Abstract
The coronavirus disease 2019 (COVID-19) pandemic has created many challenges for health care providers. At the forefront is the need to balance optimal patient care with the safety of those providing that care. This is especially true during resuscitations where life-saving procedures cause widespread aerosolization of the virus. Efforts to mitigate this exposure to front-line providers are therefore paramount. We share how we used simulation to prepare our pediatric emergency department for COVID-19 resuscitations.
Key Words: Coronavirus disease 2019, Systems integration, Infection control, Pediatrics
Introduction
The American Heart Association's (AHA) Coronavirus Disease 2019 (COVID-19) guidelines emphasize the need to balance timely, high-quality resuscitation with health care provider safety.1 Safely and rapidly implementing these guidelines may be challenging as the inherent stress that accompanies new algorithms may be compounded by fears of disease transmission and impede understanding and effective execution of new processes.
Simulation may help teams with systems integration.2, 3, 4, 5 Through collaboration and bidirectional feedback, simulation creates a safe analytic lens into spaces and processes so that flow may be optimized and risk minimized. And by encouraging deliberate practice with facilitated feedback prior to actual patient care, simulation educates participants, decreases cognitive load,6 and mitigates errors by increasing individual and team comfort and confidence with high stakes events such as COVID-19 resuscitations.
We used simulation to iteratively develop a COVID-19 resuscitation process for our pediatric emergency department (PED), a 47 bed, Level I Pediatric Trauma center with approximately 60,000 annual PED visits and housed in a free-standing, suburban children's hospital. Our simulations allowed us to collaborate, leverage different perspectives and devise an easily understood, unified resuscitation process that helps protect our team.
Discussion
Simulation to define the current state
Our first step was to assess our current PED space, teams, flow, and processes. We consulted subject matter experts and devised a COVID-19 pediatric resuscitation simulation scenario. Our subject matter experts and administrative leadership joined our simulation as silent observers. Our standard resuscitation team (Table 1 ) was hands-on and managed patient arrival by Emergency Medical Services (EMS), patient resuscitation, and disposition.
Table 1.
Pre-COVID-19 resuscitation staffing model
| Location | Team member | Role |
|---|---|---|
| At the patient stretcher | Team lead physician | Runs the resuscitation |
| Airway provider | Manages airway | |
| Resident or physician assistant | Conducts primary and secondary survey | |
| Respiratory therapist | Assists with airway procedures/management | |
| Bedside nurse | Obtains access, labs, performs procedures | |
| Medication nurse | Draws up medications, fluids | |
| Technician | Places patient on monitor, assists with procedures | |
| Next to the team around the patient stretcher or at the periphery of the room | Documenting nurse | Documents resuscitation in medical record |
| 2nd resident or physician assistant | Computer order entry during resuscitation | |
| Back up respiratory therapist | Assists primary respiratory therapist as needed | |
| Back up technician | Assists primary technician as needed | |
| At doorway or immediately outside the room | Flow supervisor | Assesses needs—asks more staff to enter resuscitation room as needed |
We then debriefed and solicited feedback taking into account all perspectives about PED flow, patient care, personnel safety, and opportunities to minimize contamination risks.
We discovered that our current resuscitation space and path for EMS into that space was not optimal for COVID-19 resuscitations. EMS’ aerosol generating procedures (AGP) would contaminate personnel, equipment, and supplies along the path into our resuscitation rooms. Additionally, these rooms contain copious equipment and supplies that need to be terminally cleaned or discarded after resuscitative AGPs leading to prolonged room turnover time. Also, these rooms are positive pressure. This is not optimal as naturally ventilated or negative pressure rooms are preferred for COVID-19 AGPs.7 , 8
Our simulation also showed that we had to reduce exposure risk, decrease our resuscitation team size, and monitor the number of staff within the resuscitation room. Individual team members had to take on more tasks than usual and we had to be creative within our space. And we needed to do this as quickly as possible prior to our anticipated peak of COVID-19 patients.
We summarized and sorted our simulation findings and feedback according to methods, equipment, supplies, and associates. Our key stakeholders assigned criticality to each item and together we developed potential mitigation options. Based on this, we conducted further simulations to leverage work as imagined with work as done9 to ensure that our mitigation strategies translated to the frontline.
Simulation to develop a new process
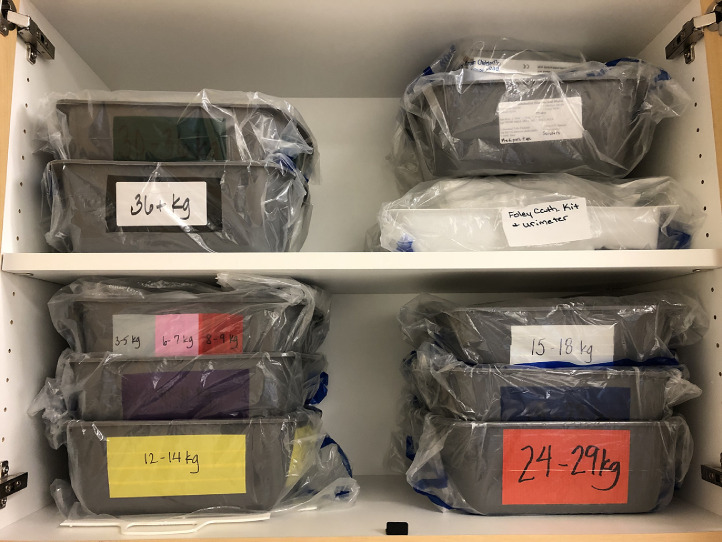
We had to limit contamination from AGPs along EMS’ path into and within our PED. None of our existing negative pressure rooms are near our ambulance entrance. Our decontamination space was ideal as it is next to the ambulance entrance, is physically closed off from the rest of the PED, and has minimal equipment. Since it contained several positive pressure rooms, our facilities team changed airflow into and within one area so that it had negative pressure airflow. We ran simulations trialing different algorithms of bringing in equipment and supplies versus strategically stocking the room. We decided to stock the room with vital airway and vascular access supplies placed in labeled, encased plastic basins presorted according to patient weight following Broselow tape recommendations (Fig. 1 and 2 ). We chose this method as it was the easiest and quickest to reliably clean postresuscitation and still allowed for the use of appropriate weight-based pediatric equipment.
Fig 1.
Cabinet with basins containing supplies presorted according to patient weight.
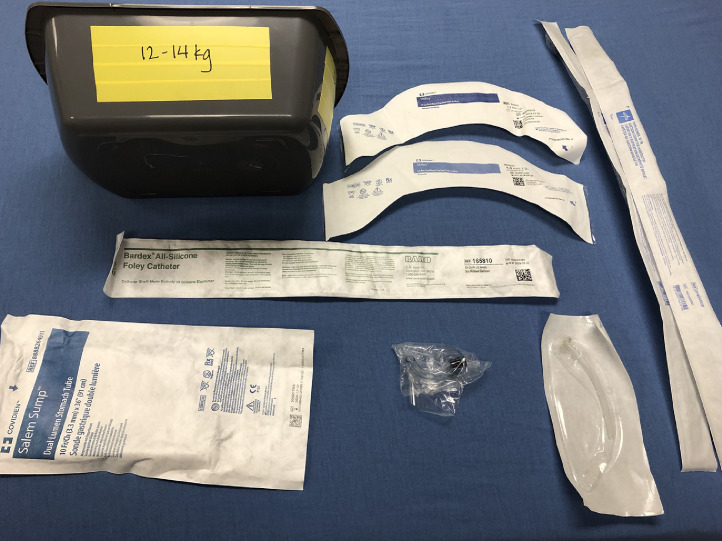
Fig 2.
Each basin contains the following appropriate weight-based supplies: 1 oral airway, 1 nasopharyngeal airway, 2 suction catheters, 2 endotracheal tubes, 1 nasogastric tube, and 1 Foley catheter.
We also used simulation to determine our optimal number of staff around the head of the bed, within the room and outside of the room (Table 2 ).
Table 2.
COVID-19 resuscitation staffing model
| Location | Team member | Role |
|---|---|---|
| At the head of the stretcher | Airway provider | Manages airway. May also function as team lead if PED physician. Conducts primary survey. |
| Respiratory therapist | Places patient on monitor, assists with airway procedures/management and assists with bedside nurse procedures as needed. | |
| Bedside nurse | Obtains access, labs, performs procedures. Together with airway provider completes secondary survey as needed. | |
| Standing 6 feet away in room in full PPE—eligible to be utilized at the bedside only if needed | Team lead | Physician leading the resuscitation if the airway provider is not functioning as team lead. |
| Medication nurse | Draws up medications, fluids and hands them over to bedside nurse. | |
| Technician | Ensures that the room stays shut. Calls out any equipment, supplies that need to be brought into the room. | |
| Documenting nurse | Documents resuscitation in medical record | |
| Outside of the resuscitation room | Resident or physician assistant | Computer order entry during resuscitation |
| Back up respiratory therapist | Runner for the hands-on respiratory therapist as needed | |
| Back up technician | Runner for equipment/supplies as needed | |
| Flow supervisor | Runner for medications as needed and ensures that room stays shut during resuscitation |
PED, pediatric emergency department; PPE, personal protective equipment.
We began with normal staffing, then subsequently removed 1 person at a time. We analyzed team comfort level and performance with each composition of team members. We monitored our teams’ ability to maintain room negative pressure, adherence to AHA COVID-19 guidelines, personnel safety, communication within and outside of the room, and success with the simulated resuscitation.
After achieving consistency in performance and participant feedback, we finalized room layout, equipment and supplies, and staffing models. In total, we conducted 7.5 hours of systems integration simulations over 2 weeks utilizing input from 30 different interprofessional participants.
Simulation to educate teams
We created an educational PowerPoint for the PED team that compared AHA COVID-19 and non-COVID-19 resuscitation recommendations and detailed who, what, why, where, when, and how of our new space. We distributed diagrams of staff placement and team member checklists. We oriented staff to the room, equipment, and supplies within the room, location of checklists, and new processes. We also reviewed challenges of team communication while fully donned in PPE and emphasized the need for continual precise loop closure both within and outside of the resuscitation room to foster situational awareness and a shared mental model. We then ran simulations focusing on the physical space, staffing and flow within that space, personnel safety, patient safety, the value of clear closed loop communication,10 and AHA COVID-19 resuscitation guidelines. These immersive simulations gave participants the opportunity for deliberate practice with facilitated feedback and reflection on performance. As a result, simulations or elements within the simulations were repeated as needed to ensure proper performance. In total, we conducted 14 hours of training simulations for 66 PED staff. The feedback is universal increased comfort with our new space, increased understanding of needed infection prevention and control measures surrounding COVID-19 resuscitations, improved understanding of AHA COVID-19 recommendations, and increased confidence in resuscitating a COVID-19 pediatric patient.
Conclusions
We utilized simulation as a vehicle to help us better understand COVID-19 resuscitation-related infection prevention and control issues within our PED. Simulation allowed us to understand barriers within our current space and helped us develop and refine a new process that would allow us to effectively resuscitate pediatric COVID-19 patients while minimizing personnel risks. And we used simulation to educate staff about our new space, processes, and workflows. Buy in from leadership stakeholders was key as they invested in our process, supported our journey and ensured that we were aligned with our organization's goals. Interprofessional input, willingness of staff to participate and learn new processes, timely and effective bidirectional feedback and loop closure of issues brought up during the simulations also led to our success. Further analysis is needed to ensure that these efforts translate to actual patient care within our PED.
We encourage the use of simulation to augment infection prevention and control initiatives. We hope that our journey may help inspire other teams to maximize the potential of simulation during the COVID-19 pandemic.
Acknowledgments
The authors would like to thank Jennifer Cooper, BSN, RN and Lisa M. Lietzke, MSN, RN, CPEN, TCRN for their assistance with this project.
Footnotes
Funding: This project received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of interest: The authors certify that to the best of our knowledge, no conflict of interest, financial or other, exists—MD and KD.
Author contributions: Drafting manuscript—MD and KD, Critical revision of manuscript for important intellectual content—MD and KD, Final approval of submitted version—MD and KD.
References
- 1.Edelson DP, Sasson C, Chan PS, et al. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: from the emergency cardiovascular care committee and get with the guidelines-resuscitation adult and pediatric task forces of the American Heart Association. Circulation. 2020;141:e933–e943. doi: 10.1161/CIRCULATIONAHA.120.047463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wheeler DS, Geis G, Mack EH, et al. High-reliability emergency response teams in the hospital: improving quality and safety using in situ simulation training. BMJ Qual Saf. 2013;22:507–514. doi: 10.1136/bmjqs-2012-000931. [DOI] [PubMed] [Google Scholar]
- 3.LeBlanc VR, Manser T, Weinger MB, et al. The study of factors affecting human and systems performance in healthcare using simulation. Simul Healthc. 2011;6(Suppl):S24–29. doi: 10.1097/SIH.0b013e318229f5c8. [DOI] [PubMed] [Google Scholar]
- 4.Choi GYS, Wan WTP, Chan AKM, et al. Preparedness for COVID-19: in situ simulation to enhance infection control systems in the intensive care unit. Br J Anaesth. 2020;125:e236–e239. doi: 10.1016/j.bja.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dieckmann P, Torgeirsen K, Qvindesland SA, et al. The use of simulation to prepare and improve responses to infectious disease outbreaks like COVID-19: practical tips and resources from Norway, Denmark, and the UK. Adv Simul (Lond) 2020;5:3. doi: 10.1186/s41077-020-00121-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reedy GB. Using cognitive load theory to inform simulation design and practice. Clin Simulation Nurs. 2015;11:355–360. [Google Scholar]
- 7.World Health Organization; Geneva: 2020. World Health Organization. Infection Prevention and Control During Health Care When Novel Coronavirus (nCoV) Infection Is Suspected: Interim Guidance, Updated.https://www.who.int/publications/i/item/10665-331495 WHO/2019-nCoV/IPC/2020.3. Available at: [Google Scholar]
- 8.Matava CT, Kovatsis PG, Lee JK, et al. Pediatric airway management in COVID-19 patients: consensus guidelines from the society for pediatric anesthesia's pediatric difficult intubation collaborative and the Canadian Pediatric Anesthesia Society. Anesth Analg. 2020;131:61–73. doi: 10.1213/ANE.0000000000004872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carvalho PVR, Righi AW, Huber GJ, et al. Reflections on work as done (WAD) and work as imagined (WAI) in an emergency response organization: a study on firefighters training exercises. Appl Ergon. 2018;68:28–41. doi: 10.1016/j.apergo.2017.10.016. [DOI] [PubMed] [Google Scholar]
- 10.Diaz M, Dawson K. Impact of simulation-based closed-loop communication training on medical errors in a pediatric emergency department [e-pub ahead of print] Am J Med Qual. 2020 doi: 10.1177/1062860620912480. Accessed August 15, 2020. [DOI] [PubMed] [Google Scholar]