As of early July 2020, >10 000 000 confirmed severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2; coronavirus disease 2019 [COVID‐19]) cases and 500 000 deaths have been recorded worldwide. This dramatic surge of the pandemic resulted in hospital overcrowding and shortages in intensive care unit (ICU) beds, creating a global crisis in healthcare systems [1]. As for many other specialties, Urology was impacted at different levels [2, 3]. A decline in number of elective surgeries was observed, with peaks of >94% reduction in most affected regions [4]. Outpatient clinics were largely shifted to virtual consults [5]. Interestingly, there was a significant decrease in hospital attendance for urological emergencies [6]. Urological surgical training was negatively impacted [7].
In the uro‐oncology field, timely patient selection based on priority criteria for surgical treatment was advocated [8]. We enjoyed reading the report from the Martini Clinic, a renowned high‐volume centre for prostate cancer surgery, where favourable outcomes were obtained without implementing rigorous screening measures, and by only applying strict protective hygiene standards [9]. Albeit remarkable, their experience might not be applicable to countries with different demographics, health systems, hospital resources, and testing capabilities. In this regard, some key differences between Germany and Italy are notable. As of 20 April 2020, >180 000 cases and 24 114 deaths had been recorded in Italy, most of which were in Northern Italy, with Lombardy being the leading region (>66 000 cases and 12 376 deaths at that time point). Southern Italy was in general less affected, with the Campania region recording >4000 cases and only 309 deaths. Germany had high testing rates early in the pandemic, which may have contributed to lower death rates. Moreover, Germany was very meticulous in tracking the contacts of those testing positive. This was not the case in Northern Italy, especially in the early phase. Another key factor was the number of hospital beds in Germany, a total of 497 000 for general and acute care (by contrast, the UK has 101 255). A recent Organisation for Economic Co‐operation and Development (OECD) survey found that before the crisis Germany had 33.9 ICU beds per 100 000 people, compared with 9.7 in Spain and 8.6 in Italy.
We would like to describe how our experience matured at a high‐volume cancer centre in Southern Italy during the early phase of the COVID‐19 pandemic, and to illustrate how a planned re‐organisation of the hospital and regional healthcare system allowed avoiding major disruption to the most commonly performed uro‐oncological surgical procedures. We looked at the surgical procedures for urological cancers performed at the Fondazione ‘G. Pascale’ IRCCS (Naples, Italy) from 2 March to 20 April 2020. A workflow was established to optimise outcomes and minimise risk of transmission. Each case was evaluated by a multidisciplinary team consisting of a urological surgeon, a genitourinary medical oncologist, and an anaesthesiologist. Intervention priorities were determined based on disease severity, risk of progression, length of time on the waiting list, disease‐related symptoms, and anaesthetic risk. At the time of pre‐hospitalisation, all patients were assessed by means of nursing triage, so that body temperature was measured, presence of COVID‐19 symptoms was ruled out, as well as possible contact with positive patients. Starting 1 April 2020, rapid blood testing was available to verify presence of (IgG)‐IgM. Asymptomatic COVID‐19‐postive patients were quarantined at home.
Use of appropriate personal protective equipment (PPE) was strictly adopted. All patients had surgical masks, and all healthcare workers were provided with filtering facepiece (FFP)‐2 masks (‘N95’ in the USA). Anaesthesia team members also wore face shields, and intubations were performed with glidescope assistance, using protective plastic intubation. Moreover, steps were taken to minimise CO2 release during robotic procedures, including use of filtered insufflation systems and low‐pressure pneumoperitoneum.
Overall, 93 patients underwent a urological surgical procedure, of which and 38 (40.8%) were performed robotically. The mean patient age was 65 years and the mean American Society of Anesthesiologists score was 2. The most common procedure was transurethral resection of the bladder with 22 cases (23%), whereas radical prostatectomy was the most common robotic procedure (18% of total). A similar number of procedures, 96 overall of which 31 robotic (30%), had been performed in the same period in 2019. Overall, there were no differences in terms of surgical outcomes between the two time periods. Only one radical cystectomy patient developed fever, reduced oxygen saturation, and lymphocytopenia on postoperative day 3. A chest X‐ray and oropharyngeal swab confirmed COVID‐19. He was transferred to a COVID‐19 hospital within the regional healthcare system where he was discharged home after 3 weeks following two consecutive negative test results. The patient did not suffer respiratory sequelae.
Healthcare in Italy is organised on a regional basis. In our region (Regione Campania), with a population of ~5.8 million people, the regional health system was restructured to create ‘COVID‐19 hospitals’ for acute management of patients with COVID‐19. Selected hospitals were provided with ‘purpose‐built’ wards specifically reserved for patients with COVID‐19, but they could still offer, to a limited capacity, elective (mostly emergent) cases. Ours was the only ‘COVID‐19‐free’ regional cancer centre. This allowed an optimal triage of incoming patients, with the possibility of transferring those testing positive to ‘COVID‐19 hospitals’, thus avoiding disruption of the timely management of non‐COVID‐19 cancer cases (Fig. 1). In general, we preferred robotic over open surgery to minimise surgical morbidity and minimise hospital stay. To date no transmission of the virus has been reported during laparoscopic procedures, and this remains open for debate, as recently pointed out by the Society of Robotic Surgery [10].
Fig. 1.
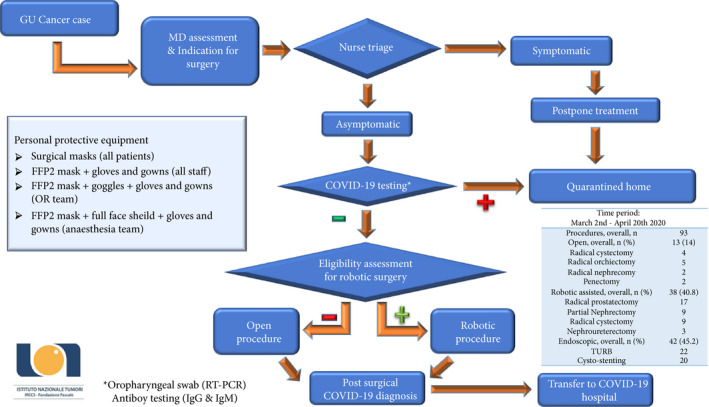
Implemented workflow to optimise surgical management of patients with genitourinary cancer at a COVID‐19‐free hospital (Istituto Nazionale Tumori IRCCS ‘Fondazione G. Pascale’, Naples, Italy). GU, genitourinary; MD, multidisciplinary; OR, operating room.
There are both similarities and differences between our experience and that reported by Würnschimmel et al. [9]. As discussed, there was a different impact of the pandemic in Germany vs Italy. While the Martini Clinic is a University‐affiliated private clinic dedicated to prostate cancer treatment, our hospital is a public ‘free standing’ cancer centre, where all genitourinary malignancies are treated. Our German colleagues did not perform COVID‐19 screening initially on a routine basis, but rather relied on patient history prior to admission, whereas we adopted in‐hospital screening for asymptomatic patients early on. In this regard, we implemented initially oropharyngeal swab (reverse transcriptase‐PCR) testing, and soon after antibody (IgG/IgM) blood test, whereas we did not use CT chest as a screening tool [11].
Overall, our experience shows that appropriate health network and hospital re‐organisation, multidisciplinary collaboration, careful patient selection, and adoption of safety protocols, allows for the safe preservation of the flow of uro‐oncological surgical procedures during this COVID‐19 era. This translates into a timely and effective treatment of patients with genitourinary cancer.
Conflicts of Interest
None.
Abbreviations
- COVID‐19
coronavirus disease 2019
- FFP
filtering facepiece
- ICU
intensive care unit
- Ig(G)(M)
immunoglobulin (G)(M)
- PPE
personal protective equipment
- SARS‐CoV‐2
severe acute respiratory syndrome coronavirus‐2
References
- 1. Boccia S, Ricciardi W, Ioannidis JP. What other countries can learn from Italy during the COVID‐19 pandemic. JAMA Intern Med 2020; 180: 927–8 [DOI] [PubMed] [Google Scholar]
- 2. Puliatti S, Eissa A, Eissa R et al. COVID‐19 and urology: a comprehensive review of the literature. BJU Int 2020; 125: E7–14 [DOI] [PubMed] [Google Scholar]
- 3. Ficarra V, Novara G, Abrate A et al. Urology practice during COVID‐19 pandemic. Minerva Urol Nefrol 2020; 72: 369–75 [DOI] [PubMed] [Google Scholar]
- 4. Rocco B, Sighinolfi MC, Sandri M et al. The dramatic COVID‐19 outbreak in Italy is responsible of a huge drop in urological surgical activity: a multicentre observational study. BJU Int 2020. [Online ahead of print]. 10.1111/bju.15149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Patel S, Douglas‐Moore J. A reflection on an adapted approach from face‐to‐face to telephone consultations in our Urology outpatient department during the COVID‐19 pandemic – a pathway for change to future practice? BJU Int 2020. [Epub ahead of print]. 10.1111/bju.15119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Novara G, Bartoletti R, Crestani A et al. Impact of COVID‐19 pandemic on the urologic practice in the emergency departments in Italy. BJU Int 2020. [Epub ahead of print]. 10.1111/bju.15107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Porpiglia F, Checcucci E, Amparore D et al. Slowdown of urology residents’ learning curve during the COVID‐19 emergency. BJU Int 2020; 125: E15–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Campi R, Amparore D, Capitanio U et al. Assessing the burden of nondeferrable major uro‐oncologic surgery to guide prioritisation strategies during the COVID‐19 pandemic: insights from three Italian high‐volume referral centres. Eur Urol 2020; 78: 11–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Würnschimmel C, Maurer T, Knipper S, et al. Martini‐Klinik experience on prostate cancer surgery during the early phase of COVID‐19. BJU Int 2020. [Epub ahead of print]. 10.1111/bju.15115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Porter J, Blau E, Gharagozloo F et al. Society of robotic surgery review: recommendations regarding the risk of COVID‐19 transmission during minimally invasive surgery. BJU Int 2020. [Epub ahead of print]. 10.1111/bju.15105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ai T, Yang Z, Hou H, et al. Correlation of chest CT and RT‐PCR testing in coronavirus disease 2019 (COVID‐19) in China: a report of 1014 cases. Radiology 2020. [Epub ahead of print. 10.1148/radiol.2020200642 [DOI] [PMC free article] [PubMed] [Google Scholar]


