Abstract
Background
Although rotational changes in lower limb alignment after total hip arthroplasty (THA) affect functional stem anteversion, less is known about the effects of femoral rotational alignment in the standing position. This study investigated postoperative changes in femoral rotation and evaluated the association with whole-body alignment in patients who underwent THA.
Methods
Sixty-five patients with unilateral hip osteoarthritis who underwent THA were enrolled. Preoperative and postoperative femoral rotation in the standing and supine positions were measured using EOS 2D/3D X-ray imaging system and computed tomography. Negative and positive changes in femoral rotation angle were indicative of internal and external rotation, respectively. The associations between femoral rotation and preoperative clinical and radiological factors were investigated.
Results
Femoral rotation showed significant internal changes in both the standing (−4.7° ± 11.0°) and supine (−3.5°± 10.9°) positions after THA. The preoperative femoral rotation angle, knee flexion angle, sagittal vertical axis (SVA), lumbar lordosis, body mass index, age, and internal and external rotation angles of the hip range of motion on the contralateral side were significantly correlated with femoral rotation in the standing position after THA. Multiple regression analysis showed that preoperative femoral rotation (β = 0.416, P < .001) and SVA (β = 0.216, P = .040) were significant predictors of postoperative femoral rotation in the standing position.
Conclusions
Femoral rotation had significant association with the patient-inherent posture represented by the SVA in the standing position. Because extensive external change of femoral rotation may increase the risk of hip impingement and dislocation, careful attention is required in patients with external femoral rotation and forward bent posture in the preoperative standing position.
Keywords: Femoral rotation, EOS imaging, Total hip arthroplasty (THA), Hip osteoarthritis (OA), Whole-body alignment
Introduction
Total hip arthroplasty (THA) is an effective orthopaedic procedure for patients with hip disorders, providing excellent long-term clinical outcomes. THA can relieve pain, restore function, and improve quality of life [1]. Appropriate implant positioning that restores the hip center and reduces femoral offset and leg length discrepancy is important for obtaining a good range of motion (ROM) and improving activity [[2], [3], [4], [5]]. Impingement and dislocation remain major complications after THA and may result in early clinical failure requiring revision surgery. A combined anteversion technique, consisting of cup and stem alignment, can optimize the hip ROM and reduce the risk of the impingement or the dislocation after THA [3,[6], [7], [8]].
Although several studies reported the association of changes in spinal alignment [[9], [10], [11]] and functional cup angle [12,13] with an increased risk for hip impingement or dislocation after THA, fewer studies have focused on postoperative changes in lower limb alignment in patients who underwent THA [[14], [15], [16]]. Moreover, changes in axial lower limb alignment have been measured mostly in the supine position because examination of axial lower limb alignment in the standing position requires a 2D-3D matching technique [17,18] or a novel imaging modality such as the EOS system (EOS Imaging, Paris, France) [19,20]. The major advantage of the EOS system is its ability to measure whole-body alignment with low-dose radiation.
The present study investigated changes in femoral rotation in both the standing and supine positions after THA and evaluated the preoperative patient factors predictive of femoral rotation after THA in both positions. Femoral rotation and whole-body alignment were measured using the EOS system in the standing position and computed tomography (CT) images in the supine position.
Materials and methods
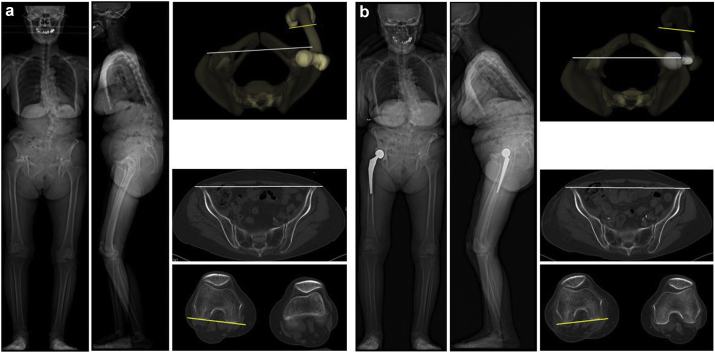
The protocol of this prospective study was approved by the institutional ethical committee of Yokohama City University. Of the 396 hips of patients who had undergone THA between October 2014 and May 2016, 52 women and 13 men of a mean age of 62 years met the criteria for this study. The patients with bilateral osteoarthritis (OA) of the hip, osteonecrosis of the femoral head, rheumatoid arthritis, and subchondral fracture of the femoral head and who have difficulty in keeping the standing position to take EOS were excluded from the study. Finally, we selected 65 patients, 52 women and 13 men, of a mean age of 62 years, who had undergone unilateral THA for unilateral hip OA and agreed to preoperative/postoperative EOS imaging. Of 65 patients, 57 were treated using a mini-direct lateral approach (7- to 10-cm skin incision) [21] and 8 using an anterolateral approach. All patients provided written informed consent. The following femoral prostheses were used in this study: 33 Accolade II stems (Stryker, Mahwah, NJ), 29 SL-PLUS MIA HA stems (Smith and Nephew, Memphis, TN), 2 Polar stems (Smith and Nephew), and 1 SMF stem (Smith and Nephew). The surgeons selected prostheses in an attempt to optimize each patient’s kinematics based on preoperative radiographs. Acetabular prostheses were implanted with the use of combined anteversion technique to reduce the risk of dislocation after THA. Combined cup anteversion and stem antetorsion were determined by the following formula: [cup anteversion + 0.7 × stem antetorsion = 37.3] as reported by Widmer and Zurfluh [22]. EOS images (EOS Imaging, Paris, France) were obtained before and 3 months after THA in the standing position, with patients instructed to stand stationary in a leg straddle position with the right leg in front of the left leg [23] (Fig. 1a-d). Femoral rotation angles in the standing position were measured on EOS images using dedicated software. Femoral rotation was defined as an angle of projection between the posterior bicondylar axis and the line connecting the bilateral anterior superior iliac spine to the ground, with negative and positive femoral rotation angles defined as internal and external rotations, respectively (Fig. 1e). All patients underwent CT scanning from the pelvis to the distal end of the femur before and 1 week after THA in the supine position (Siemens SOMATOM Definition AS, 1.5 mm/slice, Germany). Femoral rotation angles in the supine position were measured on CT axial images (Fig. 1f). The femoral anteversion angle was defined as the angle between a line passing through the centers of the femoral head and neck and a line passing through the posterior aspect of the femoral condyles [24].
Figure 1.
EOS imaging system for the production of 3D whole-body image. (a-d): frontal (a) and lateral (b) whole-body images obtained by EOS in the standing position. Using dedicated software, these images were converted to 3D images to measure whole-body alignments (c and d). (e and f): Measurement of the femoral rotation angle, defined as the angle between the posterior bicondylar axis and the line connecting ASIS, by an EOS imaging system in the standing position (e) and by CT scans in the supine position (f). ASIS, anterior superior iliac spine.
Patient factors associated with changes in femoral rotation from before to after THA were evaluated by univariate and multivariate regression analyses. Patient factors included the age; gender; body mass index (BMI); preoperative Kellgren and Lawrence grade of hip OA [25]; Bombelli classification of OA type [26]; Harris Hip Score [27]; preoperative and postoperative hip ROM (flexion, abduction, adduction, internal rotation and external rotation in the supine position, and extension in the lateral position); insertion angle of stem anteversion; and whole-body alignments, including alignments of the lower limbs and pelvis and global spinal alignments. Lower limb alignments consisted of the functional length of the lower limb, defined as the distance between the center of the femoral head and the central point of the distal articulation of the tibia; femoral offset, defined as the distance between the center of the femoral head and the proximal femoral diaphysis axis; the knee flexion angle, defined as the angle between the femoral mechanical axis and the tibial mechanical axis in the knee sagittal plane; and the percent mechanical axis, defined as the ratio of the distance between the medial proximal end of tibia and the Mikulicz line and the width of the proximal tibia in the frontal plane. Pelvic alignments consisted of the anterior pelvic plane inclination angle, defined as the angle between the vertical axis and the anterior pelvic plane in the standing position; the pelvic tilt, defined as the angle between the line connecting the midpoint of the sacral plate to the center of the axis of both the acetabula and the vertical axis; and the sacral slope, defined as the angle between the sacral plate and the horizontal axis. Spinal alignments consisted of the T1-T12 kyphosis angle (T1/T12), defined as the angle between the upper T1 plate and the lower T12 plate in the sagittal plane; and the L1-S1 lordosis angle (L1/S1), defined as the angle between the upper L1 plate and the tangent to the sacral plate in the sagittal plane. Global spinal alignment was measured using the sagittal vertical axis (SVA), defined as the distance between the posterior edge of the sacral plate and the vertical axis passing through the center of the C7 vertebra in the sagittal plane.
After univariate analysis of the association of each of these factors with femoral rotation before to after THA, 4 factors with P-values < .05 were selected and included in multivariate regression analysis. Associations on multivariate regression analysis were reported as standardized regression coefficients (β) and P-values, with P < .05 indicating statistical significance. All statistical analyses were performed using SPSS, version 16.0 software for Windows (IBM Corp., Japan).
Results
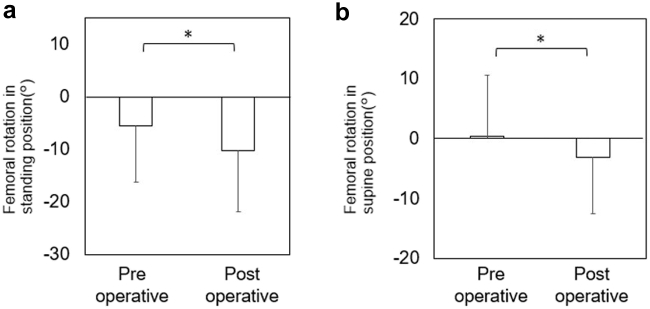
The femoral position showed significant mean internal rotation after THA in both the standing (from −5.5° to −10.2°, P < .05, Fig. 2a) and supine (mean: 0.38° to −3.2°, P < .05, Fig. 2b) positions. There was no significant difference in the mean magnitude of change in the standing and supine positions (4.7° vs 3.5°, P = .43). Of the 65 patients, 43 (66%) had an internal, 21 (32%) had an external, and one (1%) had a neutral femoral rotational position before THA. After THA, 49 (75%) of the 65 patients showed an internal and 15 (23%) showed an external rotational position. Postoperative femoral rotational changes were >10° in 30 (46%) patients and >20° in 3 (5%) patients. There were no patients who experienced hip dislocation during the follow-up period. Histograms of postoperative angular changes in the femoral rotational position showed wide variations (Fig. 3).
Figure 2.
Preoperative and postoperative angles of femoral rotation in the (a) standing and (b) supine positions. Femoral rotation in both positions showed significant internal changes after THA. ∗P < .05, by paired t-tests; error bars denote standard deviations.
Figure 3.
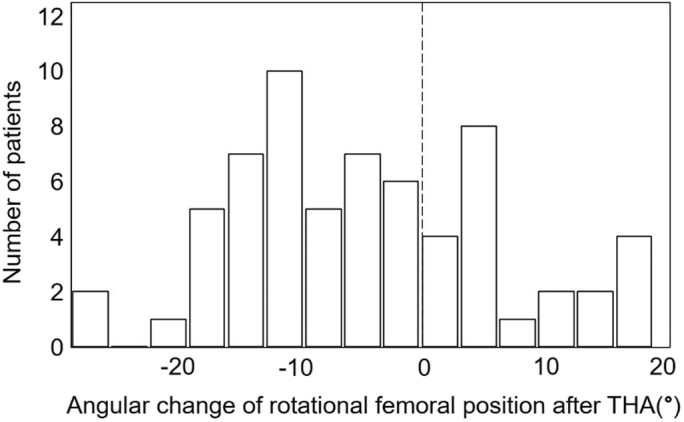
Histogram of angular changes in the rotational femoral position in patients who underwent THA. Most patients showed internal changes in the femoral position after THA, although 19 of 65 (29%) showed external changes.
The correlations of preoperative and postoperative clinical and radiographic data with femoral rotation in the standing position were evaluated using Pearson’s correlation analysis. The SVA (r = 0.388, P = .001) and knee flexion angle (r = 0.271, P = .028) correlated significantly with preoperative femoral rotation in the standing position (Table 1A), whereas the SVA (r = 0.309, P = .006), knee flexion angle (r = 0.311, P = .006), sacral slope (r = −0.241, P = .028), L1/S1 (r = 0.289, P = .01), and stem anteversion (r = −0.268, P = .016) correlated significantly with postoperative femoral rotation in the standing position (Table 1B). External rotation of the femoral position was significantly greater in patients who underwent THA with a forward posture, bent knee, and/or lumbar kyphosis than in patients with upright posture (Fig. 4).
Table 1.
Factors affecting preoperative and postoperative femoral rotation in the standing position.
| A: Preoperative factors affecting preoperative femoral rotation in the standing position | ||
|---|---|---|
| Correlation coefficient (r) | P | |
| SVA | 0.388 | .001 |
| Knee flexion angle | 0.271 | .028 |
| B: Postoperative factors affecting postoperative femoral rotation in the standing position | ||
|---|---|---|
| Correlation coefficient (r) | P | |
| SVA | 0.309 | .006 |
| Knee flexion angle | 0.311 | .006 |
| SS | −0.241 | .03 |
| L1/S1 | 0.289 | .01 |
| Stem anteversion | −0.268 | .03 |
Figure 4.
A representative patient experiencing external femoral rotation after THA. A 79-year-old woman with a forward-bending, knee flexion posture experienced a change from an internal femoral position (−4.7°) before THA (a) to an external femoral position (7.7°) after THA (b). Before and after THA, her knee flexion angles were 22.2° and 21.6°, respectively, and her SVA were 141 mm and 213 mm, respectively.
Univariate regression analysis showed that preoperative femoral rotation (r = 0.516 P < .001), knee flexion (r = 0.313 P = .006), the internal (r = −0.217, P = .044) and external (r = −0.235, P = .032) rotation angles of the hip ROM on the contralateral side, the age (r = 0.268, P = .016), BMI (r = 0.282 P = .012), SVA (r = 0.353, P = .002), and L1/S1 (r = −0.249 P = .023) were significantly associated with postoperative femoral rotation in the standing position (Table 2A). Among these significant factors, we selected preoperative femoral rotation, the SVA, the BMI, and the knee flexion angle as the explanatory variables in the multivariate analysis for the prediction of postoperative standing femoral rotation based on the value of correlation coefficient and clinical importance. Multiple regression analysis revealed that preoperative femoral rotation (β = 0.416, P < .001) and the SVA (β = 0.216, P = .04) significantly affected postoperative femoral rotation in the standing position. The final regression formula for postoperative femoral rotation in the standing position was as follows: postoperative femoral rotation in the standing position = −18.72 + (0.460 × preoperative femoral rotation) + (0.071 × SVA) (Table 2B).
Table 2.
Association of preoperative patient factors with postoperative femoral rotation in standing and supine position.
| A. Univariate analysis of correlations between preoperative patient factors and postoperative femoral rotation in the standing position | ||
|---|---|---|
| Correlation coefficient (r) | P | |
| Preoperative femoral rotation | 0.516 | <.001 |
| Knee flexion | 0.313 | .006 |
| Internal rotation of hip | −0.217 | .04 |
| External rotation of hip | −0.235 | .03 |
| Age | 0.268 | .02 |
| BMI | 0.282 | .01 |
| SVA | 0.353 | .002 |
| L1/S1 | −0.249 | .02 |
| B. Multivariate analysis of correlations between preoperative patient factors and postoperative femoral rotation in the standing position | ||||
|---|---|---|---|---|
| Adjusted R2 | B | β | P | |
| Constant | 0.369 | −18.72 | .002 | |
| Preoperative femoral rotation | 0.460 | 0.416 | <.001 | |
| SVA | 0.071 | 0.216 | .04 | |
| C. Multivariate analysis of correlations between preoperative patient factors and postoperative femoral rotation in the supine position | ||||
|---|---|---|---|---|
| Adjusted R2 | B | β | P | |
| Constant | 0.241 | −0.381 | .80 | |
| Preoperative femoral rotation | 0.386 | 0.415 | .001 | |
| Stem anteversion | −0.196 | −0.334 | .004 | |
Univariate regression analyses also revealed that preoperative femoral rotation (r = 0.397, P = .001), stem anteversion (r = −0.439, P < .001), age (r = 0.231, P = .03), and functional length of the lower limb (r = −0.215, P = .04) are the significant factors associated with postoperative femoral rotation in the supine position. Using 4 factors described previously as the explanatory variables, multiple regression analyses for prediction of postoperative femoral rotation yielded the following formula: Postoperative femoral rotation in the supine position = −0.381 + (0.386 × preoperative femoral rotation) − (0.196 × stem anteversion) (Table 2C).
The final regression formula and positive correlation between preoperative and postoperative femoral rotation (r = 0.516, P < .01) demonstrated that the widely variable preoperative femoral rotation converged to a mean small variation after THA (Fig. 5).
Figure 5.

Correlation between preoperative and postoperative femoral rotation angles in the standing position (r = 0.516, P < .01).
Discussion
Extensive changes in femoral rotation may increase the risks of bone and implant impingement because of functional increases or decreases in stem anteversion. However, femoral rotation after THA had not been previously investigated. The present study quantified postoperative femoral rotation angles, finding that, after THA, 76% of patients had an internal femoral rotational position in the standing position. These findings indicated that there is little need to pay attention to changes in femoral rotation in most patients because internal changes of the femur were less likely to cause anterior dislocation in the standing position. By contrast, 15 (23%) patients had external femoral rotational positions in the standing position after THA, with one of these patients having an external rotational position >10°. There have been no reports that demonstrated the relation between the femoral rotation and the hip impingement or dislocation; however, the excessive external rotation of the femur will increase the risk of the hip impingement or dislocation because of an increase in functional combined anteversion.
The femoral rotation angle after THA is correlated with clinical background, hip function, surgical intervention, and imaging findings [[14], [15], [16]]. However, the association of femoral rotation with whole-body alignment in the standing position had not been investigated previously. Because the hip joint plays a pivotal role in whole-body alignment in the standing position, the present study analyzed the correlations of spinal, pelvic, and lower limb alignment with femoral rotation. The SVA and knee flexion angle had significant positive correlations with femoral rotation, both before and after THA. Our results showed that a forward-bending and knee-bending posture correlated with the external position of the femur in the standing position. Knee flexion can compensate for the maintaining of sagittal balance by patients with a forward-bending posture [28]. Our findings indicated an external femoral position may compensate, at least in part, for the loss of sagittal balance in patients who had undergone THA.
Multivariate regression analysis was performed to assess the ability of preoperative and intraoperative factors to predict postoperative femoral rotation. Postoperative femoral rotation in the standing position correlated with preoperative femoral rotation and the SVA, whereas postoperative femoral rotation in the supine position correlated with preoperative femoral rotation and stem anteversion. The discrepancy observed between the standing and supine positions may be due to the diminished effect of stem anteversion on femoral rotation in the standing position, resulting from the weight-bearing–induced stabilization of the leg position in this position. In the supine position, the femur may be more flexible, allowing the angle of the stem anteversion to influence femoral rotation. The reduction in the mean value of femoral rotation in the standing position may be explained by surgery-induced reduction of hip contracture.
One limitation of the present study was its focus on short-term changes in femoral rotation after THA. Moreover, postoperative EOS imaging and CT scans were performed at different times. Other limitations were we enrolled only patients who underwent THA via a lateral approach, as the type of surgical approach may affect femoral rotation and no patient in the present study experienced hip dislocation. In addition, the small adjusted R2 values in multivariate analysis may have been due to large interindividual differences in the femoral rotation angle.
Nevertheless, the present study had several advantages. It investigated femoral rotation in both the supine and standing positions, showed that whole-body alignment was associated with femoral rotation, and determined factors predictive of postoperative femoral rotation. Additional studies are required to determine the effect of femoral rotation on clinical outcomes after THA.
Conclusion
The present study showed that internal changes of femoral rotation in the standing position are significant after THA, although 23% of patients who underwent THA experienced an external femoral rotational position, which may increase the risk of hip impingement and anterior dislocation. Femoral rotation correlated with patient-inherent posture represented by the SVA and knee flexion both before and after THA, suggesting that femoral rotation is associated with maintenance of sagittal balance. Preoperative femoral rotation and SVA were significant predictors of postoperative femoral rotation in the standing position.
Conflict of interest
The authors declare there are no conflicts of interest.
Acknowledgments
The authors thank all medical staff members in Yokohama City University.
Supplementary data
References
- 1.Barrack R.L., Paprosky W., Butler R.A. Patients' perception of pain after total hip arthroplasty. J Arthroplasty. 2000;15(5):590. doi: 10.1054/arth.2000.6634. [DOI] [PubMed] [Google Scholar]
- 2.Amstutz H.C., Lodwig R.M., Schurman D.J. Range of motion studies for total hip replacements. A comparative study with a new experimental apparatus. Clin Orthop Relat Res. 1975;111:124. doi: 10.1097/00003086-197509000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Yoshimine F. The safe-zones for combined cup and neck anteversions that fulfill the essential range of motion and their optimum combination in total hip replacements. J Biomech. 2006;39(7):1315. doi: 10.1016/j.jbiomech.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 4.Cichy B., Wilk M., Sliwinski Z. Changes in gait parameters in total hip arthroplasty patients before and after surgery. Med Sci Monit. 2008;14(3):CR159. [PubMed] [Google Scholar]
- 5.Lewinnek G.E., Lewis J.L., Tarr R. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60(2):217. [PubMed] [Google Scholar]
- 6.Hisatome T., Doi H. Theoretically optimum position of the prosthesis in total hip arthroplasty to fulfill the severe range of motion criteria due to neck impingement. J Orthop Sci. 2011;16(2):229. doi: 10.1007/s00776-011-0039-1. [DOI] [PubMed] [Google Scholar]
- 7.Dorr L.D., Malik A., Dastane M. Combined anteversion technique for total hip arthroplasty. Clin Orthop Relat Res. 2009;467(1):119. doi: 10.1007/s11999-008-0598-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ranawat C.S., Maynard M.J. Modern techniques of cemented total hip arthroplasty. Tech Orthop. 1991;6:17. [Google Scholar]
- 9.Yoshimoto H., Sato S., Masuda T. Spinopelvic alignment in patients with osteoarthrosis of the hip: a radiographic comparison to patients with low back pain. Spine (Phila Pa 1976) 2005;30(14):1650. doi: 10.1097/01.brs.0000169446.69758.fa. [DOI] [PubMed] [Google Scholar]
- 10.Radcliff K.E., Orozco F., Molby N. Change in spinal alignment after total hip arthroplasty. Orthop Surg. 2013;5(4):261. doi: 10.1111/os.12076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weng W., Wu H., Wu M. The effect of total hip arthroplasty on sagittal spinal-pelvic-leg alignment and low back pain in patients with severe hip osteoarthritis. Eur Spine J. 2016;25(11):3608. doi: 10.1007/s00586-016-4444-1. [DOI] [PubMed] [Google Scholar]
- 12.Inaba Y., Kobayashi N., Suzuki H. Preoperative planning for implant placement with consideration of pelvic tilt in total hip arthroplasty: postoperative efficacy evaluation. BMC Musculoskelet Disord. 2016;17:280. doi: 10.1186/s12891-016-1120-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Suzuki H., Endo K., Mizuochi J. Sagittal lumbo-pelvic alignment in the sitting position of elderly persons. J Orthop Sci. 2016;21(6):713. doi: 10.1016/j.jos.2016.06.015. [DOI] [PubMed] [Google Scholar]
- 14.Uemura K., Takao M., Sakai T. The validity of using the posterior condylar line as a rotational reference for the femur. J Arthroplasty. 2016;31(1):302. doi: 10.1016/j.arth.2015.08.038. [DOI] [PubMed] [Google Scholar]
- 15.Tezuka T., Inaba Y., Kobayashi N. The influence of patient factors on femoral rotation after total hip arthroplasty. BMC Musculoskelet Disord. 2018;19(1):189. doi: 10.1186/s12891-018-2110-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Akiyama K., Nakata K., Kitada M. Changes in axial alignment of the ipsilateral hip and knee after total hip arthroplasty. Bone Joint J. 2016;98-B(3):349. doi: 10.1302/0301-620X.98B3.35468. [DOI] [PubMed] [Google Scholar]
- 17.Takao M., Nishii T., Sakai T. Application of a CT-3D fluoroscopy matching navigation system to the pelvic and femoral regions. Comput Aided Surg. 2012;17(2):69. doi: 10.3109/10929088.2012.654823. [DOI] [PubMed] [Google Scholar]
- 18.Zheng G., Zhang X. Computer assisted determination of acetabular cup orientation using 2D-3D image registration. Int J Comput Assist Radiol Surg. 2010;5(5):437. doi: 10.1007/s11548-010-0407-x. [DOI] [PubMed] [Google Scholar]
- 19.Wybier M., Bossard P. Musculoskeletal imaging in progress: the EOS imaging system. Joint Bone Spine. 2013;80(3):238. doi: 10.1016/j.jbspin.2012.09.018. [DOI] [PubMed] [Google Scholar]
- 20.Illes T., Somoskeoy S. The EOS imaging system and its uses in daily orthopaedic practice. Int Orthop. 2012;36(7):1325. doi: 10.1007/s00264-012-1512-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Inaba Y., Kobayashi N., Yukizawa Y. Little clinical advantage of modified Watson-Jones approach over modified mini-incision direct lateral approach in primary total hip arthroplasty. J Arthroplasty. 2011;26(7):1117. doi: 10.1016/j.arth.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 22.Widmer K.H., Zurfluh B. Compliant positioning of total hip components for optimal range of motion. J Orthop Res. 2004;22(4):815. doi: 10.1016/j.orthres.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 23.Dubousset J., Charpak G., Skalli W. [EOS stereo-radiography system: whole-body simultaneous anteroposterior and lateral radiographs with very low radiation dose] Rev Chir Orthop Reparatrice Appar Mot. 2007;93(6 Suppl):141. doi: 10.1016/s0035-1040(07)92729-4. [DOI] [PubMed] [Google Scholar]
- 24.Cibulka M.T. Determination and significance of femoral neck anteversion. Phys Ther. 2004;84(6):550. [PubMed] [Google Scholar]
- 25.Brandt K.D., Fife R.S., Braunstein E.M. Radiographic grading of the severity of knee osteoarthritis: relation of the Kellgren and Lawrence grade to a grade based on joint space narrowing, and correlation with arthroscopic evidence of articular cartilage degeneration. Arthritis Rheum. 1991;34(11):1381. doi: 10.1002/art.1780341106. [DOI] [PubMed] [Google Scholar]
- 26.Saito M., Saito S., Ohzono K. The osteoblastic response to osteoarthritis of the hip. Its influence on the long-term results of arthroplasty. J Bone Joint Surg Br. 1987;69(5):746. doi: 10.1302/0301-620X.69B5.3680335. [DOI] [PubMed] [Google Scholar]
- 27.Mahomed N.N., Arndt D.C., McGrory B.J. The Harris hip score: comparison of patient self-report with surgeon assessment. J Arthroplasty. 2001;16(5):575. doi: 10.1054/arth.2001.23716. [DOI] [PubMed] [Google Scholar]
- 28.Obeid I., Hauger O., Aunoble S. Global analysis of sagittal spinal alignment in major deformities: correlation between lack of lumbar lordosis and flexion of the knee. Eur Spine J. 2011;20(Suppl 5):681. doi: 10.1007/s00586-011-1936-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.