suggesting limited activity of single agent immunotherapy. Six patients underwent testing for PD-L1 expression and the median percentage of cells that expressed PD-L1 was 26, and the small sample size and low response rate limit the analysis of PD-L1 as a predictive biomarker for response in RET + NSCLC. A retrospective study identified 74 patients with RET + NSCLC.48 Twenty-six patients had sufficient tumor samples available for PD-L1 testing, and PD-L1 expression was 0%, 1–49%, and ⩾50% in 58% (n = 15), 23% (n = 6), and 19% (n = 5), respectively. Forty-four patients had sufficient tumor for tumor mutational burden (TMB) testing and the median TMB was 1.75 mutations/Mb. Fourteen patients were treated with immunotherapy, and 13 patients were evaluable for responses and no responses were observed. The median PFS was 3.4 months, and no association with PD-L1 or TMB and PFS was observed. These data suggest limited efficacy for single agent immunotherapy in RET + NSCLC.
The combination chemotherapy and immunotherapy is a first-line option without regard to PD-L1 status.49–51 Patients with RET + NSCLC were not excluded from the phase III trial of carboplatin, pemetrexed and pembrolizumab as patient with EGFR mutant and ALK rearranged NSCLC were, so patients can receive this combination. Patients with RET + NSCLC have many of the clinical characteristics (younger age and history of never smoking) and tumor characteristics (adenocarcinoma and single oncogenic driver) of patients with EGFR mutant NSCLC and ALK rearranged NSCLC. Patients with an EGFR mutation or ALK rearrangement who were previously treated with TKIs were eligible for the phase III trial of carboplatin, paclitaxel, bevacizumab (the standard arm) compared to carboplatin, paclitaxel, bevacizumab, atezolizumab or carboplatin, paclitaxel and atezolizumab. In a retrospective subset analysis patients with EGFR mutations (n = 124), patients treated with carboplatin, paclitaxel, bevacizumab and atezolizumab compared to carboplatin, paclitaxel, bevacizumab experienced a numerically higher response rate, longer PFS and longer OS.52 The outcomes of patients with an EGFR mutation treated with carboplatin, paclitaxel, atezolizumab compared to carboplatin, paclitaxel and bevacizumab were similar. Forty patients with a ALK rearrangement were enrolled in the three treatment arms, and the small number of patients in each arm limited the interpretation of the efficacy results. The results of this retrospective subset analysis suggest the combination of carboplatin, paclitaxel, bevacizumab and atezolizumab may be the preferred chemotherapy and immunotherapy combination for patients with oncogenic driver alterations with disease progression of TKI. However, we do not have specific efficacy data on patients with RET + NSCLC from this trial.
Next generation RET TKIs
The struggles with the multi-targeted TKIs spurred the development of TKIs which were more specific and potent RET inhibitors. Selpercatinib (LOXO-292) and pralsetinib (BLU-667) are highly selective for the RET tyrosine kinase, have activity against multiple RET rearrangements, and have central nervous system (CNS) activity in mouse models.53–55 These agents also have activity against acquired RET gatekeeper resistance mutations that have been observed after multi-targeted TKIs.53,56–58 Importantly, in preclinical studies mechanisms of resistance other than RET resistance mutations have been observed, including the development of the NRAS mutation and increased expression of the EGFR and AXL.59 Thus, these agents may not have activity against RET independent mechanisms of acquired resistance.
Selpercatinib was investigated in a phase I/II trial, which enrolled 253 patients with RET + NSCLC, and the primary analysis set is 105 patients who received prior platinum-based therapy.60 The median age in the primary analysis set was 61 years (range 23–81), 103 patients (98%) had a performance status of 0 or 1, 50 patients (48%) had received a multi-targeted TKIs previously, and 37 patients (35%) had brain metastases. The most common RET fusion partner was KIF5B in 85 patients (59%), followed by CCDC6 in 32 patients (22%). The recommend dose for phase II trials was 160 mg twice daily. The efficacy results for the primary analysis set and the subset of patients who were treatment naive (n = 39) revealed clinically significant activity (Table 2). The safety profile included data from 531 patients treated, and the grade 3 or 4 treatment-related adverse events observed in ⩾5% were hypertension (8% grade 3, <1% grade 4), increased AST (4% grade 3, 1% grade 4), and increased ALT (6% grade 3, 1% grade 4). Nine patients (1.7%) discontinued therapy due to treatment-related adverse events. Preliminary evidence suggests that selpercatinib has activity in patients with acquired resistance mutations from previous therapies.
Table 2.
Efficacy results of selpercatinib (LOXO-292) in RET + NSCLC in the primary analysis set and the treatment naive subset.60.
| Efficacy parameter | Primary analysis set (n = 105) | Treatment naive (n = 39) |
|---|---|---|
| Objective response rate (%) Number of patients | 68% (95% CI 58–76%) 71/105 |
85% (95% CI 69–95%) 29/34 |
| CNS objective response rate Number of patients | 91% (95% CI 59–100%) 10/11 |
Not available |
| Median duration of response Number of events | 20.3 months (95% CI 13.8–24.0) 16/69 |
Not reached 2/22 |
| Progression-free survival Number of events | 18.4 months (95% CI 12.9–24.9) 33/105 |
Not reached 4/34 |
NSCLC, non-small cell lung cancer; CI, confidence interval; CNS, central nervous system.
Pralsetinib was investigated in a phase I/II trial, which enrolled patients with RET + NSCLC who were treated with prior platinum-based therapy and were platinum naive.55 The recommended dose for phase II trials was 400 mg daily. At the time of the analysis 120 patients with RET + NSCLC were included, and 91 patients had received previous therapy with platinum-based therapy. The median age was 60 years (range 28–87), 46 patients (38%) had performance status of 1, 21 patients (18%) had received a previous multi-targeted TKI, and 48 patients (40%) had brain metastases. The most common RET fusion partner was KIF5B in 79 patients (66%), followed by CCDC6 in 16 patients (13%). Among the 48 patients evaluable for response the ORR was 58% [95% confidence interval (CI) 43–72%], and among the 35 patients who had received prior platinum-based therapy the ORR was 60% (95% CI 42–76%). Seven of the nine patients with measurable CNS disease experienced a decrease in the size of the brain metastases. The median duration of response data is not available. The grade ⩾ 3 treatment-related adverse events observed in ⩾5% of patients were neutropenia (n = 16, 13%), and hypertension (n = 12, 10%). Eight patients (7%) discontinued due treatment-related adverse events (pneumonitis, respiratory distress/hypoxia, mucositis/colitis, myelosuppression, gait disturbance, and anemia).
In addition to these agents several other RET-specific TKIs are in development. TPX-0046 is a selective RET/SRC inhibitor which has revealed preclinical activity in a RET-driven cell line and patient-derived xenograft tumor models, and a clinical trial has been initiated.61 BOS172738 is a novel RET inhibitor and a phase I trial has been initiated with this agent.62
Clinical management
The development of selpercatinib and pralsetinib represents a fundamental change in the treatment of RET + NSCLC as these agents are highly active and well tolerated. The first critical step will be to increase the rate of molecular testing for RET rearrangements, ideally at the time of diagnosis. Clinicians can use RET FISH testing, which represents a single marker testing strategy or as a panel using NGS, by either tumor testing or ctDNA. If testing panels are not available then RET testing could be performed in patients who have tested negative for EGFR, ALK, ROS1 and BRAF V600E because the prevalence RET rearrangements is higher in this clinical situation. Currently, if a RET rearrangement is identified referral to a clinical trial of selpercatinib and pralsetinib is the preferred option, and if trials with these agents are not available a referral to another RET-specific inhibitor trial is an option (Table 3).63 Many of these trials enroll patients with diseases other than NSCLC, and include multiple cohorts depending on disease and previous treatment. Once selpercatinib and pralsetinib become available outside of clinical trials they could be considered for first line therapy. The multi-targeted TKIs remain a potential option if the next generation RET TKIs are not available.
Table 3.
Currently recruiting trials for RET + NSCLC.63
| NCT no. | Agent | Phase | Primary outcome |
|---|---|---|---|
| NCT01639508 | Cabozantinib | 2 | ORR |
| NCT04131543 | Cabozantinib | 2 | ORR |
| NCT03037385 | Pralsetinib (BLU-667) | ½ | Phase I: MTD Phase II: ORR |
| NCT04222972 | Pralsetinib (BLU-667) versus platinum/pemetrexed alone or with pembrolizumab | 3 | PFS |
| NCT03780517 | BOS172738 | 1 | MTD and adverse events |
| NCT03445000 | Alectinib | 2 | ORR |
| NCT02183883 | Alectinib | 2 | PFS |
| NCT03157128 | Selpercatinib (LOXO-292) | 2 | Phase I: MTD Phase II: ORR |
| NCT04161391 | TPX-0046 | 1/2 | Phase I: MTD Phase II: ORR |
| NCT03178552 | Alectinib | 2 | Phase II |
MTD, maximum tolerated dose; NCT, National Clinical Trials; NSCLC, non-small cell lung cancer; ORR, objective response rate; PFS, progression-free survival.
The optimal treatment at the time of disease progression remains ambiguous. Carboplatin and pemetrexed has demonstrated activity and some clinicians may opt to use chemotherapy alone since RET + NSCLC patients have clinical characteristics associated with less benefit from immunotherapy. Patients with RET + NSCLC were not excluded from the trial of carboplatin, pemetrexed and pembrolizumab so this combination is also an option. Some clinicians may extrapolate from the results of the EGFR mutation subset analysis, and preferentially use the combination of carboplatin, paclitaxel, bevacizumab, and atezolizumab. Most likely all three options will be used, and the selection of therapy will be based on physician and patient preference.
Future directions
One inherent challenge with this rare molecular subset is that performing prospective phase III trials is difficult and time consuming, and once an agent has shown promising activity patients and physicians may not have equipoise. In EGFR mutant and ALK rearranged NSCLC phase III trials demonstrated the superiority of targeted therapy compared to platinum-based chemotherapy. A phase III trial of pralsetinib compared to chemotherapy with carboplatin and pemetrexed alone or with pembrolizumab, has been initiated.63 Global registries may have a critical role in this situation because they can be designed to collect specific clinical data, and participation would be less labor intensive than participation in a clinical trial. These registries would provide a better assessment of outcomes than retrospective studies.
With the use of more potent RET inhibitors it is inevitable that mechanisms of acquired resistance will develop, and based on other targeted therapies the prevalence of resistance mutations will increase.64 Some patients may have upregulation of bypass tracks and develop ‘RET independent’ mechanisms of resistance. Biopsies or ctDNA at the time of disease progression will be important to assess the mechanisms of resistance, and develop the next generation RET TKIs.
Footnotes
Funding: The author disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research funding for clinical trials (institution): Genentech/Roche, Blueprint Medicines, Merck, Astra Zeneca, Takeda, Advaxis, Regeneron.
Conflict of interest statement: Consulting or advisory board (personal): Takeda, Astra Zeneca, Genentech/Roche, GI Therapeutics, Foundation Medicine, Pfizer, EMD Serono, Novartis, Lilly.
References
- 1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin 2019; 69: 7–34. [DOI] [PubMed] [Google Scholar]
- 2. Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Abate D, et al. Global Burden of Disease Cancer Collaboration. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2017: a systematic analysis for the global burden of disease study. JAMA Oncol 2019; 5: 1749–1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Govindan R, Page N, Morgensztern D, et al. Changing epidemiology of small-cell lung cancer in the United States over the last 30 years: analysis of the surveillance, epidemiologic, and end results database. J Clin Oncol 2006; 24: 4539–4544. [DOI] [PubMed] [Google Scholar]
- 4. Sandler A, Gray R, Perry MC, et al. Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med 2006; 355: 2542–2550. [DOI] [PubMed] [Google Scholar]
- 5. Johnson DH, Fehrenbacher L, Novotny WF, et al. Randomized phase II trial comparing bevacizumab plus carboplatin and paclitaxel with carboplatin and paclitaxel alone in previously untreated locally advanced or metastatic non-small-cell lung cancer. J Clin Oncol 2004; 22: 2184–2191. [DOI] [PubMed] [Google Scholar]
- 6. Scagliotti G, Hanna N, Fossella F, et al. The differential efficacy of pemetrexed according to NSCLC histology: a review of two phase III studies. Oncologist 2009; 14: 253–263. [DOI] [PubMed] [Google Scholar]
- 7. Mok TS, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med 2009; 361: 947–957. [DOI] [PubMed] [Google Scholar]
- 8. Soda M, Choi YL, Enomoto M, et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature 2007; 448: 561–566. [DOI] [PubMed] [Google Scholar]
- 9. Kwak EL, Bang YJ, Camidge DR, et al. Anaplastic lymphoma kinase inhibition in non-small-cell lung cancer. N Engl J Med 2010; 363: 1693–1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Shaw AT, Ou SH, Bang YJ, et al. Crizotinib in ROS1-rearranged non-small-cell lung cancer. N Engl J Med 2014; 371:1963–1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Drilon A, Siena S, Dziadziuszko R, et al. Entrectinib in ROS1 fusion-positive non-small-cell lung cancer: integrated analysis of three phase 1-2 trials. Lancet Oncol 2020; 21: 261–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Drilon A, Clark JW, Weiss J, et al. Antitumor activity of crizotinib in lung cancers harboring a MET exon 14 alteration. Nat Med 2020; 26: 47–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Drilon A, Laetsch TW, Kummar S, et al. Efficacy of larotrectinib in TRK fusion-positive cancers in adults and children. N Engl J Med 2018; 378: 731–739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Planchard D, Besse B, Groen HJM, et al. Dabrafenib plus trametinib in patients with previously treated BRAF(V600E)-mutant metastatic non-small cell lung cancer: an open-label, multicentre phase 2 trial. Lancet Oncol 2016; 17: 984–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lindeman NI, Cagle PT, Aisner DL, et al. Updated molecular testing guideline for the selection of lung cancer patients for treatment with targeted tyrosine kinase inhibitors: guideline from the college of American pathologists, the international association for the study of lung cancer, and the association for molecular pathology. J Thorac Oncol 2018; 13: 323–358. [DOI] [PubMed] [Google Scholar]
- 16. Takahashi M, Ritz J, Cooper GM. Activation of a novel human transforming gene, RET, by DNA rearrangement. Cell 1985; 42: 581–588. [DOI] [PubMed] [Google Scholar]
- 17. Lipson D, Capelletti M, Yelensky R, et al. Identification of new ALK and RET gene fusions from colorectal and lung cancer biopsies. Nat Med 2012; 18: 382–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yoh K, Seto T, Satouchi M, et al. Vandetanib in patients with previously treated RET-rearranged advanced non-small-cell lung cancer (LURET): an open-label, multicentre phase 2 trial. Lancet Respir Med 2017; 5: 42–50. [DOI] [PubMed] [Google Scholar]
- 19. Wang R, Hu H, Pan Y, et al. RET fusions define a unique molecular and clinicopathologic subtype of non-small-cell lung cancer. J Clin Oncol 2012; 30: 4352–4435. [DOI] [PubMed] [Google Scholar]
- 20. Kohno T, Ichikawa H, Totoki Y, et al. KIF5B-RET fusions in lung adenocarcinoma. Nat Med 2012; 18: 375–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Takeuchi K, Soda M, Togashi Y, et al. RET, ROS1 and ALK fusions in lung cancer. Nat Med 2012; 18: 378–381. [DOI] [PubMed] [Google Scholar]
- 22. Gainor JF, Shaw AT. Novel targets in non-small cell lung cancer: ROS1 and RET fusions. Oncologist 2013; 18: 865–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Drilon A, Hu ZI, Lai GGY, et al. Targeting RET-driven cancers: lessons from evolving preclinical and clinical landscapes. Nat Rev Clin Oncol 2018; 15: 151–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mizukami T, Shiraishi K, Shimada Y, et al. Molecular mechanisms underlying oncogenic RET fusion in lung adenocarcinoma. J Thorac Oncol 2014; 9: 622–630. [DOI] [PubMed] [Google Scholar]
- 25. Gautschi O, Milia J, Filleron T, et al. Targeting RET in patients with RET-rearranged lung cancers: results from the global, multicenter RET registry. J Clin Oncol 2017; 35: 1403–1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ferrara R, Auger N, Auclin E, et al. Clinical and translational implications of RET rearrangements in non-small cell lung cancer. J Thorac Oncol 2018; 13: 27–45. [DOI] [PubMed] [Google Scholar]
- 27. Ju YS, Lee WC, Shin JY, et al. A transforming KIF5B and RET gene fusion in lung adenocarcinoma revealed from whole-genome and transcriptome sequencing. Genome Res 2012; 22: 436–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Qian Y, Chai S, Liang Z, et al. KIF5B-RET fusion kinase promotes cell growth by multilevel activation of STAT3 in lung cancer. Mol Cancer 2014; 13: 176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Go H, Jung YJ, Kang HW, et al. Diagnostic method for the detection of KIF5B-RET transformation in lung adenocarcinoma. Lung Cancer 2013; 82: 44–50. [DOI] [PubMed] [Google Scholar]
- 30. Tsuta K, Kohno T, Yoshida A, et al. RET-rearranged non-small-cell lung carcinoma: a clinicopathological and molecular analysis. Br J Cancer 2014; 110: 1571–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Borrelli N, Giannini R, Proietti A, et al. KIF5B/RET fusion gene analysis in a selected series of cytological specimens of EGFR, KRAS and EML4-ALK wild-type adenocarcinomas of the lung. Lung Cancer 2013; 81: 377–381. [DOI] [PubMed] [Google Scholar]
- 32. Pan Y, Zhang Y, Li Y, et al. ALK, ROS1 and RET fusions in 1139 lung adenocarcinomas: a comprehensive study of common and fusion pattern-specific clinicopathologic, histologic and cytologic features. Lung Cancer 2014; 84: 121–126. [DOI] [PubMed] [Google Scholar]
- 33. Leighl NB, Page RD, Raymond VM, et al. Clinical utility of comprehensive cell-free DNA analysis to identify genomic biomarkers in patients with newly diagnosed metastatic non-small cell lung cancer. Clin Cancer Res 2019; 25: 4691–4700. [DOI] [PubMed] [Google Scholar]
- 34. Beaubier N, Bontrager M, Huether R, et al. Integrated genomic profiling expands clinical options for patients with cancer. Nat Biotechnol 2019; 37: 1351–1360. [DOI] [PubMed] [Google Scholar]
- 35. Benayed R, Offin M, Mullaney K, et al. High yield of RNA sequencing for targetable kinase fusions in lung adenocarcinomas with no mitogenic driver alteration detected by DNA sequencing and low tumor mutation burden. Clin Cancer Res 2019; 25: 4712–4722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Drilon A, Hu ZI, Lai GGY, et al. Targeting RET-driven cancers: lessons from evolving preclinical and clinical landscapes. Nat Rev Clin Oncol 2018; 15: 151–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lee SH, Lee JK, Ahn MJ, et al. Vandetanib in pretreated patients with advanced non-small cell lung cancer-harboring RET rearrangement: a phase II clinical trial. Ann Oncol 2017; 28: 292–297. [DOI] [PubMed] [Google Scholar]
- 38. Drilon A, Rekhtman N, Arcila M, et al. Cabozantinib in patients with advanced RET-rearranged non-small-cell lung cancer: an open-label, single-centre, phase 2, single-arm trial. Lancet Oncol 2016; 17: 1653–1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hida T, Velcheti V, Reckamp KL, et al. A phase 2 study of lenvatinib in patients with RET fusion-positive lung adenocarcinoma. Lung Cancer 2019; 138: 124–130. [DOI] [PubMed] [Google Scholar]
- 40. Drilon A, Fu S, Patel MR, et al. A phase I/Ib trial of the VEGFR-sparing multikinase RET inhibitor RXDX-105. Cancer Discov 2019; 9: 384–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Yanagitani N, Takeuchi S, Takahara S, Alectinib in, et al. previously treated RET-rearranged advanced non-small-cell lung cancer: a phase 1/2 trial (ALL-RET). In: The 2019 World Conference on Lung Cancer, Barcelona, Spain, 7–10 September 2019 Abstract OA0201. [Google Scholar]
- 42. Wozniak A. RXDX105. 2020 Targeted Therapies of Lung Cancer Meeting, Santa Monica, CA, USA, 19–22 February 2020. [Google Scholar]
- 43. Lin JJ, Kennedy E, Sequist LV, et al. Clinical activity of alectinib in advanced RET-rearranged non-small cell lung cancer. J Thorac Oncol 2016; 11: 2027–2032. [DOI] [PubMed] [Google Scholar]
- 44. Horiike A, Takeuchi K, Uenami T, et al. Sorafenib treatment for patients with RET fusion-positive non-small cell lung cancer. Lung Cancer 2016; 93: 43–46. [DOI] [PubMed] [Google Scholar]
- 45. Gozgit JM, Chen TH, Song Y, et al. RET fusions observed in lung and colorectal cancers are sensitive to ponatinib. Oncotarget 2018; 9: 29654–29664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Drilon A, Bergagnini I, Delasos L, et al. Clinical outcomes with pemetrexed-based systemic therapies in RET-rearranged lung cancers. Ann Oncol 2016; 27: 1286–1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Mazieres J, Drilon A, Lusque A, et al. Immune checkpoint inhibitors for patients with advanced lung cancer and oncogenic driver alterations: results from the IMMUNOTARGET registry. Ann Oncol 2019; 30: 1321–1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Offin M, Guo R, Wu SL, et al. Immunophenotype and response to immunotherapy of RET-rearranged lung cancers. JCO Precis Oncol 2019; 3: 10.1200/PO.1800386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Gandhi L, Rodriguez-Abreu D, Gadgeel S, et al. Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med 2018; 378: 2078–2092. [DOI] [PubMed] [Google Scholar]
- 50. Paz-Ares L, Luft A, Vicente D, et al. Pembrolizumab plus chemotherapy for squamous non-small-cell lung cancer. N Engl J Med 2018; 379: 2040–2051. [DOI] [PubMed] [Google Scholar]
- 51. Socinski MA, Jotte RM, Cappuzzo F, et al. Atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N Engl J Med 2018; 378: 2288–2301. [DOI] [PubMed] [Google Scholar]
- 52. Reck M, Shankar G, Lee A, et al. Atezolizumab in combination with bevacizumab, paclitaxel and carboplatin for the first-line treatment of patients with metastatic non-squamous non-small cell lung cancer, including patients with EGFR mutations. Expert Rev Respir Med 2020; 14: 125–136. [DOI] [PubMed] [Google Scholar]
- 53. Subbiah V, Velcheti V, Tuch BB, et al. Selective RET kinase inhibition for patients with RET-altered cancers. Ann Oncol 2018; 29: 1869–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Evans E, Hu W, Cao F, et al. BLU-667 demonstrates robust activity in RET fusion-driven intracranial tumor models. In: The 2019 World Conference on Lung Cancer, Barcelona, Spain, 7–10 September 2019. Abstract P2.03-44. [Google Scholar]
- 55. Gainor JF, Lee DH, Curigliano G, et al. Clinical activity and tolerability of BLU-667, a highly potent and selective RET inhibitor, in patients (pts) with advanced RET-fusion+ non-small cell lung cancer (NSCLC). J Clin Oncol 2019; 37 (Suppl. 15): Abstract 9008. [Google Scholar]
- 56. Nakaoku T, Kohno T, Araki M, et al. A secondary RET mutation in the activation loop conferring resistance to vandetanib. Nat Commun 2018; 9: 625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Liu X, Shen T, Mooers BHM, et al. Drug resistance profiles of mutations in the RET kinase domain. Br J Pharmacol 2018; 175: 3504–3515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Subbiah V, Gainor JF, Rahal R, et al. Precision targeted therapy with BLU-667 for RET-driven cancers. Cancer Discov 2018; 8: 836–849. [DOI] [PubMed] [Google Scholar]
- 59. Nelson-Taylor SK, Le AT, Yoo M, et al. Resistance to RET-inhibition in RET-rearranged NSCLC is mediated by reactivation of RAS/MAPK signaling. Mol Cancer Ther 2017; 16: 1623–1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Drilon A, Oxnard G, Wirth L, et al. Registrational results of LIBRETTO-001: a phase 1/2 trial of selpercatinib (LOXO-292) in patients with RET fusion-positive lung cancers. In: The 2019 World Conference on Lung Cancer, Barcelona, Spain, 7–10 September 2019. Abstract PL02.08. [Google Scholar]
- 61. Drilon A, Rogers E, Zhai D, et al. TPX-0046 is a novel and potent RET/SRC inhibitor for ret-driven cancers. Ann Oncol 2019; 30 (Suppl. 5): v159–v193. [Google Scholar]
- 62. Schoffski P, Aftimos PG, Massard C, et al. A phase I study of BOS172738 in patients with advanced solid tumors with RET gene alterations including non-small cell lung cancer and medullary thyroid cancer. J Clin Oncol 2019; 37 (Suppl. 15): abstract TPS3162. [Google Scholar]
- 63. ClinicalTrials.gov. Ponatinib in advanced NSCLC w/ RET translocations. 2019. https://clinicaltrials.gov/ct2/show/NCT01813734 (2019; accessed 24 February 2020).
- 64. Solomon BJ, Tan L, Lin JJ, et al. RET solvent front mutations mediate acquired resistance to selective RET inhibition in RET-driven malignancies. J Thorac Oncol 2020; 15: 541–549. https://clinicaltrials.gov/ct2/results?cond=Lung+Cancer&term=RET&cntry=&state=&city=&dist= (accessed 24 February2020) [DOI] [PMC free article] [PubMed] [Google Scholar]