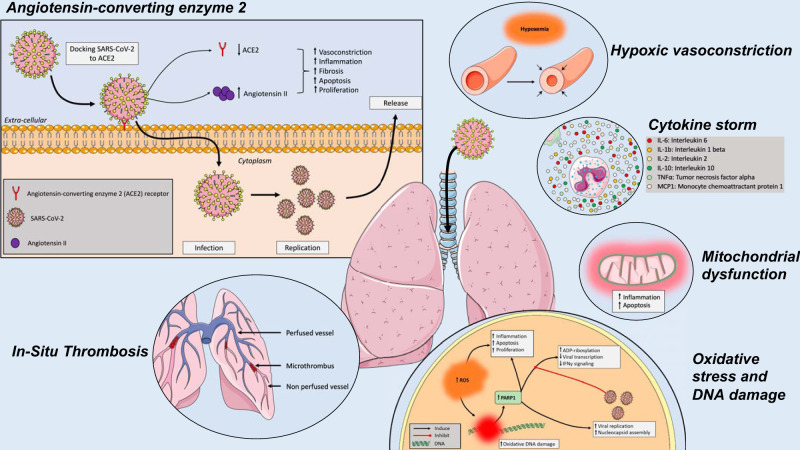
Fig. 1.
Effects of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) on the lungs and the pulmonary vasculature. SARS-CoV-2 cycle starts with the interaction with the angiotensin-converting enzyme 2 (ACE2) receptor from the host cells. Upon entry into the host cells, the viral RNA genome is then translated and proteins and RNA are packaged into progeny virions being released to infect more cells. The SARS-CoV-2-related disease (COVID-19) results in cytokine outburst, including IL-6, IL-1b, IL-2, IL-10, TNF-α, and monocyte chemoattractant protein-1 (MCP-1). Reactive oxygen species (ROS) are key signaling molecules that play an important role in the progression of inflammatory disorders, resulting in oxidative stress, mitochondrial dysfunction, and DNA damage. In addition to parenchymal abnormalities, disseminated intravascular coagulation, endothelial dysfunction, and impaired hypoxic pulmonary vasoconstriction ultimately generate pulmonary microthrombi, ventilation-perfusion mismatch, and hypoxemia.