Abstract
Teratomas commonly occur within ovaries, sacrococcygeal regions, testis, mediastinum, and intracranial regions. One of the rare sites for this tumor includes kidneys. Renal anomalies such as horseshoe kidneys with teratoma are one of the extremely rare presentations. The authors present a case of a large teratoma within a horseshoe kidney in an 8-year-old girl whose main clinical manifestation was abdominal distension. Intrarenal teratoma within horseshoe kidneys is a rare and interesting clinical entity that would require an appropriate therapeutic approach to salvage the kidneys and remove the mass.
Keywords: Renal teratoma, Horseshoe kidney
Abbreviations: CT, computed tomography; MRI, Magnetic resonance imaging
Background
More common sites for teratomas include the gonads, mediastinum, retroperitoneum, sacrococcygeal region, and the pineal gland [1]. The kidneys are considered extremely rare sites for teratomas [1,2]. Renal congenital anomalies such as horseshoe kidney or duplicated collecting system are uncommonly seen harboring a renal teratoma [3]. The occurrence of tumors in the horseshoe kidneys is considered extremely rare [4]. The authors attempt to present a pediatric patient with intrarenal teratoma in a horseshoe kidney.
Case presentation
An 8-year-old girl complaining of chronic abdominal distention was referred to the radiology department to undergo an abdominal computed tomography (CT) scan. No urine analysis or blood tests were performed since the primary concern was abdominal distension and the patient was specifically sent for an abdominal CT scan. There was no pertinent prior medical, family, and psycho-social history including any genetic predisposition. No pertinent prior interventions were noted. A contrast-enhanced abdominal CT scan was performed on a 128-slice Siemens scanner. The images revealed communicating lower poles of both kidneys consistent with a horseshoe kidney (Fig. 1). There was a large complex mass arising from the right aspect of the horseshoe kidney. The claw sign and embedded sign were demonstrated implying the origin of the lesion from the kidney (Fig. 2). The mass demonstrated gross dense calcifications with cystic spaces and a considerable amount of fat components (Fig. 3). It measured 17 cm × 11.7 cm × 12 cm in craniocaudal, anteroposterior, and transverse dimensions respectively. There was a significant mass effect resulting in the displacement of bowel loops without obstruction. The liver was also slightly displaced antero-superiorly. The lesion was exerting mass effect on the portal vein. The lesion crossed the midline resulting in a slight rightward displacement of the abdominal aorta. No invasion of the aforementioned vessels was detected. There were no findings to suggest osseous or soft tissue metastatic disease (Fig. 4).
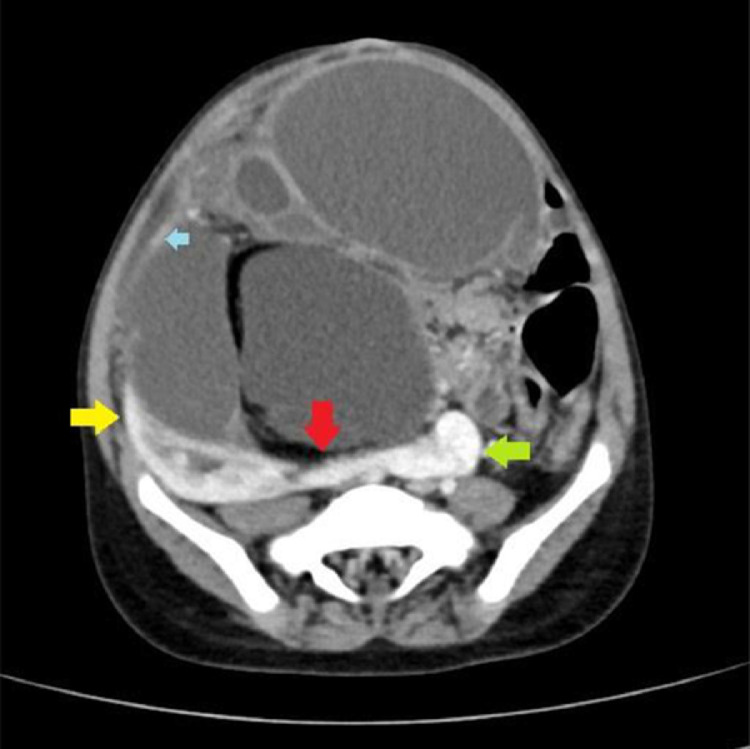
Fig. 2.
Contrast-enhanced abdomen selected axial image: horseshoe kidney, the right aspect of the horseshoe kidney (yellow arrow), the isthmus (red arrow), and the left aspect of the horseshoe kidney (green arrow). Acute angles on either side of the mass are noted with surrounding normal renal parenchyma (blue arrow) consistent with the claw sign. Color version available online.
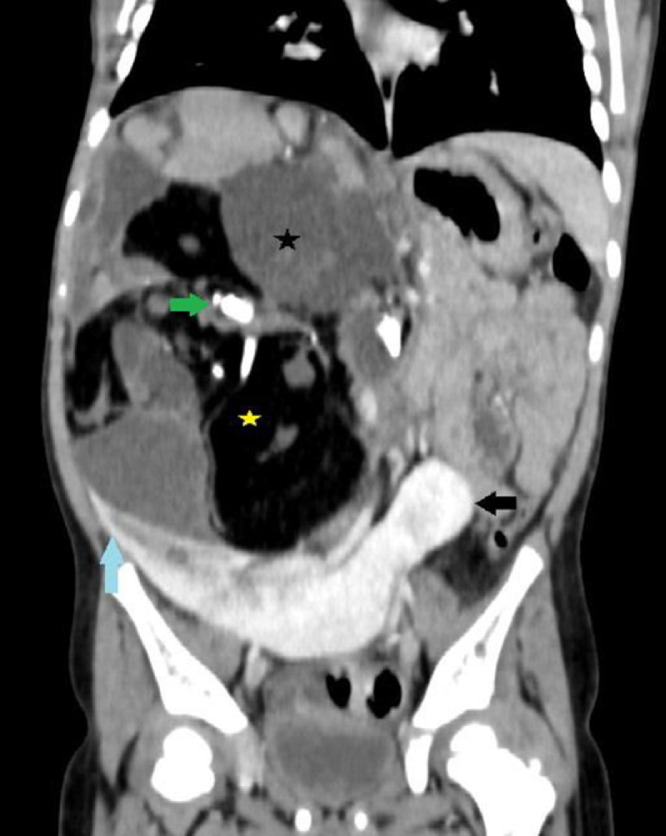
Fig. 3.
Contrast-enhanced abdomen selected coronal image: Right aspect of the horseshoe kidney (blue arrow) and lower pole of the left aspect of the horseshoe kidney (black arrow). Teratoma arising from the right aspect with dense calcifications (green arrow) and fatty components (yellow asterisk). Acute angles are demonstrated between the teratoma and horseshoe kidney consistent with a “claw sign.” The black asterisk is over a dense component of the mass. It may be partly fluid and partly soft tissue given some enhancement inferiorly. Color version available online.
Fig. 1.
(A) Axial contrast-enhanced abdomen selected image: large lesion in the right side with fatty components (white arrow), dense irregular calcifications (green arrow). Anteriorly and contralaterally displaced bowel loops. The upper pole of the left kidney is also shown (open black arrow). Color version available online.
Fig. 4.
Contrast-enhanced abdomen selected sagittal image: The lower pole of the right aspect of horseshoe kidney demonstrated claw sign (brown arrow), dense calcifications (blue asterisk), fat components (green asterisk) and displaced bowel loops anteriorly (black arrow). Color version available online.
After establishing the diagnosis, the patient was transferred to another facility for further management.
Discussion and conclusion
Intrarenal teratomas are extremely rare [2,5] and only 20 case reports have been reported in the literature from 1934 to 2004. Out of these cases, only 5 had associated congenital abnormalities such as horseshoe kidney, prune belly syndrome, and duplicated collecting system [6]. Few more case reports have been reported in the literature in recent years bringing the total to approximately thirty. The latest renal teratoma was described by Balanji et al in 2018 where they found a mature teratoma within the renal pelvis [7]. The most common location for teratomas are as follows: 40% in sacrococcygeal region, 25% in ovary, 18% in mediastinum and neck, 12% in testis, and 5% in brain tissues [5,8]. Its occurrence is considered less than 5% in the abdomen [5]. Mc Curdy explained the first case of teratoma in 1934 in a patient with prune belly syndrome [5,9]. There is no literature evidence for gender or side predilection in renal teratomas. There is a bimodal distribution of the retroperitoneal teratomas with a peak seen in the first 6 months of life and the second peak in early adulthood [5]. Teratomas are considered congenital tumors since they are present birth or discovered prenatally [5]. Germ cell tumors are subdivided into 5 subgroups which include teratomas, yolk sac tumors, choriocarcinomas, embryonal carcinomas, and germinomas [7]. Embryologically, the origin of teratoma comes from all 3 germ layers [7,9]. Epidermoid and dermoid cysts are both derived from ectoderm and ectodermal inclusion cysts. Epidermoid cysts are lined only by squamous epithelium but dermoid cysts have complex tissue [10]. On histological basis, teratomas can be classified as mature or immature. Well-differentiated tissues such as dermal appendages, teeth, and nervous tissues, [9] cartilage with bronchial structures, and bronchial glands are more likely to be present in a mature teratoma, [5] while there are primitive neuroepithelial elements in immature teratomas [7,9]. Immature teratomas typically demonstrate larger intralesional solid components as opposed to mature teratomas [7]. The occurrence of immature renal teratomas is extremely rare as there are only 3 reported cases in the pediatric literature [11]. There are a few tumor markers that germ cell tumors produce, for instance, yolk sac tumors produce alpha-fetoprotein, and choriocarcinoma produces B-HCG [7]. Beckwith suggests that a tumor should be termed a “renal teratoma” if it meets the following 2 criteria: (1) The entire lesion should be within the kidney, not outside the renal capsule and distant teratomas should be excluded to rule out metastasis, (2) tumor should exhibit heterotopic organogenesis.” [3,5,11,12]. Patients may present with nonspecific symptoms including abdominal pain, constipation, hematuria, [7, 1] abdominal mass, and anorexia [3,9]. Ultrasound of the abdomen is the first-line imaging investigation [7] that reveals a cystic heterogeneous, complex mass with irregular foci of calcifications within it [6,7]. On a plain radiograph, large abdominal mass can be noted crossing midline with calcifications [6,7] and visualization of teeth or bony components are characteristic of teratoma [7,9]. CT Findings that are in favor of teratoma include adipose tissue, calcifications, or bony components [7,13] while complex mass lesion having adipose tissue and wall calcifications are highly suggestive of the cystic type of teratoma [5,7]. The only reported case in which MR imaging was performed, revealed a mass with heterogeneity and low signal intensity [5]. Epidermoid cysts would demonstrate water attenuation in both CT and magnetic resonance imaging examinations in most of the cases. Dermoid cysts would depict negative attenuation of −60 to −90 HU in CT scan demonstrating true adipose tissue and high signal intensity in T1 weighted images in magnetic resonance imaging [10]. Mature teratomas of the kidney are usually benign with no metastatic incidence reported in the literature. In contrast, the metastatic disease has been found in mature teratomas arising from other organs [9]. Complete excision of teratomas is suggested and chemotherapeutic treatment is deemed unnecessary [5]. Surgical excision alone is considered an effective treatment in patients with pure immature teratomas because of 3-year event-free survival (>85%) [1,5]. There is a limited follow-up data available following surgical treatment of intrarenal teratomas.
There is a limited amount of case reports regarding intrarenal teratoma within horseshoe kidneys of which only 5 cases are reported in the literature which were associated with congenital abnormalities.
Footnotes
Note: The authors are submitting the article from Afghanistan; a low-income country and eligible for a publication fee waiver; a policy Elsevier is following. Hence we request for the publication fee waiver if the manuscript is accepted for publication
Competing Interests: The authors declare that they have no competing interests.
Funding: Not applicable.
Acknowledgments: Not applicable.
Ethics Approval and Consent to Participate: The manuscript has got an ethical review exemption from the Ethical Review Committee (ERC) of the authors’ institution (French medical institute for Mothers and Children- {FMIC}) as case reports are exempted from review according to the institutional ethical review committee's policy. Written consent is obtained from the participants for publishing the case.
Consent for Publication: Written informed consent was obtained from the parent for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Availability of Data and Materials: Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study (as this is a case report).
Authors’ Contributions: Both authors have participated sufficiently in the submission and take public responsibility for its content. HH: Selecting the case, supervising, and editing the manuscript. NF: writing and revising the manuscript, selecting the images, and corresponding with the journal. Both authors have read and approved the final manuscript.
References
- 1.Mochizuki K., Ohno Y., Tokai Y., Kanematsu T., Okada M., Kamitamari A. Congenital intrarenal teratoma arising from a horseshoe kidney. J Pediatr Surg. 2006;41(7):1313–1315. doi: 10.1016/j.jpedsurg.2006.03.019. [DOI] [PubMed] [Google Scholar]
- 2.Glazier W.B., Lytton B., Tronic B. Renal teratomas: case report and review of the literature. The Journal of urology. Jan 1980;123(1):98–99. doi: 10.1016/s0022-5347(17)55799-7. [DOI] [PubMed] [Google Scholar]
- 3.Jacob S., Ghosh D., Rawat P., Bhatti W., Singh V.P. Primary intra-renal teratoma associated with renal dysplasia: an unusual entity. Indian J Surg. 2013;75(1):77–79. doi: 10.1007/s12262-011-0356-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Briones J.R., Pareja R.R., Martín F.S., Toniolo G.C., Pérez J.H., Mavrich H.V. Incidence of tumoural pathology in horseshoe kidneys. Eur Urol. 1998;33(2):175–179. doi: 10.1159/000019551. [DOI] [PubMed] [Google Scholar]
- 5.Idrissi-Serhrouchni K., El-Fatemi H., Benhayoun K., Chbani L., Harmouch T., Bouabdellah Y. Primary renal teratoma: a rare entity. Diagnos Pathol. 2013;8(1):107. doi: 10.1186/1746-1596-8-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choi D.J., Wallace E.C., Fraire A.E., Baiyee D. Intrarenal teratoma. Radiographics. 2005;25(2):481–485. doi: 10.1148/rg.252045153. [DOI] [PubMed] [Google Scholar]
- 7.Balaji B.S., Karl I.S. Mature cystic teratoma of renal pelvis: an unusual presentation at an uncommon site. J Indian Assoc Pediatr Surg. 2019;24(3):216. doi: 10.4103/jiaps.JIAPS_114_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dhond A.P., Agrawal S.O., Sirmukaddam S.V., Srinath S., Roplekar P., Desai P.R. Mediastinal teratoma: a case report with review of literature. J Sci Soc. 2016;43(1):57. [Google Scholar]
- 9.Modi J., Modi D., Bachani M., Bachani L. Congenital renal teratoma with cystic dysplasia in a neonate: rare entity. J Clin Neonatol. 2015;4(2):126. [Google Scholar]
- 10.Smirniotopoulos J.G., Chiechi M.V. Teratomas, dermoids, and epidermoids of the head and neck. Radiographics. 1995;15(6):1437–1455. doi: 10.1148/radiographics.15.6.8577967. [DOI] [PubMed] [Google Scholar]
- 11.Zhang X.L., Xu G., Li J.L., Pan S.H., Yan J.J. Renal immature teratoma in a male adult: a case report and literature review. Medicine. 2018;97(35) doi: 10.1097/MD.0000000000012143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Otani M., Tsujimoto S., Miura M., Nagashima Y. Intrarenal mature cystic teratoma associated with renal dysplasia: case report and literature review. Pathol Int. 2001;51(7):560–564. doi: 10.1046/j.1440-1827.2001.01236.x. [DOI] [PubMed] [Google Scholar]
- 13.Wu Y.H., Song B., Xu J., Chen W.X., Zhao X.F., Jia R. Retroperitoneal neoplasms within the perirenal space in infants and children: differentiation of renal and non-renal origin in enhanced CT images. Eur J Radiol. 2010;75(3):279–286. doi: 10.1016/j.ejrad.2010.05.038. [DOI] [PubMed] [Google Scholar]