Abstract
BACKGROUND AND PURPOSE:
Evaluation of shunted hydrocephalus is the most common indication for ultrafast brain MRI. Radiation-/sedation-free imaging capabilities make this protocol more desirable over CT and standard brain MRI. We hypothesized that ultrafast brain MRI can be used for selected indications beyond shunted hydrocephalus without adverse outcomes.
MATERIALS AND METHODS:
Ultrafast brain MRI was performed with axial, sagittal, and coronal HASTE. The radiology information system was used to identify pediatric patients (0–18 years of age) who underwent ultrafast brain MRI between March 2014 and May 2016. A retrospective chart review was completed to identify indications other than shunted hydrocephalus, such as ventriculomegaly, macrocephaly, or intracranial cyst. All ultrafast brain MRIs were evaluated by a certified neuroradiologist and a neurosurgeon. Ultrafast brain MRI was deemed of sufficient diagnostic value for these indications if no further standard brain MRI was required for the study indication or if additional imaging was performed for an alternate indication.
RESULTS:
The radiology information system identified 800 patients who had undergone an ultrafast brain MRI during the study period. One hundred twenty-two of these patients had ventriculomegaly, macrocephaly, or intracranial cyst as the study indication. Twenty-one of the 122 patients were excluded due to insufficient follow-up. Of the remaining 101 patients, only 5 had a standard brain MRI for the same indication, with no additional clinically significant information identified on those studies.
CONCLUSIONS:
These results suggest that ultrafast brain MRI is sufficient to evaluate ventriculomegaly, macrocephaly, or intracranial cyst. Ultrafast brain MRI is radiation- and sedation-free; therefore, we recommend its use as the primary screening neuroimaging study for these indications.
Ultrafast brain MRI (UFB-MRI) has been used for evaluation of shunted hydrocephalus since 2002 per published data in PubMed.1 Lack of ionizing radiation made UFB-MRI a preferred technique for evaluation of pediatric shunted hydrocephalus, given the longer survival rates and concerns for cumulative radiation doses in these children.2–4 In addition, UFB-MRI does not require sedation or general anesthesia due to the short imaging time. Adverse outcomes of general anesthesia in young children5 make standard brain MRI protocols less desirable. In addition, the short total acquisition time of UFB-MRI improves patient throughput/work flow and consequently may improve overall health care costs.6,7 Initially, the published literature focused on the use of UFB-MRI in patients with shunted hydrocephalus.1,3,8,9 Later, modified fast protocols were proposed, such as for brain trauma.10,11 Although the use of UFB-MRI for indications other than hydrocephalus has been proposed in prior publications,12,13 validation for those indications has not been published.
UFB-MRI demonstrates fluid-containing structures well against the brain parenchyma and calvaria. We hypothesized that UFB-MRI can be used beyond shunted hydrocephalus for indications such ventriculomegaly (Figs 1–3), macrocephaly (Fig 4), or intracranial cyst (Fig 5) without adverse outcomes.
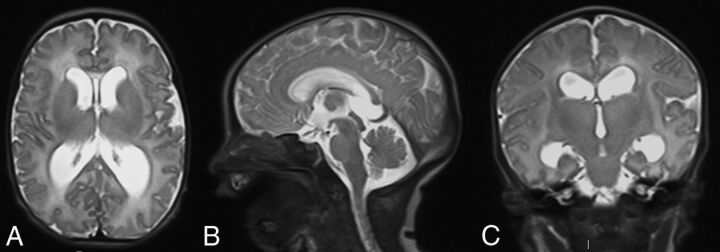
Fig 1.
UFB-MRI performed in axial (A), sagittal (B), and coronal (C) planes with HASTE in a 1-day-old male infant with natural sleep. The study indication was a prenatal diagnosis of ventriculomegaly. Note the mild enlargement of the supratentorial ventricles and normal size of the fourth ventricle. There were no clinical signs of increased intracranial pressure. Although the cerebral aqueduct patency evaluation was limited in this study, the patient was followed with UFB-MRI. No additional standard MRI was deemed clinically necessary (Fig 2).
Fig 2.
Coronal HASTE of the same patient as in Fig 1 obtained at day of life 1 (A), 5 months of age (B), and 2 years of age (C). Imaging demonstrates normalization of the ventricular size across time. High-quality diagnostic images were obtained without exposure to radiation or sedation/anesthesia. Ventricular size and extra-axial spaces are easily seen in all UFB-MRIs. This case shows the value of UFB-MRI in follow-up examinations in children with ventriculomegaly.
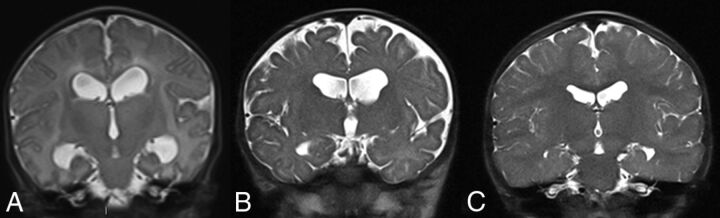
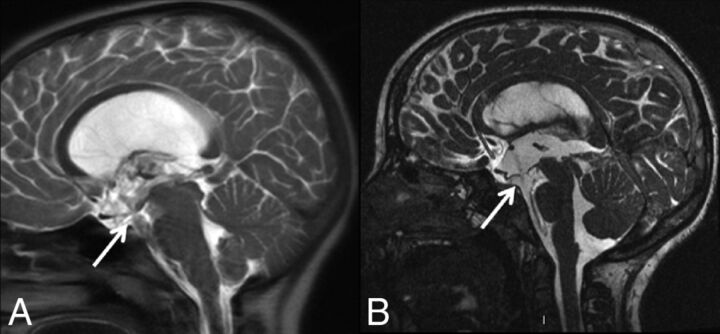
Fig 3.
A 10-year-old girl incidentally found to have hydrocephalus. In this imaging, she is 6 months status post third ventriculostomy. A, Sagittal HASTE in the midline shows lateral ventriculomegaly. Note the CSF flow artifacts/signal loss through the ventriculostomy site (arrow) at the floor of the third ventricle, B, Sagittal CISS at the same plane shows similar findings (arrow) with higher spatial resolution.
Fig 4.
A 3-month-old child with macrocephaly and head circumference increase from the 50th to >95th percentile with normal neurologic developmental milestones. UFB-MRI was performed with axial (A), coronal (B), and sagittal (C) HASTE. Note mild supratentorial ventriculomegaly and prominence of the frontoparietal extra-axial CSF spaces confirming benign enlargement of the extra-axial CSF spaces.
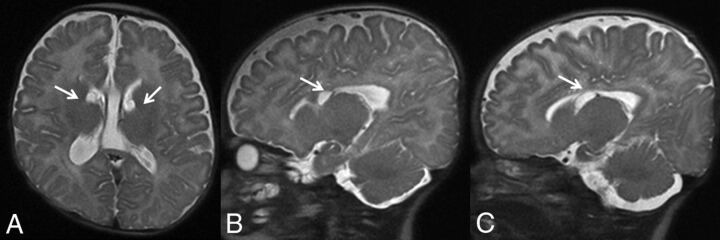
Fig 5.
A 2-month-old boy with a prenatal diagnosis of intracranial cysts. Axial (A), right (B), and left (C) parasagittal HASTE shows simple-appearing cysts at the caudothalamic notches (arrows) without other abnormalities. Note the normal ventricular size. Follow-up MRI at 6 months of age showed resolution of these cysts.
Materials and Methods
The radiology information system was used to identify pediatric patients (0–18 years of age) who underwent UFB-MRI between March 2014 and May 2016. A retrospective chart review was completed in these cases to identify the following indications: ventriculomegaly, macrocephaly, or intracranial cyst. UFB-MRI was performed with axial, sagittal, and coronal HASTE (TR, 3000 ms; TE, 90–120 ms; slice thickness, 4 mm) using the head coils on 1.5T and 3T scanners (Siemens, Erlangen, Germany).
All UFB-MRIs were evaluated by a pediatric neuroradiologist and a pediatric neurosurgeon. Each MRI was evaluated for diagnostic quality to assess the ventricular size and extra-axial CSF spaces, and patients were categorized with the following diagnoses: ventriculomegaly/hydrocephalus, intracranial cysts, and macrocephaly. Inclusion criteria were as follows:
No follow-up standard brain MRI required after the UFB-MRI for the indicated diagnosis.
If clinical presentation, neurologic examination and UFB-MRI were diagnostic for patient discharge from pediatric neurosurgery.
Cases that required additional standard MRI were reviewed to assess whether additional imaging contributed to the indicated diagnosis.
All cases followed up clinically or radiographically for at least 6 months, unless discharged from care.
Ventriculomegaly diagnosis included etiologies of congenital or acquired origin (eg, secondary to intraventricular hemorrhage, post traumatic injury, or follow-up of ventriculomegaly secondary to tumor) or idiopathic origin. Intracranial cysts were defined as arachnoid, intraventricular, leptomeningeal, choroid plexus, or germinolytic. For postoperative tumor cases, UFB-MRI did not replace standard contrast-enhanced postoperative MRI.
Results
The radiology information system identified 800 patients who had UFB-MRI during the study period. Of these 800 patients, 122 met the study criteria based on their imaging diagnosis. Twenty-one of the 122 did not meet the follow-up criteria either due to moving out of state without adequate follow-up, not presenting for their scheduled clinical appointments, or having less than 6 months imaging/clinical follow-up.
We used the presence of additional MRI following UFB-MRI as a surrogate for insufficiency of UFB-MRI. Five patients had a standard brain MRI completed after UFB-MRI for the same indication. However, UFB-MRI was still deemed diagnostic for the indicated purposes in these cases: 1) A patient with ventriculomegaly was also noted to have a Chiari I malformation. He had an endoscopic third ventriculostomy based on the UFB-MRI and then had standard brain and spine MRI under anesthesia following his operation to further assess the Chiari I malformation. 2) A patient with ventriculomegaly had a routine follow-up study that included CISS imaging months later to assess aqueductal stenosis, though no significant additional diagnostic information was obtained. 3 and 4) Two patients with hydrocephalus were treated with endoscopic third ventriculostomy; they had endoscopic third ventriculostomy protocol brain MRIs (including CISS and cine) postoperatively as part of routine postoperative protocol. 5) A patient with an intracranial cyst underwent a standard brain MRI on long-term follow-up after an operation for cyst fenestration, including CISS imaging.
Fourteen other patients underwent standard brain MRI following UFB-MRI; however, the UFB-MRI was sufficient for the indicated diagnosis because the standard MRI was performed for an alternate diagnosis: Eleven of the 14 were patients with ventriculomegaly. The indication for the standard MRI was vascular malformation (n = 3), postoperative tumor (n = 6), and myelomeningocele (entire neuroaxis MRI, n = 2); 3 of the 14 had intracranial cysts: All 3 had preoperative navigation studies. No adverse outcomes were noted in these 14 patients during the study period related to imaging.
There were 65 males and 57 females, 0.003–17.63 years of age (average, 3.21 ± 4.40 years; median, 1.12 years). Ninety-seven of 122 (79.5%) patients were 5 years of age or younger, 79/122 (64.8%) were 1 year of age or younger, and 57/122 (46.7%) were younger than 1 year of age (Table). Ventriculomegaly was seen in 84/122 (44 males and 40 females): Sixty-five of 84 (77.3%) were 5 years of age or younger, 57/84 (67.9%) were 1 year of age or younger, and 41/84 (48.8%) were younger than 1 year of age. Macrocephaly was seen in 18/122 (13 males and 5 females): Eighteen of 18 (100%) patients were 5 years of age or younger, 14/18 (77.8%) were 1 year of age or younger, and 9/18 (50%) were younger than 1 year of age. Intracranial cysts were seen in 20/122 (8 males and 12 females): Fourteen of 20 (70%) were 5 years of age or younger, 8/20 (40%) were 1 year of age or younger, and 7/20 (35%) were younger than 1 year of age.
Patient age and sex distribution per diagnosis
| Total | Male | Female | Age Range (yr) | Age (Mean) (yr) | Age (SD) (yr) | Age (Median) (yr) | 5 Years of Age or Younger | 1 Year of Age or Younger | Younger than 1 Year of Age | |
|---|---|---|---|---|---|---|---|---|---|---|
| Ventriculomegaly | 84 | 44 | 40 | 0.003–17.63 | 3.28 | 4.64 | 1.05 | 65/84 (77%) | 57/84 (68%) | 41/84 (49%) |
| Macrocephaly | 18 | 13 | 5 | 0.2–4.42 | 1.26 | 1.09 | 0.98 | 18/18 (100%) | 14/18 (78%) | 9/18 (50%) |
| Cyst | 20 | 8 | 12 | 0.3–17.47 | 4.72 | 4.68 | 4.84 | 14/20 (70%) | 8/20 (40%) | 7/20 (35%) |
Discussion
UFB-MRI has proved safe and effective for imaging of shunted hydrocephalus.1,3,8,9 Ventriculomegaly, intracranial cysts, and macrocephaly, which often require imaging for diagnosis and management, are frequent referrals to the pediatric neurosurgery clinic in young children. Eighty percent of our cohort was 5 years of age or younger; 65%, 1 year of age or younger; and 47%, younger than 1 year of age. Our data demonstrate the young age of children for these diagnoses, further supporting the value of UFB-MRI to eliminate anesthesia/sedation for standard brain MRI or the risk of ionizing radiation. Rather than subjecting young children to radiation with head CT or anesthesia with a standard protocol brain MRI, we explored the utility of this radiation-free, anesthesia-/sedation-free UFB-MRI in indications beyond shunted hydrocephalus.
In our institution, UFB-MRI includes triplanar HASTE, which is a T2-weighted sequence. Acquisition time is short and relatively less motion-sensitive. In addition, the single-slice acquisition allows interrupting the image acquisition during moments of patient movement. Therefore, for this study, we only included patients in which assessment of CSF-containing spaces/structures was the primary objective, such as ventriculomegaly, intracranial cyst, or macrocephaly.
We did not have to exclude any UFB-MRI due to motion artifacts because it, in part, relies on our triplanar (axial, coronal, and sagittal) imaging. In case there was motion in 1 imaging plane, at least 1 other imaging plane proved to be free of motion artifacts, providing the required information. In all patients, UFB-MRI was deemed sufficient for diagnosis or follow-up of ventriculomegaly, intracranial cyst, or macrocephaly with adequate clinical/neurologic follow-up. In 5 patients where standard brain MRI was performed, all imaging was performed to further evaluate with advanced MRI sequences like CISS or CSF flow studies—information from these sequences would also not be obtained from head CT or conventional brain MRI sequences. We used clinical care/follow-up as our criterion standard rather than comparing UFB-MRI with standard brain MRI or head CT to avoid anesthesia/sedation or radiation.
In the past decade, “modified” fast brain MRI protocols have emerged, especially in children with traumatic brain injuries.10,11 Guided by medical indications, each hospital sets their neuroimaging protocols based on their resources, such as scanner availability, staffing, and other urgent indications. Most of the modified protocols have diffusion-weighted imaging to look for ischemic injury and susceptibility-weighted imaging to look for hemorrhagic injuries. Although additional sequences are necessary for these indications, a UFB-MRI protocol with HASTE without any other added sequences is sufficient in patients with ventriculomegaly, intracranial cysts, and macrocephaly because CSF-containing structures are the primary area of concern.
UFB-MRI is “quick” and does not require sedation or anesthesia. Still, incorporating this technique into a routine MRI schedule 24 hours a day, 7 days a week, may be challenging. Work flow changes require a coordinated effort between pediatric neuroradiology and the provider's department as well as support of the radiology department administration.14 Tekes et al15 previously published information on how to incorporate UFB-MRI into clinical routine following lean six sigma methodology; however, each institution may need to work on a work flow that best fits their internal resources. Variable practices were noted, depending on the resources and provider team's preferences and experience. In urgent cases in which UFB-MRI is not possible, head CT does remain an alternative, but to minimize the radiation in these cases, optimized low-dose pediatric head CT protocols should be used.16
We recognize the limitations of UFB-MRI, especially in the assessment of parenchymal diseases with a wide range of etiologies, including but not limited to myelination, cortical development, brain tumors, ischemia/stroke, and intracranial hemorrhages.8,12,17 Thus, UFB-MRI should not be used as a “quick scan” to evaluate these diseases.
We are proposing specific additional indications for UFB-MRI beyond the most commonly used and published indication, shunted hydrocephalus, and we used stringent inclusion criteria in our patient population (requiring either discharge from medical care for the stated indication or at least 6 months of clinical and/or imaging follow-up). Because we practice in a quaternary care children's center where we receive out-of-state and international patients, some loss to follow-up is inevitable. Some patients not meeting the stringent inclusion criteria does not reflect on the utility of the UFB-MRI.
Conclusions
Our data validate using UFB-MRI for indications like ventriculomegaly, macrocephaly, and intracranial cysts without impacting diagnostic accuracy in children. The elimination of radiation and sedation/anesthesia is magnified in its impact on patient safety due to the young age of the patient population typically presenting for evaluation of these diagnoses.
ABBREVIATION:
- UFB-MRI
ultrafast brain MRI
Footnotes
Disclosures: Thierry A.G.M. Huisman—UNRELATED: Board Membership: editorial board of the American Journal of Neuroradiology.
References
- 1. Penzkofer AK, Pfluger T, Pochmann Y, et al. . MR imaging of the brain in pediatric patients: diagnostic value of HASTE sequences. AJR Am J Roentgenol 2002;179:509–14 10.2214/ajr.179.2.1790509 [DOI] [PubMed] [Google Scholar]
- 2. Forbes KP, Pipe JG, Karis JP, et al. . Brain imaging in the unsedated pediatric patient: comparison of periodically rotated overlapping parallel lines with enhanced reconstruction and single-shot fast spin-echo sequences. AJNR Am J Neuroradiol 2003;24:794–98 [PMC free article] [PubMed] [Google Scholar]
- 3. Ashley WW Jr, McKinstry RC, Leonard JR, et al. . Use of rapid-sequence magnetic resonance imaging for evaluation of hydrocephalus in children. J Neurosurg 2005;103(2 Suppl):124–30 10.3171/jns.2005.103.1.0124 7 [DOI] [PubMed] [Google Scholar]
- 4. Brenner DJ, Hall EJ. Computed tomography: an increasing source of radiation exposure. N Engl J Med 2007;357:2277–84 10.1056/NEJMra072149 [DOI] [PubMed] [Google Scholar]
- 5. Malviya S, Voepel-Lewis T, Prochaska G, et al. . Prolonged recovery and delayed side effects of sedation for diagnostic imaging studies in children. Pediatrics 2000;105:E42 10.1542/peds.105.3.e42 [DOI] [PubMed] [Google Scholar]
- 6. Vanderby SA, Babyn PS, Carter MW, et al. . Effect of anesthesia and sedation on pediatric MR imaging patient flow. Radiology 2010;256:229–37 10.1148/radiol.10091124 [DOI] [PubMed] [Google Scholar]
- 7. Simon TD, Riva-Cambrin J, Srivastava R, et al. ; Hydrocephalus Clinical Research Network. Hospital care for children with hydrocephalus in the United States: utilization, charges, comorbidities, and deaths. J Neurosurg Pediatr 2008;1:131–37 10.3171/PED/2008/1/2/131 [DOI] [PubMed] [Google Scholar]
- 8. Sugahara T, Korogi Y, Hirai T, et al. . Comparison of HASTE and segmented-HASTE sequences with a T2-weighted fast spin-echo sequence in the screening evaluation of the brain. AJR Am J Roentgenol 1997;169:1401–10 10.2214/ajr.169.5.9353469 [DOI] [PubMed] [Google Scholar]
- 9. Iskandar BJ, Sansone JM, Medow J, et al. . The use of quick-brain magnetic resonance imaging in the evaluation of shunt-treated hydrocephalus. J Neurosurg 2004;101(2 Suppl):147–51 [DOI] [PubMed] [Google Scholar]
- 10. Roguski M, Morel B, Sweeney M, et al. . Magnetic resonance imaging as an alternative to computed tomography in select patients with traumatic brain injury: a retrospective comparison. J Neurosurg Pediatr 2015;15:529–34 10.3171/2014.10.PEDS14128 [DOI] [PubMed] [Google Scholar]
- 11. Ryan ME, Jaju A, Ciolino JD, et al. . Rapid MRI evaluation of acute intracranial hemorrhage in pediatric head trauma. Neuroradiology 2016;58:793–99 10.1007/s00234-016-1686-x [DOI] [PubMed] [Google Scholar]
- 12. Singh RK, Smith JT, Wilkinson ID, et al. . Ultrafast MR imaging in pediatric neuroradiology. Acta Radiol 2003;44:550–57 [DOI] [PubMed] [Google Scholar]
- 13. Missios S, Quebada PB, Forero JA, et al. . Quick-brain magnetic resonance imaging for nonhydrocephalus indications. J Neurosurg Pediatr 2008;2:438–44 10.3171/PED.2008.2.12.438 [DOI] [PubMed] [Google Scholar]
- 14. Durand DJ, Kohli MD. Advanced practice quality improvement project: how to influence physician radiologic imaging ordering behavior. J Am Coll Radiol 2014;11(12 Pt A):1155–59 10.1016/j.jacr.2014.08.034 [DOI] [PubMed] [Google Scholar]
- 15. Tekes A, Jackson EM, Ogborn J, et al. . How to reduce head CT orders in children with hydrocephalus using the lean six sigma methodology: experience at a major quaternary care academic children's center. AJNR Am J Neuroradiol 2016;37:990–96 10.3174/ajnr.A4658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pindrik J, Huisman TA, Mahesh M, et al. . Analysis of limited-sequence head computed tomography for children with shunted hydrocephalus: potential to reduce diagnostic radiation exposure. J Neurosurg Pediatr 2013;12:491–500 10.3171/2013.8.PEDS1322 [DOI] [PubMed] [Google Scholar]
- 17. Rozovsky K, Ventureyra EC, Miller E. Fast-brain MRI in children is quick, without sedation, and radiation-free, but beware of limitations. J Clinical Neurosci 2013;20:400–05 10.1016/j.jocn.2012.02.048 [DOI] [PubMed] [Google Scholar]