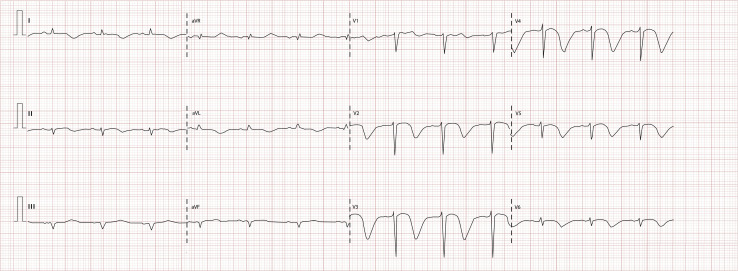
A 54-year-old woman with a history of type 2 diabetes and hypertension was admitted with dry cough and 3-day fever. She was dyspneic, with Sao 2 82%, pulse rate 75 beats/min, and blood pressure 100/60 mm Hg. Diffuse pulmonary rales were found. Laboratory results (normal range in parentheses) reported lymphopenia (total lymphocytes 900/μL), ferritin 717.5 ng/mL (23.9 to 336.2 ng/mL), albumin 3.3 g/dL (3.5 to 5 g/dL), D-dimer 1.6 μg/mL (0 to 0.24 μg/mL), and C-reactive protein 33.2 mg/L (1 to 3 mg/L). Chest radiograph showed bilateral diffuse interstitial infiltrates. The initial management included oxygen with a nonrebreathing mask with flow at 10 L/min and thromboprophylaxis with enoxaparin. Results for real-time reverse transcriptase–polymerase chain reaction for detection of severe acute respiratory syndrome coronavirus 2 ribonucleic acid were positive, so antiviral therapy (lopinavir 400 mg/ritonavir 100 mg twice a day) was added. On the fourth day of evolution, the patient developed acute chest pain, hypotension, and pulmonary edema. The new laboratory results reported high-sensitivity cardiac troponin at 692 ng/L (8 to 18 ng/L), creatine kinase-MB 11.78 ng/dL (0.06 to 6.3 ng/dL), and N-terminal pro hormone BNP 9,000 pg/mL (15 to 125 pg/mL). A 12-lead ECG was performed (Figure 1 ).
Figure 1.
ECG after hemodynamic deterioration.
What is the most likely diagnosis?
Diagnosis
Interpretation
Takotsubo’s syndrome associated with COVID-19 infection. In Figure 1, the ECG shows pulse rate 75 beats/min; PR interval 160 msec; QRS interval 100 msec; prolonged QTc interval 551 msec; QRS axis –30 degrees; poor R-wave progression; giant inverted T waves at V2 to V6, DI, and AVL; and Q waves at DII and AVF.
Clinical Course
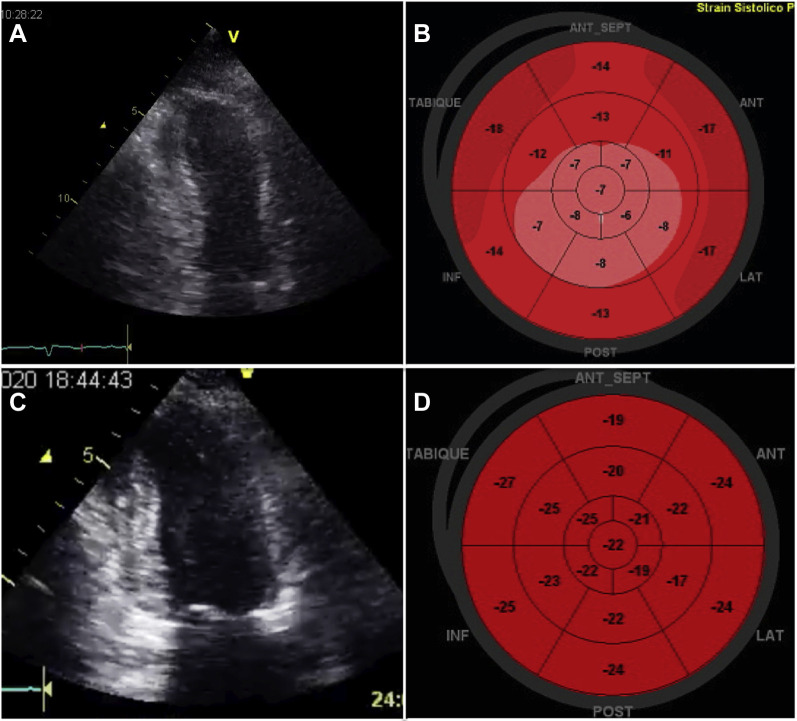
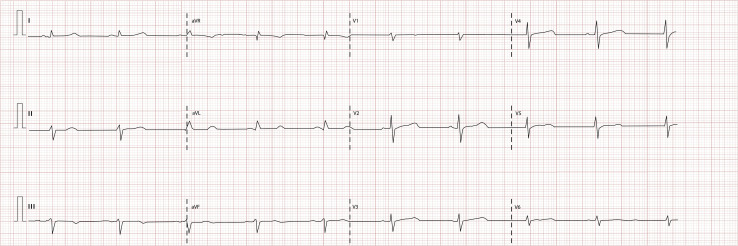
Transthoracic echocardiography was performed. In the apical 2-chamber view, apical ballooning with normal contraction of the basal segments was observed (Figure 2 A); left ventricular longitudinal strain was decreased in the mid and apical segments (Figure 2 B). Advanced airway management and invasive mechanical ventilation were started, with high requirements for vasopressors and inotropes. After medical management was established with hemodynamic and respiratory support, transthoracic echocardiography was performed again, showing reversal of regional wall-motion abnormalities in the apical 2-chamber view (Figure 2 C) and in the left ventricular longitudinal strain (Figure 2 D). Normalization in the T waves, significant reduction of QTc interval (469 msec), and disappearance of the Q waves was also noticed 1 week after the initial ECG (Figure 3 ).
Figure 2.
A, Apical 2-chamber view showing apical ballooning. B, Bull's-eye plot of the left ventricle's global longitudinal strain of –11.8% (reduced), showing that the apical segments (center) are the predominantly affected area. C, Apical 2-chamber view showing improvement of regional wall-motion abnormalities. D, Bull's-eye plot of the left ventricle's global longitudinal strain of –22% (normal), showing improvement at the apical and mid segments.
Figure 3.
ECG after hemodynamic and respiratory stabilization.
Discussion
The differential diagnosis of giant inverted T waves should include Takotsubo’s syndrome, myocarditis, acute pericarditis, acute myocardial infarction, hypokalemia, pulmonary embolism, hypertrophic cardiomyopathy, and intracranial bleeding.1 One study that compared patients with confirmed acute myocardial infarction with those with confirmed Takotsubo’s syndrome found that inverted T waves without concomitant ST-segment elevation or ST-segment depression occurred more frequently in Takotsubo’s syndrome than acute myocardial infarction.2 This clinical entity is classified in the stress-related cardiomyopathy syndromes, and postmenopausal women are predominantly affected (approximately 80% are older than 50 years). Sympathetic stimulation is the central pathogenesis and has been associated with conditions of catecholamine excess. In the critically ill patient with sudden hemodynamic deterioration, investigation should always be made for a stress-related cardiomyopathy syndrome.
The classic Takotsubo’s syndrome pattern is characterized by transient left ventricular systolic dysfunction with apical akinesia or dyskinesia (apical ballooning) and compensatory basal hyperkinesia (or normal contraction). One of the main features of this pathologic process includes its reversibility after the insult is eliminated. ECG normalization is variable, with gradual resolution of T-wave inversion and QTc-interval prolongation during days to weeks, and complete recovery of regional wall-motion abnormalities in 4 to 8 weeks.3 In coronavirus disease 2019 infection, the main physiopathologic mechanisms include systemic inflammatory response syndrome and thrombosis. Currently published data suggest that a sizeable proportion of individuals with this infection develop cardiovascular complications (7.2% acute cardiac injury, 16.7% arrhythmias, and 23% heart failure). To date, few cases of Takotsubo’s syndrome with coronavirus disease 2019 infection have been formally reported.4 In this patient with confirmed coronavirus disease 2019 infection and because of her comorbidities and clinical presentation, the initial differential diagnosis included Takotsubo’s syndrome, pulmonary embolism, and myocardial infarction. This patient had an InterTAK Diagnostic Score of 56 points, including the following criteria: female sex (25 points), physical trigger (13 points), absence of ST-segment depression (12 points), and QTc-interval prolongation (6 points); patients with a score of greater than or equal to 50 receive a diagnosis of Takotsubo’s syndrome in nearly 95% of cases.5 The patient had an adequate evolution; tracheostomy was performed after 14 days of invasive mechanical ventilation and she was weaned from the ventilator.
In prioritizing intrahospital security policies during the pandemic to limit staff exposure and because of the initial transthoracic echocardiographic abnormalities and their reversal after medical management (along with T-wave normalization), we considered Takotsubo’s syndrome as the final diagnosis without the need for coronary anatomy imaging.3
Pearls
-
•
In a critically ill patient with new giant inverted T waves on ECG and sudden hemodynamic instability, Takotsubo’s syndrome needs to be considered.
-
•
A differential diagnosis of giant inverted T waves should also include pulmonary embolism and acute myocardial infarction.
-
•
Improvement of the ECG and echocardiographic abnormalities over time is typical in patients with Takotsubo’s syndrome.
Acknowledgments
The authors acknowledge the INC Critical Care Ultrasonography Working Group.
Footnotes
For the diagnosis and teaching points, see page 266.
To view the entire collection of ECG of the Month, visitwww.annemergmed.com.
References
- 1.Pillarisetti J., Gupta K. Giant inverted T waves in the emergency department: case report and review of differential diagnoses. J Electrocardiol. 2010;43:40–42. doi: 10.1016/j.jelectrocard.2009.08.048. [DOI] [PubMed] [Google Scholar]
- 2.Frangieh A., Obeid S., Ghadri J., et al. ECG criteria to differentiate between Takotsubo (stress) cardiomyopathy and myocardial infarction. J Am Heart Assoc. 2016;5:e003418. doi: 10.1161/JAHA.116.003418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ghadri J., Wittstein I., Prasad A., et al. International expert consensus document on Takotsubo syndrome (part II): diagnostic workup, outcome and management. Eur Heart J. 2018;39:2047–2062. doi: 10.1093/eurheartj/ehy077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Minhas A., Scheel P., Garibaldi B., et al Takotsubo syndrome in the setting of COVID-19. JACC Case Rep. 2020;2:1321–1325. doi: 10.1016/j.jaccas.2020.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ghadri J., Cammann V., Jurisic S., et al. A novel clinical score (InterTAK Diagnostic Score) to differentiate Takotsubo syndrome from acute coronary syndrome: results from the International Takotsubo Registry. Eur J Heart Fail. 2016;19:1036–1042. doi: 10.1002/ejhf.683. [DOI] [PubMed] [Google Scholar]