Abstract
Opiates are addicting and have a high potential for dependency. In the past decades, opiates remained the first-line pharmaceutical option of prehospital treatment for acute traumatic pain in the civilian population. Ketamine is an N-methyl-d-aspartate (NMDA) receptor antagonist that has analgesic properties and may serve as an alternative agent for the treatment of acute traumatic pain in prehospital settings. This study aims to assess the safety and efficacy of ketamine administration by paramedics in civilian prehospital settings for the treatment of acute traumatic pain.
This was a prospective observational study in San Bernardino, Riverside and Stanislaus counties. Patients were included if they were > 15 years of age with complaints of traumatic or burn-related pain. Patients were excluded if they received opiates up to six hours prior to or concurrently with ketamine administration. The dose administered was 0.3 mg/kg intravenously over five minutes with a maximum dose of 30 mg. The option to administer a second dose was available to paramedics if the patient continued to have pain after 15 minutes following the first administration. Paired-T tests were conducted to assess the change in the primary outcome (pain score) and secondary outcomes (e.g. systolic blood pressure, pulse, and respiratory rate). P-value<0.05 was considered to be statistically significant.
A total of 368 patients were included in the final analysis. The average age was 52.9 ± 23.1 years, and the average weight was 80.4 ± 22.2 kg. There was a statistically significant reduction in the pain score (9.13 ± 1.28 vs 3.7 ± 3.4, delta=5.43 ± 3.38, p<0.0001). Additionally, there was a statistically significant change in systolic blood pressure (143.42 ± 27.01 vs 145.65 ± 26.26, delta=2.22 ± 21.1, p=0.044), pulse (88.06 ± 18 vs 84.64 ± 15.92, delta= -3.42 ± 12.12, p<0.0001), and respiratory rate (19.04 ± 3.59 vs 17.74 ± 3.06, delta=-1.3 ± 2.96, p<0.0001).
The current study suggested that paramedics are capable of safely identifying the appropriate patients for the administration of sub-dissociative doses of ketamine in the prehospital setting. Furthermore, the current study suggested that ketamine may be an effective analgesic in a select group of adult trauma patients.
Keywords: ketamine, civilian, adult, prehospital
Introduction
The medicinal effects of opium have been exploited for centuries, long before the synthesis of the first opiate drug. However, the extent of its addictive properties were not evident until the last several decades. Currently, 11.4 million people misuse prescription opiates in the United States, with an estimated 130 people dying every day from opioid-related drug overdoses [1]. In 2017, more than 47,600 deaths were attributed to opioid overdose. The cost of this epidemic in 2013 estimated almost $78.5 billion [2]. The economic burden of opiate addiction and misuse is projected to increase as opiate prescriptions are still readily distributed, with an estimated 58.5 per 100 Americans receiving an opiate prescription in 2017 [3]. Despite this public health emergency, opiates remain a first-line pharmaceutical option for patients with acute pain. In the prehospital setting, opiates - morphine and fentanyl - remain the recommended means of treatment for moderate to severe pain [4]. Alternative means of treating acute traumatic pain in a prehospital setting have been proposed, including the use of non-steroidal anti-inflammatory drugs. However, no unequivocal data existed to support a clinically significant reduction in pain with use of nonsteroidal anti-inflammatory drugs (NSAIDs) in the prehospital setting [5].
Ketamine may be a non-opioid alternative used for pain management. In 1982, Lodge et al. conclusively demonstrated that ketamine acts as an N-methyl-d-aspartate (NMDA) receptor antagonist [6]. However, further research showed that ketamine may also have opiate-receptor specific binding capacity, thus eliciting an analgesic effect [7]. Ketamine’s efficacy as an analgesic was first described in 1971 [8]. Since then, several studies have demonstrated the efficacy of ketamine as an analgesic in the hospital setting [9-12]. The vast majority of data available for pre-hospital administration of ketamine reflects on its utilization in military and combat environments [13-18].
To date, there were limited data on the use of ketamine in the civilian prehospital environment as an analgesic. This study aimed to evaluate the safety and efficacy of paramedic administration of ketamine as a prehospital analgesic in traumatically injured civilian patients. We hypothesize that the administration of ketamine in the prehospital setting by paramedics is safe and effective in reducing pain.
Materials and methods
A prospective observational study was conducted by paramedics representing 30 advanced life support (ALS) transport providers in three California counties (San Bernardino, Riverside and Stanislaus). Prior authorization was obtained from Local Emergency Medical Services Agencies. Additionally, the protocol was approved by the Institutional Review Board at Arrowhead Regional Medical Center (Colton, CA). An oversight committee in each participating county regularly reviewed the data and addressed any discrepancies during the study period. The paramedics participating in the study were trained by their respective participating agencies regarding the ketamine administration inclusion and exclusion criteria and appropriate documentation. Patients were included in the study if they: were at least 15 years of age; had experienced an acute traumatic or burn injury; had a Glasgow Coma Scale (GCS) score of 15; would normally receive analgesia during routine care and/or transport, and had a pain score of at least “5” on a scale of 0 - 10, with 0 meaning “no pain” and 10 meaning “extremely severe pain”. The exclusion criteria were: GCS 14 or less; known or suspected pregnancy; known allergy to ketamine; known or suspected alcohol or drug intoxication; having received narcotic analgesia in any form within six hours of planned ketamine administration; and pain score less than "5" prior to the first dose of ketamine. Paramedics assessed each patient for the source of the pain to determine whether the pain was somatic or visceral. Paramedics were taught that visceral pain or chronic pain is less likely to respond to ketamine, and they should choose a different analgesic in those circumstances. However, if the patient met the inclusion criteria, then ketamine was preferred.
Pain was assessed on a visual analogue pain scale ranging from 0 (no pain) to 10 (most severe pain). Pain assessment was performed by a paramedic prior to administration of ketamine. Reassessment of pain was performed every five minutes following administration. The pain scale measured at 15 minutes was used as the final pain scale. EMS personnel were instructed to document age, weight, chief complaint, initial vital signs (including systolic blood pressure), Glasgow coma scale, as well as past medical history, allergies and home medications used by the patient.
Paramedics were instructed to administer 0.3 mg/kg (max dose 30 mg) of ketamine as slow intravenous push over five minutes. An additional dose of 0.3 mg/kg (max dose 30 mg) was permitted if pain severity remained greater than five on the pain scale, 15 minutes following first administration. The time of ketamine administration and total dose were documented in the electronic patient care report, as well as any observed adverse effects.
All statistical analyses were conducted using the SAS software for Windows version 9.3 (Cary, North Carolina, USA). Descriptive statistics were presented as means and standard deviations for continuous variables, along with frequencies and proportions for categorical variables. Change in the pain scale and vital signs were analyzed using the paired T-test. Change in the pain scale was also compared between those who received one vs two doses of ketamine using independent T-test. All statistical analyses were two-sided. P-value<0.05 was considered to be statistically significant.
Results
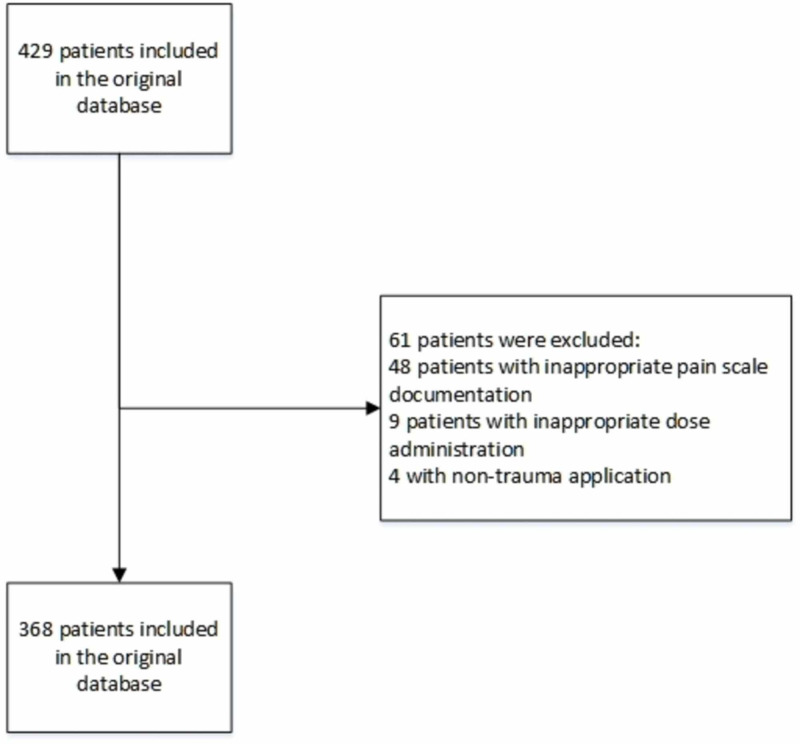
Among the original 429 patients, 368 patients were included in the final analysis. Figure 1 presents the patient flow chart. The average age was 52.9 ± 23.1 years old, and the average weight was 80.4 ± 22.2 kg. The median transport time from the first administration to arrival at the hospital was 18 minutes (first quartile=12 minutes, third quartile=27 minutes).
Figure 1. Patients Flow Chart.
The change of pain score and vital signs were compared using a paired T-test. The analysis results were presented in Table 1. There was a statistically significant reduction in the pain score (9.13 ± 1.28 vs 3.7 ± 3.4, delta=5.43 ± 3.38, p<0.0001). Additionally, there was a statistically significant change in SBP (143.42 ± 27.01 vs 145.65 ± 26.26, 2.22 ± 21.1, p=0.0440), pulse (88.06 ± 18 vs 84.64 ± 15.92, delta= -3.42 ± 12.12, p<0.0001), and respiratory rate (19.04 ± 3.59 vs 17.74 ± 3.06, delta=-1.3 ± 2.96, p<0.0001).
Table 1. Change of Pain Score and Vital Signs Pre and Post Administration of Ketamine .
| Pre | Post | Delta (Post Less Pre) | P-value | |
| Pain Score | 9.13 ± 1.28 | 3.7 ± 3.4 | -5.43 ± 3.38 | <0.0001 |
| Systolic BP | 143.42 ± 27.01 | 145.65 ± 26.26 | 2.22 ± 21.1 | 0.044 |
| Diastolic BP | 82.67 ± 17.41 | 84.42 ± 18.76 | 1.75 ± 18.29 | 0.069 |
| Pulse | 88.06 ± 18 | 84.64 ± 15.92 | -3.42 ± 12.12 | <0.0001 |
| Respiratory Rate | 19.04 ± 3.59 | 17.74 ± 3.06 | -1.3 ± 2.96 | <0.0001 |
A total of 58 (15.8%) patients received a second dose of ketamine. A subgroup analysis of change in pain score and vital signs was compared between cohorts who received one vs two doses of ketamine. The analysis results were presented in Table 2. First, among patients who received one dose of ketamine, there was a statistically significant reduction in the pain score (9.05 ± 1.32 vs 3.5 ± 3.35, delta=-5.55 ± 3.35, p<0.0001). Additionally, there was a statistically significant change in pulse (87.64 ± 18.03 vs 84.18 ± 15.91, delta= -3.47 ± 12.08, p<0.0001), and respiratory rate (18.98 ± 3.65 vs 17.73 ± 3.14, delta=-1.24 ± 2.95, p<0.0001). Second, among patients who received two doses of ketamine, there was statistically significant reduction in the pain score (9.59 ± 0.92 vs 4.76 ± 3.5, delta=-4.83 ± 3.53, p<0.0001). Additionally, there was a statistically significant change in respiratory rate (19.37 ± 3.28 vs 17.8 ± 2.64, delta=-1.57 ± 2.99, p=0.0003). Lastly, there was no statistically significant difference in the change of pain score and vital signs between patients who received one vs two doses of ketamine (all p-values>0.05).
Table 2. Comparison of Change in Pain Score and Vital Signs Between Ketamine Doses.
P-value1 was comparing the change of pain score and vital signs among patients who received one dose of ketamine
P-value2 was comparing the change of pain score and vital signs among patients who received two doses of ketamine
P-value3 was comparing the comparing the change of pain score and vital signs between patients who receive one vs two doses of ketamine.
| One Dose of Ketamine (n=310) | Two Dose of Ketamine (n=58) | ||||||||
| Pre | Post | Delta (Post Less Pre) | P-value1 | Pre | Post | Delta (Post Less Pre) | P-value2 | P-value3 | |
| Pain Score | 9.05 ± 1.32 | 3.5 ± 3.35 | -5.55 ± 3.35 | <0.0001 | 9.59 ± 0.92 | 4.76 ± 3.5 | -4.83 ± 3.53 | <0.0001 | 0.1368 |
| Systolic BP | 142.41 ± 26.29 | 144.47 ± 26.11 | 2.06 ± 20.71 | 0.08 | 148.86 ± 30.24 | 151.93 ± 26.37 | 3.07 ± 23.23 | 0.3186 | 0.7398 |
| Diastolic BP | 81.95 ± 16.36 | 83.64 ± 18.93 | 1.7 ± 18.16 | 0.103 | 86.56 ± 21.99 | 88.6 ± 17.36 | 2.04 ± 19.14 | 0.4255 | 0.898 |
| Pulse | 87.64 ± 18.03 | 84.18 ± 15.91 | -3.47 ± 12.08 | <0.0001 | 90.3 ± 17.85 | 87.11 ± 15.89 | -3.19 ± 12.41 | 0.057 | 0.8756 |
| Respiratory Rate | 18.98 ± 3.65 | 17.73 ± 3.14 | -1.24 ± 2.95 | <0.0001 | 19.37 ± 3.28 | 17.8 ± 2.64 | -1.57 ± 2.99 | 0.0003 | 0.4548 |
The complications associated with ketamine were reported in Table 3. Overall, 86.7% (n=319) did not have any complications, and the most prevalent complication was dysphoria (6.3%, n=23). The same pattern of complications apply to patients regardless whether they received one or two doses of ketamine.
Table 3. Complications Associated With Administration of Ketamine.
| Overall | 1 dose | 2 doses | |
| Apnea | 1 (0.3%) | 1 (0.3%) | 0 (0%) |
| Dizziness | 11 (3%) | 10 (3.2%) | 1 (1.7%) |
| Dysphoria | 23 (6.3%) | 20 (6.5%) | 3 (5.2%) |
| Euphoria | 1 (0.3%) | 0 (0%) | 1 (1.7%) |
| Headache | 1 (0.3%) | 1 (0.3%) | 0 (0%) |
| Hypotension | 1 (0.3%) | 1 (0.3%) | 0 (0%) |
| Nausea | 10 (2.7%) | 9 (2.9%) | 1 (1.7%) |
| None | 319 (86.7%) | 267 (86.1%) | 52 (89.7%) |
| Vomiting | 1 (0.3%) | 1 (0.3%) | 0 (0%) |
Discussion
The current study suggested the effective reduction of acute pain with the use of sub-dissociative doses of ketamine in the prehospital setting. Furthermore, the treatment of pain was not associated with clinically significant adverse effects. While dysphoria was described in a small percentage of patients, hemodynamic instability or respiratory depression were not witnessed. In contrast, opiates, while effective in reducing pain, have a known side effect profile of respiratory depression and hypotension. Similar findings were reported in the literature. One systematic review and meta-analysis, including six trials and 438 patients, suggested that ketamine’s analgesic effects to be similar or superior to placebo or opiates, and while ketamine potentially had increased risk of neurological and psychological adverse effects, the opioid group had a higher risk of major cardiopulmonary events [19].
Other studies have evaluated the use of ketamine in conjunction with opiates to treat acute pain in the emergency department. These studies aim to determine if co-administration reduces the overall use of opiates, and consequentially, the associated adverse effects. The results demonstrate a clinically significant reduction in pain, comparable to opiate alone, with less need for rescue analgesia and decreased incidence of clinically deleterious adverse effects [9].
The opioid epidemic has increased the demand for a less-addictive alternative pharmacologic means of treating acute pain. Several studies demonstrated anti-depressant and anti-addiction properties of ketamine. One study suggested that ketamine may be used to treat addiction by decreasing the incentive-motivational value of reward-related cues [20]. Other studies have shown a prolongation of abstinence from the use of alcohol and heroin in dependent individuals [21]. This suggests that ketamine may be less addicting when compared to opiates, and ketamine may actually aid in preventing addiction to other substances. An article suggested that ketamine’s effect on NMDA receptors on gamma-aminobutyric acid neurons in the thalamic reticular nucleus may lead to increased release of dopamine, thus leading to possible dependence [22]. Death from direct toxicity from ketamine use is rare [23]. In fact, a case report described a case of a patient taking 1-3 g of ketamine daily for multiple years without significant adverse effects. The patient described antidepressant effects, as well as diminished cravings for alcohol [24].
This study has several limitations. First, this study focused on the prehospital setting, and was therefore limited in its capacity to assess whether the use of ketamine may lead to dependence or addiction. However, research has reported the anti-addiction property of ketamine [20-22]. A prospective cohort study with a longer follow-up period is warranted to verify the anti-addiction property of ketamine reported by the research community. Second, prehospital transport time may vary. Longer transportation may increase the total amount of ketamine administered, or demand repeat doses. Conversely, shorter transport time may not have provided sufficient time to establish IV access or administer ketamine as slow intravenous push. Consideration of alternative means of administering ketamine, including intranasal or intramuscular, may potentially circumvent this limitation. Last, severity of traumatic or burn injuries were not provided in the electronic patient care report. Increasing severity of injury may require increased dose, repeat dose, or alternative mechanisms of analgesia for sufficient pain control. One study suggests that Injury Severity Score > 15 required additional doses of analgesia [25]. Furthermore, increased severity of injuries may lead to an increased likelihood of hemodynamic instability following analgesic administration. The current study suggested the positive effect of ketamine administration on systolic blood pressure.
The current research was presented as a podium presentation at the 10th Mediterranean Emergency Medicine Congress in Dubrovnik, Croatia in September 2019. The abstract was published in Western Journal of Emergency Medicine Volume 20 Supplement (5.1). The web address for the published abstract was https://escholarship.org/uc/item/40k6b3fx.
Conclusions
There is sufficient support for the use of ketamine as a safe alternative to opiates for the treatment of acute pain. Ketamine’s use as an analgesic is well documented in the emergency department, perioperative and inpatient settings. Limited studies in combat demonstrate its efficacy in the prehospital setting. As this study suggests, its use as an analgesic may be expanded to include prehospital administration for civilian populations. Our assessment via the NRS, demonstrated an absolute reduction of pain following the administration of ketamine. Ketamine is safe to administer as slow intravenous push. The trial did not demonstrate severe adverse effects, including hemodynamic instability or respiratory failure. Ketamine appears to be a suitable alternative to opiates for analgesia in the prehospital setting.
Future studies are needed to evaluate for the potential of dependence and abuse, determining the safety and efficacy of ketamine use in the pediatric population, and alternative routes of administration, including intranasal and intramuscular.
Acknowledgments
We thank Dr. Tyler Mitchell for his help with editing of the manuscript. We would like to send a special thank you to the men and women of the ground emergency medical service agencies in the San Bernardino, Riverside, and Stanislaus County who participated in this study.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study. Arrowhead Regional Medical Center IRB issued approval 18-20
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.U.S. Department of Health and Human Services. What is the U.S. opioid epidemic? [May;2019 ];https://www.hhs.gov/opioids/about-the-epidemic/index.html 2019
- 2.The economic burden of prescription opioid overdose, abuse and dependence in the United States, 2013. Florence C, Luo F, Xu L, Zhou C. Med Care. 2016;54:901–906. doi: 10.1097/MLR.0000000000000625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Opioid overdose. [May;2019 ];https://www.cdc.gov/drugoverdose/data/prescribing.html 2019
- 4.An evidence-based guideline for prehospital analgesia in trauma. Gausche-Hill M, Brown KM, Oliver ZJ, et al. Prehosp Emerg Care. 2014;18:25–34. doi: 10.3109/10903127.2013.844873. [DOI] [PubMed] [Google Scholar]
- 5.Review on pharmacological pain management in trauma patients in (pre‐hospital) emergency medicine in the Netherlands. Dijkstra B, Berben S, Van Dongen R, Schoonhoven L. Eur J Pain. 2014;18:3–19. doi: 10.1002/j.1532-2149.2013.00337.x. [DOI] [PubMed] [Google Scholar]
- 6.Effects of optical isomers of ketamine on excitation of cat and rat spinal neurones by amino acids and acetylcholine. Lodge D, Anis N, Burton N. Neurosci Lett. 1982;29:281–286. doi: 10.1016/0304-3940(82)90330-5. [DOI] [PubMed] [Google Scholar]
- 7.Opiate receptor mediation of ketamine analgesia. Finck AD, Ngai S. https://anesthesiology.pubs.asahq.org/article.aspx?articleid=1956935. Anesthesiology. 1982; 56:291–297. doi: 10.1097/00000542-198204000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Analgesic effects of ketamine administered in subdissociative doses. Sadove MS, Shulman M, Hatano S, Fevold N. https://journals.lww.com/anesthesia-analgesia/Citation/1971/05000/Analgesic_Effects_of_Ketamine_Administered_in.37.aspx. Anesth Analg. 1971;50:452–457. [PubMed] [Google Scholar]
- 9.Low‐dose ketamine improves pain relief in patients receiving intravenous opioids for acute pain in the emergency department: results of a randomized, double‐blind, clinical trial. Beaudoin FL, Lin C, Guan W, Merchant RC. Acad Emerg Med. 2014;21:1193–1202. doi: 10.1111/acem.12510. [DOI] [PubMed] [Google Scholar]
- 10.Analgesia in patients with trauma in emergency medicine: a systematic review and meta-analysis. Häske D, Böttiger BW, Bouillon B, et al. Dtsch Arztebl Int. 2017;114:785–792. doi: 10.3238/arztebl.2017.0785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Intravenous subdissociative-dose ketamine versus morphine for analgesia in the emergency department: a randomized controlled trial. Motov S, Rockoff B, Cohen V, et al. Ann Emerg Med. 2015;66:222–229. doi: 10.1016/j.annemergmed.2015.03.004. [DOI] [PubMed] [Google Scholar]
- 12.Management of severe acute pain in emergency settings: ketamine reduces morphine consumption. Galinski M, Dolveck F, Combes X, et al. Ann Emerg Med. 2007;25:385–390. doi: 10.1016/j.ajem.2006.11.016. [DOI] [PubMed] [Google Scholar]
- 13.Ketamine for prehospital trauma analgesia in a low-resource rural trauma system: a retrospective comparative study of ketamine and opioid analgesia in a ten-year cohort in Iraq. Losvik OK, Murad MK, Skjerve E, Husum H. https://sjtrem.biomedcentral.com/articles/10.1186/s13049-015-0176-1. Scand J Trauma Resusc Emerg Med. 2015;23:94. doi: 10.1186/s13049-015-0176-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.A comparison of ketamine and morphine analgesia in prehospital trauma care: a cluster randomized clinical trial in rural Quang Tri province, Vietnam. Tran KP, Nguyen Q, Truong XN, et al. Prehosp Emerg Care. 2014;18:257–264. doi: 10.3109/10903127.2013.851307. [DOI] [PubMed] [Google Scholar]
- 15.Multicenter, prospective study of prehospital administration of analgesia in the US combat theater of Afghanistan. Schauer SG, Mora AG, Maddry JK, Bebarta VS. Prehosp Emerg Care. 2017;21:744–749. doi: 10.1080/10903127.2017.1335814. [DOI] [PubMed] [Google Scholar]
- 16.Ketamine for military prehospital analgesia and sedation in combat casualties. Moy Moy, Wright C. J R Army Med Corps. 2018;164:436–437. doi: 10.1136/jramc-2018-000910. [DOI] [PubMed] [Google Scholar]
- 17.Trends in prehospital analgesia administration by US forces from 2007 through 2016. Schauer SG, Naylor JF, Maddry JK, Hinojosa-Laborde C, April MD. Prehosp Emerg Care. 2019;23:271–276. doi: 10.1080/10903127.2018.1489022. [DOI] [PubMed] [Google Scholar]
- 18.Prehospital analgesia: systematic review of evidence. Park C, Roberts D, Aldington D, Moore R. J R Army Med Corps. 2010;156:295–300. doi: 10.1136/jramc-156-04s-05. [DOI] [PubMed] [Google Scholar]
- 19.The effects of low-dose ketamine on acute pain in an emergency setting: a systematic review and meta-analysis. Lee EN, Lee JH. PLoS One. 2016;11:165461. doi: 10.1371/journal.pone.0165461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Subanesthetic ketamine decreases the incentive-motivational value of reward-related cues. Fitzpatrick CJ, Morrow JD. J Psychopharmacol. 2017;31:67–74. doi: 10.1177/0269881116667709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ketamine for the treatment of addiction: Evidence and potential mechanisms. Ezquerra-Romano II, Lawn W. Neuropharmacology. 2018;142:72–82. doi: 10.1016/j.neuropharm.2018.01.017. [DOI] [PubMed] [Google Scholar]
- 22.Ketamine abuse potential and use disorder. Liu Y, Lin D, Wu B, Zhou W. Brain Res Bull. 2016;126:68–73. doi: 10.1016/j.brainresbull.2016.05.016. [DOI] [PubMed] [Google Scholar]
- 23.Ketamine: an update on its abuse. Bokor G, Anderson PD. J Pharm Pract. 2014;27:582–586. doi: 10.1177/0897190014525754. [DOI] [PubMed] [Google Scholar]
- 24.Intensive ketamine use for multiple years: A case report. Liu JX, Zerbo E, Ross S. Am J Addict. 2015;24:7–9. doi: 10.1111/ajad.12153. [DOI] [PubMed] [Google Scholar]
- 25.Prehospital analgesia for pediatric trauma patients in Iraq and Afghanistan. Schauer SG, Arana AA, Naylor JF, Hill GJ, April MD. Prehosp Emerg Care. 2018;22:608–613. doi: 10.1080/10903127.2018.1428839. [DOI] [PubMed] [Google Scholar]