Abstract
Aim
In Hokkaido, Japan, the number of people suffering from coronavirus disease 2019 (COVID‐19) is rapidly increased, and by the end of February 2020, there were already 70 confirmed cases of the disease. We investigated the safety of urgently initiated maternal telemedicine in preventing the spread of the coronavirus infection.
Methods
This retrospective, single‐institution study examined maternal telemedicine at the department of obstetrics of the Hokkaido University Hospital from March 4 to April 2, 2020. The physicians remotely examined the pregnant women from their homes using a visual communication system which kept communication confidential, performed prenatal checkup and administered medical care according to their various blood pressures, weights and cardiotocograms.
Results
Forty‐four pregnant women received a total of 67 telemedicine interventions. Thirty‐two pregnant women (73%) had complications, and 22 were primiparas (50%). Telemedicine interventions were provided 19 times at less than 26 weeks of gestation, 43 times between 26 and 36 weeks of gestation and 5 times after 37 weeks of gestation. There was one case with an abnormality diagnosed during the remote prenatal checkups, and the patient was hospitalized on the same day. However, there were no abnormal findings observed in mothers and children during the other 66 remote prenatal checkups and medical care.
Conclusion
Maternal telemedicine can be safely conducted in pregnant women who are at risk of having an underlying disorder or fetal abnormality 1 month following the start of the attempt. It should be considered as a form of maternal medical care to prevent the spread of COVID‐19.
Keywords: cardiotocograph, COVID‐19, pregnancy, telemedicine
Introduction
The coronavirus disease 2019 (COVID‐19) is caused by a new strain of the coronavirus that has been detected in patients with idiopathic pneumonia in Wuhan, China, since December 2019. The first case of the disease in Japan was confirmed on January 16, 2020. In Hokkaido, Japan, the first case of the infection was confirmed among Chinese women on January 28, 2020, and the number of infected persons increased to 70 by February 29, 2020. This was the first outbreak in Japan. A state of emergency was declared in Hokkaido by its governor on February 28, 2020, and each person started their own efforts to prevent the spread of the infection.
The average incubation period of COVID‐19 is 5.2 days (95% confidence interval: 4.1–7.0), and the 95th percentile is 12.5 days. 1 A single infected person spreads the infection to an average of 2.2 other persons (95% confidence interval: 1.4–3.9), and the number of infected persons doubles every 7.4 days at the early stage of the epidemic. 1 Initial symptoms reported are fever, cough, fatigue, etc. 2 Dyspnea occurs within 5.0 days of the onset, admission within 7.0 days, and acute respiratory distress syndrome within 8.0 days. 3 The risk of hospital‐related transmission is also high, with hospital‐related transmission reported to account for 41% of cases. 3
The Hokkaido University Hospital is a core hospital in the region where pregnant women using immunosuppressants for autoimmune diseases and pregnant women susceptible to diseases such as diabetes mellitus, go for antenatal visits. Therefore, considering the rapid spread of COVID‐19 and the high risk of hospital‐related transmission, the improvement of remote medical care for pregnant women was deemed urgent to reduce the risk of coronavirus infection during antenatal visits.
Telemedicine for pregnant women at home on a large scale is the first trial of its kind in Japan. Considering the current situation, where COVID‐19 infection is spreading, this form of prenatal checkup may be effective. Therefore, we report the safety and usefulness of this form of checkup, although it was conducted over a short period of time, within just 1 month of its initiation.
Methods
Attempts of remote prenatal checkups and examinations began on March 4, 2020. Maternal telemedicine was approved by the Hokkaido University Hospital Ethics Committee (No. 79), by the government of Hokkaido, and by the Ministry of Health, Labor and Welfare. The data of the pregnant women provided with telemedicine interventions from March 4 to April 2, 2020 were used for the analysis. Pregnant women with twin pregnancies, fetal growth restrictions and conditions deemed inappropriate by the physician were excluded from the study, and other pregnant women benefited from the information on remote maternal care. This retrospective study was approved by the institutional review board of the Hokkaido University Hospital.
Method of remote prenatal checkups and medical care
We carried out maternal telemedicine through the following procedures:
Pregnant women who came to the outpatient clinic gave written informed consent for telemedicine, and pregnant women who were taking immunosuppressants or having symptoms of infections gave verbal informed consent for telemedicine through a visual communication system from their homes.
The pregnant women referred to the Hokkaido University Hospital Obstetrics website (https://www.hokudaibyouin-sanka.com) and registered their names, addresses and other relevant information.
The Hokkaido University Center of Innovation, supported by the Japan Science and Technology Agency, mailed a cardiotocograph and a sphygmomanometer to each pregnant woman's home address. The cardiotocograph used was iCTG (Melody International Ltd.).
The pregnant women were to have their blood pressure and weight measured on the morning of the day of the appointment and record the cardiotocogram for 20 min.
The doctor calls the pregnant woman during her appointment time and connects her smartphone or laptop to a computer at Hokkaido University Hospital via a visual communication system. The visual communication system uses Kizuna Web (Borderless Vision Corp.) with a Transport Layer Security.
The doctors used a visual communication system to examine pregnant women and take note of their blood pressures, body weights, and cardiotocogram findings in a medical record.
If any medication was needed, the doctor prescribed the drug at the hospital which was mailed to the woman's home by the Department of Center of Innovation.
The pregnant women then requested the delivery company to collect the cardiotocograph and the sphygmomanometer immediately after the examination to return them, a service they paid for out of pocket.
The pregnant women would pay the same fee charged for regular prenatal checkups when they come back later.
Pregnant women at less than 26 gestational weeks were not sent cardiotocograms and were only examined in terms of blood pressure and body weight through a visual communication system. They were required to visit the hospital at 12, 20, 24, 30 and 36 weeks of gestation for ultrasonography and other examinations. Telemedicine services were also provided for other reasons at their request.
Results
From March 4 to April 2, 2020, a total of 122 patients were examined. Of these, 9 had twins, 3 had fetal growth restriction, 3 had signs of preterm labor, 3 had disorders at risk of fetal anemia, 2 had psychiatric disorders, 2 had fetal abnormalities requiring frequent ultrasonography, 2 had social problems and 1 had a disorder of the placenta. Of the other 97 patients, 87 agreed to be served through telemedicine. Forty‐four pregnant women underwent a total of 67 telemedicine sessions during the study period. Their mean age was 33.5 ± 5 years (range, 22–43), and there were 22 primiparas (50%) and 12 healthy pregnant women (27%) (Table 1). The period from the initial visit to the first telemedicine session was 105 ± 52 days (range, 17–206). One case was diagnosed with an abnormality during remote prenatal checkups, and the patient was hospitalized on the same day. However, no abnormal findings were observed in the mothers and children of the other 66 pregnant women who underwent remote prenatal checkups and medical care.
Table 1.
Demographic characteristics of the study population
| No. of women | 44 |
| Nulliparous women | 22 (50%) |
| Age (year) | 33.5 ± 5 (range, 22–43) |
| The underlying diseases of pregnant women | |
| Autoimmune diseases† | 9 (20%) |
| Hematological diseases | 4 (9%) |
| Diabetes ‡ | 4 (9%) |
| Psychiatric diseases | 3 (7%) |
| Cervical incompetence | 3 (7%) |
| Cardiovascular diseases | 3 (7%) |
| Infectious diseases | 2 (5%) |
| Fetal abnormalities | 1 (2%) |
| Thyroid diseases | 1 (2%) |
| Hypertension | 1 (2%) |
| Placental location abnormality | 1 (2%) |
| Healthy pregnant | 12 (27%) |
| The timing of telemedicine performed | |
| ≤25 weeks | 19 (28%) |
| 26–36 weeks | 43 (64%) |
| 37 weeks ≤ | 5 (7%) |
Five patients used immunosuppressant.
Including gestational diabetes.
The hospitalized case
A 35‐year‐old primiparous woman was referred to our hospital for relocation at 17 weeks of gestation. Cervical cerclage was performed for cervical incompetence at 19 weeks of gestation, and the patient was discharged at 22 weeks of gestation. The first remote telemedicine session was performed at 31 weeks and 6 days of gestation when the cardiotocogram showed no uterine contractions (Fig. 1). At the second remote prenatal visit at 33 weeks and 1 day of gestation, despite unnoticeable uterine contractions, she complained of lower abdominal tightness, and that the fetal head was lowered; uterine contractions were observed every 5 minutes on the cardiotocogram (Fig. 1). Immediately, the patient was instructed to visit the hospital. The cervical canal length was 22 mm, and the opening of the internal cervical canal to the suture thread was confirmed. The patient was hospitalized on the same day.
Figure 1.
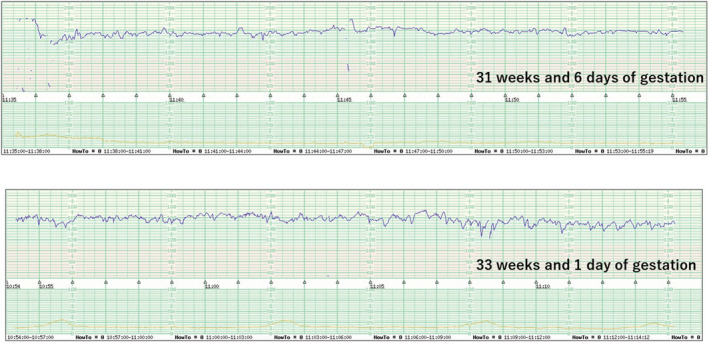
Cardiotocogram‐determined hospitalization through remote diagnosis. Uterine contraction was not recognized by the cardiotocogram at 31 weeks and 6 days of gestation (upper panel) but was observed every 5 min at 33 weeks and 1 day of gestation (lower panel).
Discussion
This trial showed that even pregnant women with complications can safely undergo remote prenatal checkups and medical care. In addition, for impending preterm birth, the necessity of hospitalization could be detected from home, and a certain screening ability was indicated.
Pregnancy‐related electronic health technology has shown comparable utility to standard healthcare in managing gestational diabetes mellitus, 4 medical abortion, 5 and assisted reproductive technology. 6 A review of pregnancy eHealth had reported few remote practices for high‐risk pregnant women, 7 but a randomized controlled trial has now been initiated in the Netherlands to investigate the safety and usefulness of remote practices for high‐risk pregnant women with pre‐eclampsia, fetal growth restriction, preterm rupture of membranes, recurrent reduced fetal movements or an intrauterine fetal death in a previous pregnancy. 8 These reports are of the doctor to patient (D to P) type, but remote medical care for pregnant women, which has been conducted only in some areas of Japan, is of the doctor to patient with nurse (D to P with N) type. 9 One of the reasons for this is that D to P telemedicine has not been approved for pregnant women in the Japanese medical system.
Coronavirus infection is known to be asymptomatic but contagious, 10 , 11 and hospital‐acquired infections have been reported in as much as 41% of cases, 3 with an increased risk of hospital‐related transmission. In New York, 14 (33%) of 43 pregnancies were found to be asymptomatic COVID‐19 patients by testing during admission, 12 and 13.5% were asymptomatic‐positive during a universal screening of 215 pregnant women. 13 We should beware of the risk of pregnant women getting infected during outpatient visits.
The specific needs of pregnant women should be included in the response plan as the COVID‐19 outbreak can have a significant impact on healthcare infrastructure. This time, the medical examination using the visual communication system was also approved by the Ministry of Health, Labor and Welfare as a valid medical practice. Although it is still a month after initiation, it is safe for pregnant women with various underlying diseases and has the screening capacity to determine which cases would require hospitalization. Remote prenatal care should be considered as a valid option in the perinatal care system during the COVID‐19 transmission period to reduce the incidence of infection among pregnant women with a low resistance to infection.
Disclosure
None declared.
Acknowledgments
This telemedicine trial was carried out with human and financial support from the Department of Center of Innovation, Hokkaido University (JST COI Grant Number JPMJCE1301), and administrative support from the Bureau of Regional Medical Service Promotion, Department of Health and Welfare of the Hokkaido Government. Melody International Ltd. (Takamatsu, Japan) and Atom Medical Corp. (Tokyo, Japan) lent us the cardiotocograph. Borderless Vision Corp. (Sapporo, Japan) urgently developed a visual communication system that met the standards required for this trial.
References
- 1. Li Q, Guan X, Wu P et al. Early transmission dynamics in Wuhan, China, of novel coronavirus‐infected pneumonia. N Engl J Med 2020; 382: 1199–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chen N, Zhou M, Dong X et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020; 395: 507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wang D, Hu B, Hu C et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus‐infected pneumonia in Wuhan, China. JAMA 2020; 323: 1061–1069. 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ming WK, Mackillop LH, Farmer AJ et al. Telemedicine technologies for diabetes in pregnancy: A systematic review and meta‐analysis. J Med Internet Res 2016; 18: e290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Endler M, Lavelanet A, Cleeve A, Ganatra B, Gomperts R, Gemzell‐Danielsson K. Telemedicine for medical abortion: A systematic review. BJOG 2019; 126: 1094–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hernández C, Valdera CJ, Cordero J, López E, Plaza J, Albi M. Impact of telemedicine on assisted reproduction treatment in the public health system. J Healthc Qual Res 2020; 35: 27–34. [DOI] [PubMed] [Google Scholar]
- 7. van den Heuvel JF, Groenhof TK, Veerbeek JH et al. eHealth as the next‐generation perinatal care: An overview of the literature. J Med Internet Res 2018; 20: e202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. van den Heuvel JFM, Ganzevoort W, De Haan‐Jebbink JM et al. Hospital care versus Telemonitoring in high‐risk pregnancy (HOTEL): Study protocol for a multicentre non‐inferiority randomised controlled trial. BMJ Open 2019; 9: e031700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Onishi Norimitsu. In Japan's rural areas, remote obstetrics fills the gap. The New York Times. [Cited 8 April 2007]. Available from URL: https://www.nytimes.com/2007/04/08/world/asia/08japan.html
- 10. Rothe C, Schunk M, Sothmann P et al. Transmission of 2019‐nCoV infection from an asymptomatic contact in Germany. N Engl J Med 2020; 382: 970–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zou L, Ruan F, Huang M et al. SARS‐CoV‐2 viral load in upper respiratory specimens of infected patients. N Engl J Med 2020; 382: 1177–1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Breslin N, Baptiste C, Gyamfi‐Bannerman C et al. COVID‐19 infection among asymptomatic and symptomatic pregnant women: Two weeks of confirmed presentations to an affiliated pair of new York City hospitals. Am J Obstet Gynecol MFM 2020; 2(2): 100118. https://www.sciencedirect.com/science/article/pii/S2589933320300483?via%3Dihub [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sutton D, Fuchs K, D'Alton M, Goffman D. Universal screening for SARS‐CoV‐2 in women admitted for delivery. N Engl J Med 2020; 382: 2163–2164. 10.1056/NEJMc2009316. [DOI] [PMC free article] [PubMed] [Google Scholar]


