Abstract
HPV-related multiphenotypic sinonasal carcinoma (HMSC) is a recently described distinct tumor entity of the sinonasal tract associated with high-risk subtypes of human papilloma virus (HPV), predominantly type 33. The biological behavior seems to be less aggressive than the often high-grade, highly proliferative morphology implies; however, recurrences are frequent. Most of the cases present as polypoid tumors within the nasal cavity. Microscopic morphology frequently encompasses adenoid cystic-like features or features reminiscent of other salivary gland tumors. Here, we describe four cases of this rare entity, all observed in women. The polypoid tumors were within the nasal cavity, leading to obstruction, facial pain and epistaxis. The morphology was predominantly basaloid, solid and adenoid cystic-like in two of four cases, one with additional glomeruloid features. Another case showed basaloid tumor cells with prominent mature squamous differentiation and extensive keratinization. A single case showed a predominantly solid and reticular growth pattern. All cases were diffusely positive for p16 (100%), expressed SOX10, LEF-1 and partially S-100, and harbored HPV high-risk types 33, 56 (2×) and 82. No recurrences or metastases were detectable after 3–50 months of follow-up. Of note, three of four patients were nurses/nursing assistant. We expand the morphological spectrum by describing a glomeruloid growth pattern and extensive mature keratinization, and add HPV type 82 to the molecular spectrum. The finding of HMSC among predominantly nurses in our cohort warrants further epidemiological studies in larger cohorts.
Keywords: Papillomaviridae, Carcinoma, Squamous cell, Paranasal sinus neoplasm, Health personnel, Multiphenotypic
Introduction
Human papilloma virus (HPV)-related multiphenotypic sinonasal carcinoma (HMSC) is a distinct carcinoma occurring in the sinonasal tract. It often manifests as a polypoid mass in the nasal cavity along with nasal congestion and epistaxis [1, 2]. In contrast to (non-keratinizing) oropharyngeal squamous cell carcinoma or nasal vestibule squamous cell carcinoma [3], it often shows adenoid cystic-like (biphasic) differentiation, leading to the initial description of HPV-related carcinoma with adenoid cystic-like features [4]. However, a variety of morphological patterns including other salivary-like differentiation (e.g. myoepithelial or epithelial-myoepithelial) and abrupt keratinization has been reported, expanding the morphological spectrum of HMSC [2, 5, 6].
The presence of HPV high-risk subtypes (typically type 33, 35 and 56), has been described in HMSC [2, 5]. Interestingly, current data indicate that these tumors are less aggressive than their often high-grade morphology would suggest. Only two of approximately 60 reported HMSC cases (~ 3%) presented with metastases (to the finger and lung) and no disease-specific deaths have been described, yet [1, 2]. Nevertheless, local recurrences are frequently encountered (up to 36%) [2], sometimes decades after the primary diagnosis (up to 30 years) [7, 8]. The exact pathogenesis or entry route of these less common HPV-types to the sinonasal tract remains largely unknown. In this study, we characterize the clinicopathological features of four more HMSC cases including first occupational data.
Materials and Methods
Patient Cohort
Pathological material and corresponding clinical data of four cases initially identified as HPV-related sinonasal carcinoma from June 2015 to March 2019 was obtained from the archives of the Department of Pathology and Molecular Pathology, University Hospital Zurich, Zurich, Switzerland. All patients gave written consent and the study was approved by the local ethics committee (protocol number 2016-00162, incl. amendment of February 24th, 2018).
Morphology
All cases were reevaluated on 2 μm sections of hematoxylin and eosin (H&E) stained formalin-fixed paraffin embedded (FFPE) tissue by an experienced, board-certified head and neck pathologist (N.J.R.). Morphological patterns included basaloid, solid, cribriform, retiform, glomeruloid and biphasic (ductal-myoepithelial) differentiation, as well as surface involvement, consisting of atypical squamous cells.
Immunohistochemistry
The following primary antibodies were applied to 2 μm sections on a Ventana Benchmark automated staining system (Roche Ventana Medical Systems, Inc.): pancytokeratin (AE1/AE3, DAKO A/S, 1:50), p40 (BC28, Zytomed Systems, 1:100), p16 (E6H4, Ventana, prediluted), S-100 (DAKO A/S, polyclonal 1:2000). The optiView DAB-kit (Ventana) was used to detect binding and counterstaining with hematoxylin (Ventana) ensued. For SOX10 (BC34, Biocare Medical, 1:150) and LEF-1 (EPR2029Y, Abcam Ltd., 1:50) immunohistochemistry, the Bond device (Leica Biosystems) was applied and the Bond Polymer Refine Detection kit (DAB; Leica Biosystems) was used for detection.
HPV Analysis
DNA was extracted from representative tumor sections or punches of the respective paraffin block as described previously [9]. The PGMY09/11 and L1C1/2 primers were used for polymerase chain reaction (PCR) as described previously [10], and in one case, GP5+/6+ primers [11] were included. Specific amplificates were purified using either the Qiagen MiniElute gel extraction kit or the Qiagen MiniElutePCR purification kit. The purified PCR products were sequenced on an ABI 3100 genetic analyzer using Big Dye terminator chemistry (Applied Biosystems) and sequences were analyzed using the Sequencer 5.1 software (Gene Codes).
Statistical Analysis
Epidemiological data were obtained from the Swiss Federal Office for Statistics report 2014 [12]. Since the catchment area of our hospital represents about 1/8 of the general Swiss population, we assumed that the proportion of nurses in the general Swiss population is the same as in our patient population. The probability of encountering a defined proportion from the same occupational group in our small cohort by chance alone was calculated using the binomial test. 95% confidence intervals are indicated (95% CI). A P value < 0.01 was considered to indicate statistical significance. All statistical analyses were performed using R 3.6.1 statistical software.
Results
Clinical Presentation
All patients were female with ages between 46 and 65 years. They presented to our Department of Otorhinolaryngology, Head and Neck Surgery with complaints of nasal obstruction (100%). Two patients had additional unilateral facial pain and one patient reported epistaxis (Table 1). Clinical examination revealed a polypoid, pedunculated tumor in all patients, three of them arising from the nasal septum and one from the middle concha, which was seen on surgery. Tumors were classified as cT1 (2 cases), cT2 (1 case) and cT3 (1 case). Initial staging featuring neck ultrasound and cross-sectional imaging (computed tomography and magnetic resonance imaging for all patients) did not reveal spread of the carcinoma to the regional lymph nodes. The patient with the largest tumor (HMSC-4) showed signs suggestive of bone erosion of the lamina papyracea (orbital lamina) on cross-sectional imaging, a finding that was not confirmed intraoperatively. There was no evidence of immunosuppression in our patient cohort. One patient, case 3, had a history of smoking (30 pack-years).
Table 1.
Overview of the clinical parameters in the HPV-related multiphenotypic sinonasal carcinomas (HMSC)
| Case | Age (years) | Gender | Occupation | Symptoms | Localization | cTNM Classification | Treatment | Recurrence/metastasis | Total follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|
| HMSC-1 | 65 | Female | Logistician | Nasal obstruction, facial pain | Polypoid tumor left middle concha | cT1 cN0 cM0 | Endoscopic middle turbinectomy | NED | 50 |
| HMSC-2 | 54 | Female | Nursing assistant | Nasal obstruction, epistaxis | Polypoid tumor left nasal cavity, septum | cT1 cN0 cM0 | Endoscopic septectomy | NED | 38 |
| HMSC-3 | 46 | Female | Nurse | Nasal obstruction, facial pain | Polypoid tumor right nasal cavity, septum | cT2 cN0 cM0 | Endoscopic septectomy | NED | 30 |
| HMSC-4 | 60 | Female | Nurse | Nasal obstruction | Polypoid tumor right nasal cavity, septum | cT3 cN0 cM0 |
Endoscopic surgical transnasal transcribriform resection Postoperative IMRT 33 × 1.8 = 59.4 Gy Concomitant Cisplatin |
NED | 3 |
Local doses shown in italic
IMRT intensity modulated radiotherapy, NED no evidence of disease
Occupational Data
Three patients (out of four) were working as nurses or nursing assistant. Another worked in logistics. Details about the exact working area of the nurses/nursing assistant were not available, but it is known that all worked on a medical ward with regular patient contact. Due to the seemingly high proportion of nurses/nursing assistant among the patients, we made the following calculation based on data compiled from the Swiss Federal Office for Statistics in 2014. Of the 4,054,000 full-time employees in Switzerland, 124,000 (3.06%) were nurses. Since the approximate catchment area of our hospital comprises 1/8 of the Swiss population, we can assume similar distributions. In our study cohort, 3 of 4 patients (75%) shared the same occupation. Using a binomial test, the probability of the latter proportion to have occurred by chance alone is rather low (P = 0.0001118, 95% CI 19–99%).
Morphology
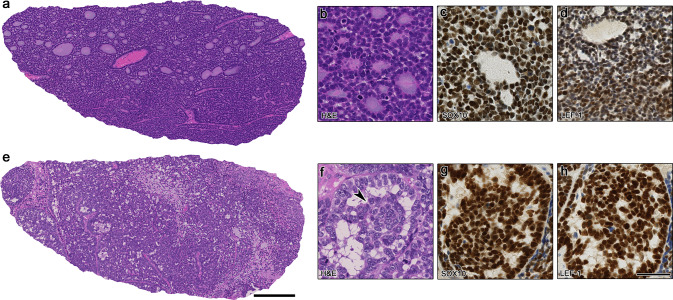
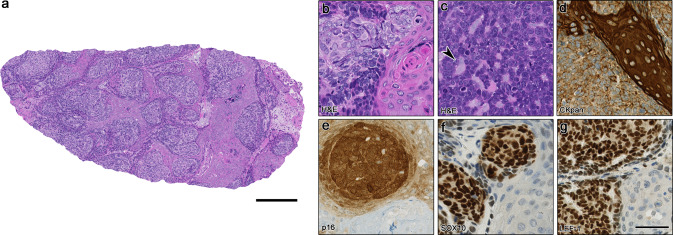
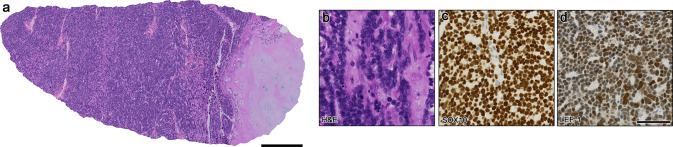
Resection specimen of all tumors confirmed the polypoid nature and revealed prominent basaloid tumor cells in all cases (100%) with abundant mitotic figures. The growth pattern was predominantly solid and lobular with tubular and cribriform areas reminiscent of adenoid cystic carcinoma in two cases (50%; Fig. 1a, b), whereas one case showed more pleomorphic cells and a glomeruloid pattern (Fig. 1e, f). One case showed an unusual prominent abrupt keratinization with plentiful mature squamous islands (HMSC-3; Fig. 2a, b). In one case, prominent reticular pattern was seen (HMSC-4; Fig. 3a, b) with infiltration into cartilage. Surface involvement of the adjacent mucosa was seen in two cases.
Fig. 1.
Morphological and immunohistochemical overview of the HPV-related multiphenotypic sinonasal carcinoma cases 1 and 2 (HMSC-1 and -2). a Shows an overview of HMSC-1 with basaloid small cells and adenoid cystic-like tubular/cribriform structures. In b magnification of monomorphic basaloid cells, forming duct-like structures can be appreciated. c and d Showing positivity for SOX10 and weak but distinct expression of LEF-1. e Depicts an overview of HMSC-2 with larger basaloid cells, focal cribriform and glomeruloid growth, and a reticular pattern (middle). In f the glomeruloid pattern is shown at higher magnification, consisting of central rotund tumor structures retracting from the periphery. g and h Showing diffuse expression of SOX10 and LEF-1 in the tumor cells. Scale bars 250 μm (a, e) and 50 μm (b–d, f–h)
Fig. 2.
Morphological and immunohistochemical overview of the HPV-related multiphenotypic sinonasal carcinoma case 3 (HMSC-3). In a an overview is depicted with islands of larger basaloid cells in lobules with abundant mature squamous islands and keratinization. b Shows magnification of the larger, somewhat brighter basaloid cells with adjacent keratinization. In c a limited focus of a more conventional morphology with smaller, monomorphic basaloid cells and duct formation (arrowhead) is seen. d Shows pancytokeratin staining, visualizing the heterogeneous expression within the basaloid tumor cells and strong, diffuse positivity in the mature squamous islands. In e strong, diffuse expression of p16 can be seen in the basaloid tumor cells, whereas the squamous islands (lower right corner) lacks p16 expression. A similar pattern can be observed for SOX10 and LEF-1 (f, g). Scale bars 250 μm (a) and 50 μm (b–g)
Fig. 3.
Morphological and immunohistochemical overview of the HPV-related multiphenotypic sinonasal carcinoma case 4 (HMSC-4). The overview in a shows monomorphic basaloid tumor cells infiltrating cartilage (right). The magnification b reveals the predominant reticular growth pattern and remarkable monomorphic, basaloid tumor cells with mitotic figures. In c the diffuse SOX10 expression is depicted, whereas d shows weak but distinct LEF-1 expression in the tumor cells. Scale bars 250 μm (a) and 50 μm (b–d)
Immunohistochemistry and HPV Typing
All cases (100%) were positive for pancytokeratin (Table 2), however, in an uncommon heterogenous expression pattern. In certain areas, a biphasic pattern (ductal-myoepithelial) could be identified. In case 3, mature squamous islands showed strong, diffuse pancytokeratin expression (Fig. 2d). Immunohistochemistry for p16 was positive in all cases, showing a strong, diffuse nuclear and cytoplasmic expression in virtually every basaloid tumor cell (100%). The mature squamous differentiation in case 3, however, lost p16 expression (Fig. 2e). S-100 showed a patchy, but distinct expression in all cases (100%). SOX10 was diffusely expressed in all cases (Figs. 1c, g, 2f, 3c); however, the prominent squamous islands in HMSC-3 were negative (Fig. 2f). The same expression pattern was noted for LEF-1, however less strong in intensity (Figs. 1d, h, 2g, 3d). HPV type 56 was identified in two cases; HPV type 82 and HPV type 33 were identified, each in one case, respectively.
Table 2.
Morphological and immunohistochemical patterns and HPV-types in the HPV-related multiphenotypic sinonasal carcinomas (HMSC)
| Case | Predominant morphology | Surface involvement | Pancytokeratin | p40 | p16 | S-100 | SOX-10 | LEF-1 | HPV-type |
|---|---|---|---|---|---|---|---|---|---|
| HMSC-1 | Basaloid, solid, tubular, cribriform | present | pos. (heterog.) | pos. (diffuse) | pos. (diffuse) | pos. (patchy) | pos. (diffuse) | pos. (weak) | HPV 56 |
| HMSC-2 | Basaloid, solid, cribriform, glomeruloid | not present | pos. (heterog.) | pos. (patchy) | pos. (diffuse). | pos. (patchy) | pos. (diffuse) | pos. (diffuse) | HPV 82 |
| HMSC-3 | Basaloid, prominent abrupt keratinization with squamous islands | present | pos. (heterog.) | pos. (diffuse) | pos. (diffuse); squamous islands neg. | pos. (patchy) | pos. (diffuse); squamous islands neg. | pos. (diffuse); squamous islands neg. | HPV 56 |
| HMSC-4 | Basaloid, solid, tubular, reticular | not present | pos. (heterog.) | pos. (diffuse) | pos. (diffuse) | pos. (patchy) | pos. (diffuse) | pos. (weak) | HPV 33 |
pos. positive, neg. negative
Treatment and Clinical Follow-Up
In all patients, tumors were removed surgically via an endoscopic approach. Adjuvant chemoradiation was performed in one case with cT3 stadium (HMSC-4). In the clinical follow up ranging from 3 to 50 months, no recurrences or metastatic spread could be detected.
Discussion
Here, we report four cases of the recently described, rare HPV-related multiphenotypic sinonasal carcinoma (HMSC) [2]. The clinical presentation with a polypoid tumor in the nasal cavity leading to nasal obstruction, epistaxis and pain is concordant with previous descriptions [2, 4–6]. In our cohort, only women were affected, whereas other cohorts comprised both genders [2] or were even males only [6]. We have not observed recurrences or metastatic spread in our cohort, yet; however our follow up is 50 months at the maximum and very late recurrences (16 and 30 years) have been observed [7, 8]. The morphology and HPV types (33, 56) were similar to other reports [2, 4–6]. Notably, one case in our series (HMSC-2) showed a prominent glomeruloid pattern with more pleomorphic cells and an associated HPV type 82, which to the best of our knowledge has not been described. This HPV type is rarely detected in cervical cancer, being phylogenetically similar [13] to the other types described in HMSC. Limited keratinization has been described previously [5, 6]. However, our case 3 (HMSC-3) showed extensive keratinization with mature squamous islands adjacent to basaloid tumor cells. Aggressive NUT carcinoma is therefore an important differential diagnosis and should be assessed by immunohistochemistry and/or molecular testing [14]. Our cases were all positive for SOX10, corroborating the previous description [15]. Interestingly, the extensive squamous differentiation in HMSC-3 lost expression of SOX10, LEF-1, p16, and was diffusely positive for pancytokeratin in contrast to the basaloid tumor cells, suggesting a metaplastic or maturing process. In this case, partial S-100 expression and focal ductal differentiation corroborated the diagnosis of HMSC. Another differential consideration is adamantinoma-like Ewing family tumor (sarcoma), which often shows similar monomorphic basaloid cells and limited keratinization, together with expression of pancytokeratin, p40 and CD99 [16]. Assessment of the EWSR1 gene can help to corroborate this diagnosis, as recurrent EWSR1 translocations are described [16, 17]. Solid variant of adenoid cystic carcinoma is another important differential diagnosis, whereas the HPV-association and the lack of MYB/MYBL1 translocation in HMSC clearly distinguishes these two entities [2, 4, 18]. The exact cell of origin in HMSC is still not clear; however, the recurrent expression of SOX10 [15] and S-100 [2] as well as the often multiphasic expression of pancytokeratin and morphology suggest a potential salivary gland origin. However, SOX10 expression is also described in basaloid (squamous cell) carcinomas, being categorized as a subclass of squamous cell carcinoma [19]. LEF-1 staining was consistently expressed in our cases, in line with a previous report [20]. HPV RNA in situ hybridization, providing evidence of transcriptionally active HPV association, together with diffuse p16 expression corroborates a causative role of HPV in HMSC [2, 21]. To date, no data exist regarding the mechanisms of HPV infection in the sinonasal tract. Interestingly, we observed that three of our four patients were hospital employees with patient contact and all tumors were within the nasal cavity. Previous data demonstrated that HPV can be detected on the body surface (e.g. nostrils) of health care professionals after the treatment of genital warts [22]. However, the overall HPV detection rate of employees performing such procedures was not significantly higher than in employees, who did not perform these procedures [23]. One study reported the detection of HPV high-risk types in the aerosol of uterine cervix electrosurgical procedures in humans [24]. Surface HPV contamination on medical equipment has been reported in genitourinary clinics, but also on airport toilets [25–27]. However, the presence of HPV DNA alone does not prove infectivity [27]. Clearly, the observations from our small case series are insufficient to extrapolate a causal relationship. Nevertheless, the cluster of cases of HMSC in our cohort of nurses/nursing assistant justifies further epidemiological studies.
Conclusion
We describe four cases of HPV-related multiphenotypic sinonasal carcinoma, three of which occurred in the nasal cavity of nurses/nursing assistant. HPV type 82 has been added to the associated virus types, as well as a glomeruloid histological growth pattern and extensive mature keratinization. Due to the low case numbers, we cannot draw a conclusion regarding a potential occupational association, but these data warrant further epidemiological investigations.
Author Contributions
Study conception and design was established by Niels J. Rupp and Grégoire B. Morand. Material preparation and data collection were performed by Niels J. Rupp, Ulrike Camenisch, Kati Seidl, Elisabeth J. Rushing, Martina A. Broglie, David Holzmann and Grégoire B. Morand. David Holzmann was mainly responsible for patient care and surgery. Analyses were performed by Niels J. Rupp, Nanina Anderegg and Grégoire B. Morand. The first draft of the manuscript was written by Niels J. Rupp and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
No funding was obtained for this study.
Data Availability
Data available on request due to privacy/ethical restrictions.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Inform Consent
All patients gave written consent and the study was approved by the local ethics committee (Protocol number 2016–0162 incl. amendment of February 24th, 2018).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bishop JA, Westra WH. Human papillomavirus-related multiphenotypic sinonasal carcinoma: an emerging tumor type with a unique microscopic appearance and a paradoxical clinical behaviour. Oral Oncol. 2018;87:17–20. doi: 10.1016/j.oraloncology.2018.10.011. [DOI] [PubMed] [Google Scholar]
- 2.Bishop JA, Andreasen S, Hang JF, Bullock MJ, Chen TY, Franchi A, et al. HPV-related multiphenotypic sinonasal carcinoma: an expanded series of 49 cases of the tumor formerly known as HPV-related carcinoma with adenoid cystic carcinoma-like features. Am J Surg Pathol. 2017;41(12):1690–1701. doi: 10.1097/PAS.0000000000000944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vital D, Holzmann D, Huber GF, Soyka MB, Moch H, Zimmermann DR, et al. p16(INK4a): a surrogate marker of high-risk human papillomavirus infection in squamous cell carcinoma of the nasal vestibule. Head Neck. 2017;39(7):1392–1398. doi: 10.1002/hed.24767. [DOI] [PubMed] [Google Scholar]
- 4.Bishop JA, Ogawa T, Stelow EB, Moskaluk CA, Koch WM, Pai SI, et al. Human papillomavirus-related carcinoma with adenoid cystic-like features: a peculiar variant of head and neck cancer restricted to the sinonasal tract. Am J Surg Pathol. 2013;37(6):836–844. doi: 10.1097/PAS.0b013e31827b1cd6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andreasen S, Bishop JA, Hansen TV, Westra WH, Bilde A, von Buchwald C, et al. Human papillomavirus-related carcinoma with adenoid cystic-like features of the sinonasal tract: clinical and morphological characterization of six new cases. Histopathology. 2017;70(6):880–888. doi: 10.1111/his.13162. [DOI] [PubMed] [Google Scholar]
- 6.Hang JF, Hsieh MS, Li WY, Chen JY, Lin SY, Liu SH, et al. Human papillomavirus-related carcinoma with adenoid cystic-like features: a series of five cases expanding the pathological spectrum. Histopathology. 2017;71(6):887–896. doi: 10.1111/his.13301. [DOI] [PubMed] [Google Scholar]
- 7.Shah AA, Lamarre ED, Bishop JA. Human papillomavirus-related multiphenotypic sinonasal carcinoma: a case report documenting the potential for very late tumor recurrence. Head Neck Pathol. 2018;12(4):623–628. doi: 10.1007/s12105-018-0895-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahn B, Kim E, Oh H, Chae YS, Kim CH, Lee Y, et al. Human papillomavirus-related multiphenotypic sinonasal carcinoma with late recurrence. J Pathol Transl Med. 2019 doi: 10.4132/jptm.2019.04.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laeng RH, Altermatt HJ, Scheithauer BW, Zimmermann DR. Amyloidomas of the nervous system: a monoclonal B-cell disorder with monotypic amyloid light chain lambda amyloid production. Cancer. 1998;82(2):362–374. doi: 10.1002/(sici)1097-0142(19980115)82:2<375::aid-cncr18>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 10.Petersen I, Schewe C, Schluns K, Dietel M, Speich N, Schmitt C, et al. Inter-laboratory validation of PCR-based HPV detection in pathology specimens. Virchows Arch. 2007;451(3):701–716. doi: 10.1007/s00428-007-0437-0. [DOI] [PubMed] [Google Scholar]
- 11.Jacobs MV, de Roda Husman AM, van den Brule AJ, Snijders PJ, Meijer CJ, Walboomers JM. Group-specific differentiation between high- and low-risk human papillomavirus genotypes by general primer-mediated PCR and two cocktails of oligonucleotide probes. J Clin Microbiol. 1995;33(4):901–905. doi: 10.1128/JCM.33.4.901-905.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Swiss Federal Office for Statistics. Trend in the number of employed persons. 2014. https://www.bfs.admin.ch/bfs/en/home/statistics/work-income/employment-working-hours/employed-persons/trend-number-employed-persons.html.
- 13.Geraets D, Alemany L, Guimera N, de Sanjose S, de Koning M, Molijn A, et al. Detection of rare and possibly carcinogenic human papillomavirus genotypes as single infections in invasive cervical cancer. J Pathol. 2012;228(4):534–543. doi: 10.1002/path.4065. [DOI] [PubMed] [Google Scholar]
- 14.Edgar M, Caruso AM, Kim E, Foss RD. NUT midline carcinoma of the nasal cavity. Head Neck Pathol. 2017;11(3):389–392. doi: 10.1007/s12105-016-0763-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hsieh MS, Lee YH, Jin YT, Huang WC. Strong SOX10 expression in human papillomavirus-related multiphenotypic sinonasal carcinoma: report of 6 new cases validated by high-risk human papillomavirus mRNA in situ hybridization test. Hum Pathol. 2018;82:264–272. doi: 10.1016/j.humpath.2018.07.026. [DOI] [PubMed] [Google Scholar]
- 16.Bishop JA, Alaggio R, Zhang L, Seethala RR, Antonescu CR. Adamantinoma-like Ewing family tumors of the head and neck: a pitfall in the differential diagnosis of basaloid and myoepithelial carcinomas. Am J Surg Pathol. 2015;39(9):1267–1274. doi: 10.1097/PAS.0000000000000460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rooper LM, Jo VY, Antonescu CR, Nose V, Westra WH, Seethala RR, et al. Adamantinoma-like Ewing sarcoma of the salivary glands: a newly recognized mimicker of basaloid salivary carcinomas. Am J Surg Pathol. 2019;43(2):187–194. doi: 10.1097/PAS.0000000000001171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rettig EM, Tan M, Ling S, Yonescu R, Bishop JA, Fakhry C, et al. MYB rearrangement and clinicopathologic characteristics in head and neck adenoid cystic carcinoma. Laryngoscope. 2015;125(9):E292–E299. doi: 10.1002/lary.25356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rooper LM, McCuiston AM, Westra WH, Bishop JA. SOX10 immunoexpression in basaloid squamous cell carcinomas: a diagnostic pitfall for ruling out salivary differentiation. Head Neck Pathol. 2018 doi: 10.1007/s12105-018-0990-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shah AA, Oliai BR, Bishop JA. Consistent LEF-1 and MYB immunohistochemical expression in human papillomavirus-related multiphenotypic sinonasal carcinoma: a potential diagnostic pitfall. Head Neck Pathol. 2019;13(2):220–224. doi: 10.1007/s12105-018-0951-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Laco J, Sieglova K, Vosmikova H, Dundr P, Nemejcova K, Michalek J, et al. The presence of high-risk human papillomavirus (HPV) E6/E7 mRNA transcripts in a subset of sinonasal carcinomas is evidence of involvement of HPV in its etiopathogenesis. Virchows Arch. 2015;467(4):405–415. doi: 10.1007/s00428-015-1812-x. [DOI] [PubMed] [Google Scholar]
- 22.Bergbrant IM, Samuelsson L, Olofsson S, Jonassen F, Ricksten A. Polymerase chain reaction for monitoring human papillomavirus contamination of medical personnel during treatment of genital warts with CO2 laser and electrocoagulation. Acta Derm Venereol. 1994;74(5):393–395. doi: 10.2340/0001555574393395. [DOI] [PubMed] [Google Scholar]
- 23.Kofoed K, Norrbom C, Forslund O, Moller C, Froding LP, Pedersen AE, et al. Low prevalence of oral and nasal human papillomavirus in employees performing CO2-laser evaporation of genital warts or loop electrode excision procedure of cervical dysplasia. Acta Derm Venereol. 2015;95(2):173–176. doi: 10.2340/00015555-1912. [DOI] [PubMed] [Google Scholar]
- 24.Neumann K, Cavalar M, Rody A, Friemert L, Beyer DA. Is surgical plume developing during routine LEEPs contaminated with high-risk HPV? A pilot series of experiments. Arch Gynecol Obstet. 2018;297(2):421–424. doi: 10.1007/s00404-017-4615-2. [DOI] [PubMed] [Google Scholar]
- 25.Strauss S, Sastry P, Sonnex C, Edwards S, Gray J. Contamination of environmental surfaces by genital human papillomaviruses. Sex Transm Infect. 2002;78(2):135–138. doi: 10.1136/sti.78.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gallay C, Miranda E, Schaefer S, Catarino R, Jacot-Guillarmod M, Menoud PA, et al. Human papillomavirus (HPV) contamination of gynaecological equipment. Sex Transm Infect. 2016;92(1):19–23. doi: 10.1136/sextrans-2014-051977. [DOI] [PubMed] [Google Scholar]
- 27.Smelov V, Eklund C, Arroyo Muhr LS, Hultin E, Dillner J. Are human papillomavirus DNA prevalences providing high-flying estimates of infection? An international survey of HPV detection on environmental surfaces. Sex Transm Infect. 2013;89(8):627. doi: 10.1136/sextrans-2013-051280. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request due to privacy/ethical restrictions.