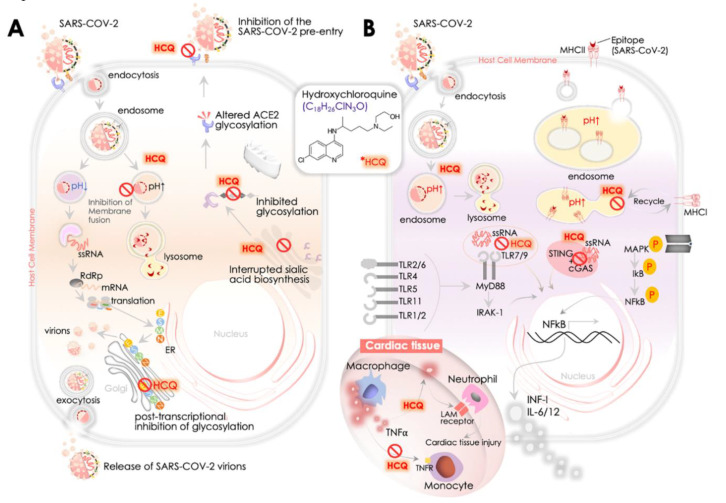
Figure 3.
Hydroxychloroquine (HCQ): SARS-CoV-2 replication and immunomodulatory activities -proposed mechanism. (A) HCQ impacts the binding of SARS-CoV-2 S-protein and ACE2 receptor at the host cell surface by altering the ACE-2 n-terminal glycosylation. HCQ restricts SARS-CoV-2 infection by increasing endosomal pH that disrupts SARS-CoV-2 envelope fusion (requires acidic pH) with endosome membrane phospholipids and subsequent release of its sRNA genome. This is a crucial step that could intervene in its further replication/transcription by RNA-dependent RNA polymerase (RdRp, viz., nsp12) and synthesis of its spike (S), membrane (M), envelope (E), nucleocapsid (N), and nsp3 (a replicase complex component). SARS-CoV-2 infection exploits host cell’s ribosome machinery to synthesize its non-structural proteins (NSPs) that constitutes a replicase-transcriptase complex that is enrolled further to synthesize its sub-genomic RNA. Viral proteins get translated in ER and processed in Golgi before assembling into the nucleocapsid and budding it as a mature virion. HCQ is postulated to alter the maturation of M protein at Golgi, resulting in the collapse of viral assembly. Besides interrupting glycosylation of the ACE2 receptor, HCQ also seems to restrict biosynthesis of the sialic acids that play a part in host cells binding with SARS-CoV-2. The role of HCQ is also implicated in attenuating the activation of mitogen-activated protein (MAP) kinase that could further impact viral replication. (B) HCQ modulates immune function and reduces inflammation. HCQ-led increase in endosomal pH impacts MHC Class I and II antigen cross-presentation. It alters the preparation and development of SARS-CoV-2 Ag-specific T-cells and B-cells. HCQ also impacts the onset of cytokine release from the innate immune system by attenuating DNA/RNA interaction and by activation of cGAS/STING signaling and by disrupting binding to TLR7/9 by increasing the endosomal pH. HCQ impact on these axes further attenuates NFkB nuclear function in promoting the expression of pro-inflammatory cytokine (IFN I, IL-6, IL-12 etc.). In the cardiac tissue, HCQ also attenuates TNFα production in the macrophages and thereby reduces expression of TNFR (TNFα receptor)-1/2 at the membrane of nearby monocytes, which further restricts TNFα’s role in the extravasation of neutrophils that supports opening up the tight junctions of vascular endothelial cells and stimulates leukocyte adhesion molecules (LAM) expression.