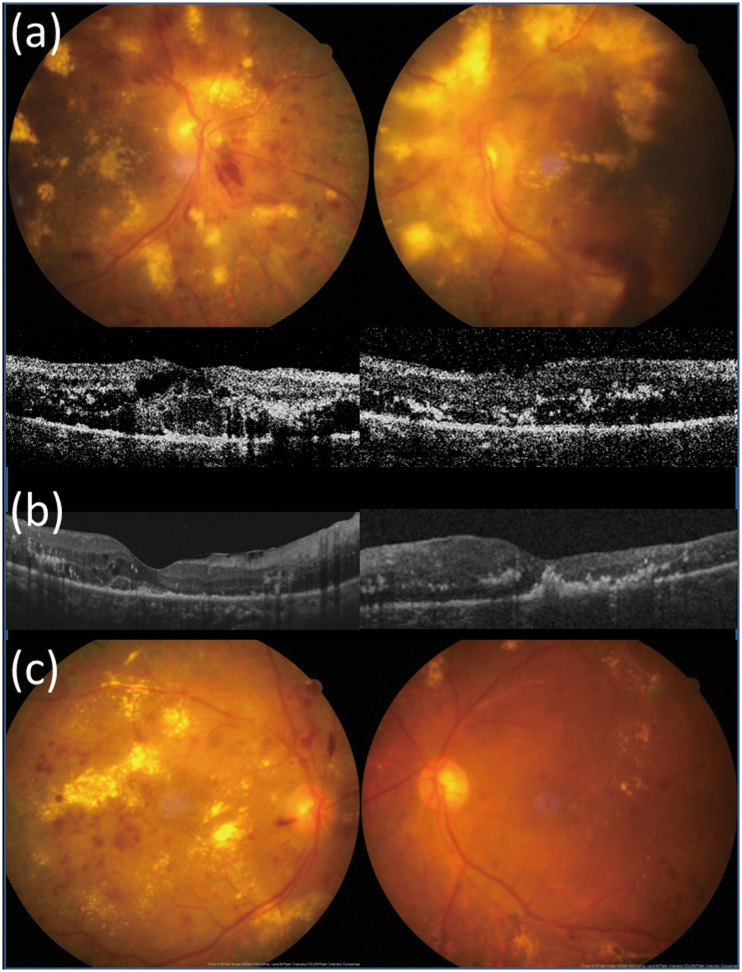
Fig 4. A patient with bilateral DME and massive hard exudates receiving different treatment strategies in both eyes.
(a) A 63-year-old female with hypertension and type 2 diabetes mellitus for 20 years presented with bilateral diabetic macular edema with massive hard exudates, unresponsive to intravitreal bevacizumab injection and macular photocoagulation. Pars plana vitrectomy with internal limiting membrane peeling and focal laser were performed in the left eye. Pre-operative visual acuity (VA) was counting fingers in the left eye and central macular thickness (CRT) was 396 μm. VA in the right eye was 20/200 and CRT was 380 μm at the same time. (b) One month post-operatively, CRT decreased to 296 μm in the left eye. (c) Eight months post-operatively, hard exudates resorbed significantly and VA improved to 20/125 in the left eye. VA of the right eye remained poor (20/400) due to persistent hard exudates despite repeated intravitreal bevacizumab injections, posterior sub-Tenon injections of triamcinolone, and macular laser photocoagulation.