Abstract
Computable biomedical knowledge (CBK) represents an evolving area of health informatics, with potential for rapid translational patient benefit. Health Data Research UK (HDR UK) is the national Institute for Health Data Science, whose aim is to unite the UK’s health data to enable discoveries that improve people’s lives. The three main components include the UK HDR Alliance of data custodians, committed to making health data available for research and innovation purposes for public benefit while ensuring safe use of data and building public trust, the HDR Hubs, as centres of expertise for curating data and providing expert domain-specific services, and the HDR Innovation Gateway (‘Gateway’), providing discovery, accessibility, security and interoperability services. To support CBK developments, HDR UK is encouraging use of open data standards for research purposes, with guidance around areas in which standards are emerging, aims to work closely with the international CBK community to support initiatives and aid with evaluation and collaboration, and has established a phenomics workstream to create a national platform for dissemination of machine readable and computable phenotypical algorithms to reduce duplication of effort and improve reproducibility in clinical studies.
Keywords: health care, medical informatics, information systems
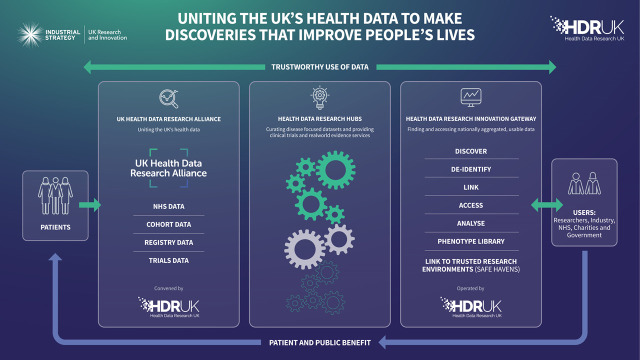
Health Data Research UK (HDR UK) is the national Institute for Health Data Science. Supported by 11 UK-based funders, its aim is to unite the UK’s health data to enable discoveries that improve people’s lives. HDR UK is working in partnership with the public, National Health Service (NHS) bodies, industry, and the charitable sector to make health data available to researchers and innovators to better understand diseases and find ways to prevent, treat and cure them.1 With funding from the UK Government as part of the Industrial Strategy Challenge Fund, HDR UK requirements for a robust UK HDR and innovation infrastructure have been defined, with three key components (figure 1):
Figure 1.
Schematic demonstrating overview of the major components of the Health Data Research UK (HDR UK) structure representing data owners, data services and infrastructure. Underpinning workstreams across all aspects include development of guidance around data standards and models, to improve data quality and interoperability.
UK HDR Alliance (‘Alliance’)—an alliance of data custodians committed to making an unprecedented breadth and depth of health data available for research and innovation purposes for public benefit, while ensuring safe use of data and building public trust.1
HDR Hubs (‘Hubs’)—centres of expertise dedicated to making specific data available, curating data and providing expert domain-specific research services. The Hubs will enable researchers and innovators to collaborate and co-create with colleagues, clinicians and patients to draw insight and understanding from raw and fragmented data.2
HDR Innovation Gateway (‘Gateway’)—an application providing discovery, accessibility, security and interoperability to find data, support linkage and enable health data science to take place in a safe and efficient manner.1
In addition to provision and use of data according to FAIR (Findable, Accessible, Interoperable, Reusable) guiding principles,2 internationally, there is increasing focus on the concept of CBK, specifically regarding how healthcare practices, such as clinical guidelines or care pathways, can be represented in reproducible and computer readable formats.3 This capability is a key component of the development of learning health systems internationally and will underpin successful delivery of the ‘Better care’ priority area of HDR UK, where patients across the UK directly benefit from healthcare decisions informed by large-scale data and advanced analytics embedded in clinical care settings.
In order for such CBK to be determined, evaluated and reproducibly translated to clinical care scenarios, it is essential that the underlying data are recorded, and/or made available, through open standards which promote semantic and technical interoperability. For discrete healthcare data, several such data models/specifications are in common use and freely available including, for example, OMOP (Observational Medical Outcomes Partnership), OpenEHR and FHIR (Fast Healthcare Interoperability Resources), along with associated terminologies/ontologies such as SNOMED-CT (Systematised Nomenclature of Human Medicine Clinical Terms), LOINC (Logical Observation Identifiers Names and Codes) and ICD10 (International Classification of Diseases).
In this regard, HDR UK is therefore supporting mobilising CBK in the UK in three ways.
First, as there is an urgent need to encourage convergence of standards adoption, HDR UK is acting as a clearing house of best practice by working with the NHS to convene the community of health data custodians in the Alliance for Digital Innovation Hubs to encourage use of such standards for secondary use and research purposes. It is also providing leadership and guidance around areas of uncertainty in which standards are emerging.
Second, since at present few standards exist regarding agreed and interoperable representation of CBK, HDR UK will work closely with the international CBK community to support such initiatives and aid with evaluation and collaboration. Possible solutions are emerging, with Openclinical having established a community or users and tools in this domain,4 and with the increasing support for the FHIR specification internationally for clinical care purposes, FHIR release 4 provides support for representing knowledge artefacts for the purpose of improving care, which could include clinical decision support.5 Furthermore, development of appropriate knowledge infrastructure platforms or pipelines have been suggested as key enablers for learning health system maturity, aligning with the HDR UK Better Care priority area, which is one of six science priority areas, seeking to improve people’s lives by equipping health and care professionals and patients with the best possible information with which to make decisions about their care. The vision is that by 2030, patients across the UK will benefit from health and care decisions informed by large-scale data and advanced analytics to identify what will work best for them. The overarching aim of the HDR UK Better Care programme is to support the application of advanced analytics to large-scale, real world data sets to enable continuous, scalable quality improvement in individual healthcare decisions, in a way that is trusted by patients, and health and care professionals and the public.
Finally, HDR UK has established a phenomics/human phenome workstream to create a national platform for dissemination of machine readable and computable phenotypical algorithms, including tools for deployment, to reduce duplication of effort and improve reproducibility in clinical studies. CBK pathways and guidelines will provide maximum value only if patients are accurately identified and phenotyped, with their specific disease characteristics recorded, in order to ensure applicability of the pathway or guideline and facilitate tool evaluation. At present, this process is difficult since data may be collected for a range of purposes, using multiple systems and with variable quality.
In conclusion, the development of interest and activity in the evolving area of CBK is likely to represent an important component of future HDR. HDR UK is working in partnership to drive standards adoption across the UK, to work with key international bodies with an interest in CBK, and creating an open phenomics resource. These activities are closely aligned to wider ongoing HDR UK activities to build a robust UK HDR infrastructure. These efforts will result in significant changes to both future health knowledge management research and provide direct and tangible benefits to patients through improved patient care.
Footnotes
Contributors: All authors have contributed to the conception, drafting and writing of the manuscript in accordance with authorship guidelines.
Funding: This work was supported by Health Data Research UK, which is funded by the UK Medical Research Council, Engineering and Physical Sciences Research Council, Economic and Social Research Council, Department of Health and Social Care (England), Chief Scientist Office of the Scottish Government Health and Social Care Directorates, Health and Social Care Research and Development Division (Welsh Government), Public Health Agency (Northern Ireland), British Heart Foundation and the Wellcome Trust.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Commissioned; internally peer reviewed.
References
- 1. Health Data Research UK HDR UK [Internet]. Available: https://www.hdruk.ac.uk/ [Accessed 5 Nov 2019].
- 2. Wilkinson MD, Dumontier M, Aalbersberg IJJ, et al. The fair guiding principles for scientific data management and stewardship. Sci Data 2016;3:160018 10.1038/sdata.2016.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Adler-Milstein J, Nong P, Friedman CP. Preparing healthcare delivery organizations for managing computable knowledge. Learn Health Syst 2019;3:e10070 10.1002/lrh2.10070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. OpenClinical Knowledge management technologies for healthcare [Internet]. Available: http://www.openclinical.org/ [Accessed 5 Nov 2019].
- 5. HL7.org Clinicalreasoning-knowledge-artifact-representation - FHIR v4.0.1 [Internet]. Available: https://www.hl7.org/fhir/clinicalreasoning-knowledge-artifact-representation.html [Accessed 5 Nov 2019].