Abstract
Background:
The use of transcatheter aortic valve replacement (TAVR) has grown rapidly. The purpose of this study was to assess whether hospital market competition was associated with the use of TAVR.
Methods:
We used 5 Healthcare Cost and Utilization Project state inpatient databases (Arizona, Florida, Iowa, Massachusetts, Washington) to identify patients undergoing TAVR (n=5,563) or surgical aortic valve replacement (n=30,672) across 154 hospitals from 2011 to 2014. Using the Herfindahl-Hirschman Index (HHI) to calculate market competition, hospitals were categorized into commonly used categories of low (HHI > 0.25), moderate (HHI 0.15-0.25), and high (HHI < 0.15) competition. We associated market competition category with TAVR utilization using hierarchical logistic regression, adjusting for patient characteristics, hospital characteristics, year, and hospital random effect. We modeled associations between HHI category and in-hospital mortality, admission length of stay, and discharge to home as secondary outcomes.
Results:
After adjustment, patients treated at high-competition hospitals had higher odds of receiving TAVR, relative to patients at low-competition hospitals (adjusted odds ratio [ORadj], 5.31; 95% confidence interval [CI]: 2.10-13.4). TAVR use increased each year (ORadj, 1.73; 95% CI, 1.38-2.17) but was similar across HHI categories. Competition was not associated with in-hospital mortality or length of stay. Patients at high-competition hospitals were more likely to be discharged home (ORadj, 2.39; 95% CI, 1.23-4.66) compared with patients at low-competition hospitals.
Conclusions:
Market competition was positively associated with a hospital’s adoption of TAVR. Future studies should further examine the impact of competition on quality and appropriateness.
Keywords: Aortic Valve, replacement, Health economics, Heart valve replacement, transapical, percutaneous, outcomes
Introduction
Transcatheter aortic valve replacement (TAVR) has rapidly evolved as a therapy for patients with severe aortic stenosis[1]. Originally indicated as an alternative to medical therapy for patients not suitable for surgical aortic valve replacement (SAVR) (2011), TAVR’s approved use has expanded to high (2012) and intermediate (2016) surgical risk populations[2–4]. Consequently, there has been a 7-fold increase in annual TAVR volume during this period, and continued expansion of the number of centers performing TAVR[5,6].
Evidence on the role of market competition in the adoption of TAVR is currently limited. On the one hand, adoption of TAVR is driven by unmet clinical need among patients at prohibitive risk for SAVR, the Food and Drug Administration’s expanding criteria for use, and patient preference for a less invasive procedure[7]. On the other hand, prior research suggests that market forces contribute significantly to the adoption of new surgical procedures and technologies[8–10]. Moreover, evidence has suggested that hospitals in more competitive markets provide higher quality care, but this has not been explored in the context of aortic valve replacement[11–13]. Understanding how the local market factors of hospitals have contributed to the adoption of TAVR, and whether or not they are associated with quality of care, may inform coverage determinations and best practices for the treatment of severe aortic stenosis.
Utilizing a retrospective cohort study, we sought to estimate the independent association between hospital market competition and use of TAVR in patients undergoing aortic valve replacement. We hypothesized that patients treated in hospitals located in high-competition markets would be more likely to receive TAVR vs SAVR compared with patients treated in low-competition market hospitals, independent of patient and hospital characteristics. As a secondary analysis, we explored the association between hospital market competition and measures of surgical quality of care - including in-hospital mortality, admission length of stay (LOS), and discharge to home.
Patients and Methods
This study was reviewed by the University of Michigan Institutional Review Board and deemed to be exempt from institutional review board approval (HUM00134771).
Patient Population
For this retrospective cohort study, we used State Inpatient Databases for Arizona, Florida, Iowa, Massachusetts, and Washington to identify patients undergoing TAVR or SAVR from January 1, 2011 to December 31, 2014[14]. International Classification of Diseases (ICD)-9-Clinical Modification procedure codes were employed to identify 5,563 TAVR admissions (35.05, 35.06) and 38,540 SAVR admissions (35.21, 35.22). Unique TAVR-specific ICD-9 codes were not implemented until the third quarter of 2011, and thus we excluded 7,868 admissions from our cohort among patients undergoing aortic valve replacement before October 2011. Our final sample included 5,563 TAVR and 30,672 SAVR admissions for a total of 36,235 admissions for both procedures (Supplemental Figure 1). We linked State Inpatient Database files with data from the Hospital Market Structure (2009), and American Hospital Association (2011) linkage files, which provide additional information concerning hospital market competition and hospital-level characteristics, respectively.
Measures
The primary outcome for this analysis was whether a patient received TAVR vs SAVR during their admission. Our secondary outcomes included in-hospital mortality, hospital LOS (in days), and discharge to home (vs not to home) as proxies of quality of care.
Our primary exposure was hospital market competition. We used the Herfindahl-Hirschman Index (HHI) to estimate competition at the hospital level[15,16]. This index has been widely used as a measure of competition in medical research[8–10]. The HHI is calculated as the sum of the squared market shares of the hospitals in a given market. For instance, in a market with two hospitals that treat 75% and 25% of the patients in that region, respectively, the HHI for those hospitals is = 0.752 + 0.252 = 0.5625 + 0.0625 = 0.625. A market consisting of 10 hospitals who each treat 10% of the patients in that region will have an HHI = (0.102) * 10 = 0.10. An HHI of 0 represents an extremely competitive market consisting of many, small hospitals, whereas an HHI of 1 indicates a low competition, or highly concentrated market, in which there is a monopoly. Consistent with prior literature, we elected to use a variable radius to define markets[8]. This method assigns a market area to each hospital based on the distance required to capture a specified percentage of its discharges. We selected a 75% variable radius (the radius required to capture 75% of a hospital’s discharges) for our calculation of the HHI. We categorized hospitals into different levels of competition: HHI less than 0.15 was classified as a high-competition market, HHI between 0.15 and 0.25 was classified as a moderate-competition market, and HHI greater than 0.25 was classified as a low-competition market. To ensure our findings were robust to different market definitions, we also defined HHI using other measures available in the Healthcare Cost and Utilization Project Hospital Market Structure data source, including using variable radii, fixed radii, core-based statistical areas, and health service areas[17].
Statistical Methods
We compared patient-level and hospital-level characteristics of the cohort by TAVR vs SAVR status. Chi-square and student’s t tests were used to assess univariate associations for categorical and continuous characteristics, respectively. Patient-level characteristics assessed included age, sex, race, admission status, admission source, and Elixhauser comorbidities[18]. Hospital-level characteristics examined included bed size, teaching status, ownership structure, whether the hospital belongs to a health system, urban status, and safety net status.
Next, we plotted hospital-level HHI against hospital TAVR proportion to illustrate the overall association between hospital-level market competition and TAVR utilization. We estimated the Pearson correlation coefficient between hospital HHI and TAVR proportion to assess the strength of the correlation. We also estimated the Pearson correlation coefficient between hospital HHI and overall aortic volume (TAVR+SAVR) to understand the relationship between market competition and procedural volume.
We then estimated the TAVR proportion (TAVR divided by TAVR+SAVR) by HHI category (low, moderate, and high), and used hierarchical logistic regression models to estimate the relative odds of TAVR (vs. SAVR) in high-competition and moderate-competition hospitals compared to low-competition hospitals. We assessed 3 models: (1) an unadjusted model, (2) a model adjusted for patient characteristics, and (3) a model adjusted for both patient-level and hospital-level characteristics. All models included a hospital random intercept to account for hospital-level clustering. We also estimated the interaction term between time (defined as year and quarter in separate analyses) and HHI category to assess whether trends in TAVR use were different by HHI category. We report the estimate, standard error, and p-value for these interaction terms. As a sensitivity analysis, the effect of HHI on TAVR utilization was assessed using alternative market definitions (core-based statistical areas, health service areas, and fixed radius).
For our secondary objective, we estimated the association between HHI category and quality of care measures available in Healthcare Cost and Utilization Project, including in-hospital mortality, hospital LOS (in days), and discharge to home vs. not to home. We performed this analysis for TAVR and SAVR patients together adjusting for procedure type, patient and hospital characteristics, and hospital random intercept. We also performed this analysis for TAVR and SAVR patients separately, adjusting for patient and hospital characteristics and hospital random intercept.
All analyses were performed with SAS version 9.4 (SAS Institute, Cary, NC).
Results
The primary outcome of TAVR utilization occurred in 5,563 of 36,235 (15.4%) patients undergoing either SAVR or TAVR. At the hospital level, the mean proportion of patients receiving TAVR was 8.2% ± 12.3%. The distribution of patient and hospital-level factors by TAVR vs SAVR status can be found in Table 1.
Table 1.
Study cohort characteristics.
| Characteristics | Overall | SAVR ( % or mean, SD) | TAVR (n, % or mean, SD) | p-value |
|---|---|---|---|---|
| N = 44,103 | n = 38,540, 84.6% | n = 5,563, 15.4% | ||
| Patient-level | ||||
| Age (years) | 71.0, 13.7 | 69.1, 13.5 | 81.6, 9.3 | <0.01 |
| Female Sex | 37.2 | 35.5 | 46.2 | <0.01 |
| Non-white race | 13.0 | 13.5 | 9.9 | <0.01 |
| Elective Case | 72.7 | 71.3 | 80.1 | <0.01 |
| Admitted from Home | 54.3 | 54.1 | 55.2 | <0.01 |
| Elixhauser Comorbidities, # | 4.04, 2.01 | 3.92, 2.0 | 4.73, 1.95 | <0.01 |
| Paralysis | 1.72 | 1.64 | 2.21 | <0.01 |
| Chronic Lung Disease | 23.8 | 21.7 | 35.2 | <0.01 |
| Coagulopathy | 30.6 | 31.8 | 24.2 | <0.01 |
| CHF | 39.0 | 33.3 | 70.6 | <0.01 |
| Deficiency Anemia | 20.9 | 20.1 | 25.3 | <0.01 |
| Depression | 7.2 | 7.3 | 7.1 | 0.71 |
| Diabetes Mellitus | 30.3 | 29.8 | 33.7 | <0.01 |
| Fluid and Electrolyte Disorders | 35.0 | 36.3 | 27.8 | <0.01 |
| Hypertension | 75.3 | 74.5 | 80.1 | <0.01 |
| Hypothyroidism | 14.4 | 13.2 | 20.8 | <0.01 |
| Neurological Disorders (other than paralysis) | 5.16 | 4.91 | 6.58 | <0.01 |
| Obesity | 18.7 | 19.6 | 13.5 | <0.01 |
| Peripheral Vascular Disease | 22.3 | 20.4 | 32.9 | <0.01 |
| Pulmonary circulatory disease | 15.5 | 14.1 | 22.8 | <0.01 |
| Renal failure | 18.3 | 15.6 | 33.2 | <0.01 |
| Valvular disease | 26.4 | 28.3 | 16.1 | <0.01 |
| Hospital-level | ||||
| Teaching hospital | <0.01 | |||
| Major teaching hospital | 35.3 | 39.1 | 13.4 | |
| Minor teaching hospital | 26.1 | 24.5 | 35.0 | |
| Non-teaching hospital | 38.6 | 36.4 | 51.0 | |
| Member of Health System | 73.7 | 73.6 | 74.4 | 0.20 |
| Urban Setting | 99.6 | 99.6 | 99.9 | <0.01 |
| Ownership status | <0.01 | |||
| Public | 9.55 | 8.58 | 14.9 | |
| Not-for-profit | 77.3 | 77.1 | 78.4 | |
| For-profit | 13.1 | 14.3 | 6.72 | |
| Bed count < 300 | 23.27 | 25.6 | 10.4 | <0.01 |
| Safety Net Hospital | 28.0 | 24.9 | 44.9 | <0.01 |
| HHI | ||||
| 75% variable radius (continuous) | 0.306 (0.266) | 0.323 (0.272) | 0.215 (0.207) | <0.01 |
| 75% variable radius (categorical) | <0.01 | |||
| High Competition | 36.0 | 32.6 | 54.8 | |
| Moderate Competition | 16.9 | 17.8 | 12.1 | |
| Low Competition | 46.9 | 49.4 | 33.1 | |
| Clinical Outcomes | ||||
| In-hospital mortality | 3.29 | 3.09 | 4.39 | <0.01 |
| Length of stay | 9.73 | 10.0 | 8.02 | <0.01 |
| Discharge to home | 27.5 | 27.3 | 28.5 | <0.01 |
The mean, patient-level HHI in our study cohort was 0.306 ± 0.266. Patients undergoing TAVR had a significantly lower mean HHI relative to SAVR (0.215 vs 0.323; p < 0.01). TAVR utilization differed significantly by HHI category (p < 0.01). The unadjusted relationship between hospital HHI and proportion of patients undergoing TAVR is presented in Figure 1; as HHI increases, the proportion of patients receiving TAVR decreases (Pearson correlation coefficient r= −0.28, p<0.01). HHI is also significantly associated with a hospital’s volume of aortic procedures (TAVR + SAVR); as HHI increases, the volume of patients receiving TAVR or SAVR decreases (Spearman correlation coefficient r = −0.17, p = 0.03). The distribution of HHI using alternative market definitions by TAVR status can be found in Supplemental Table 1.
Figure 1.
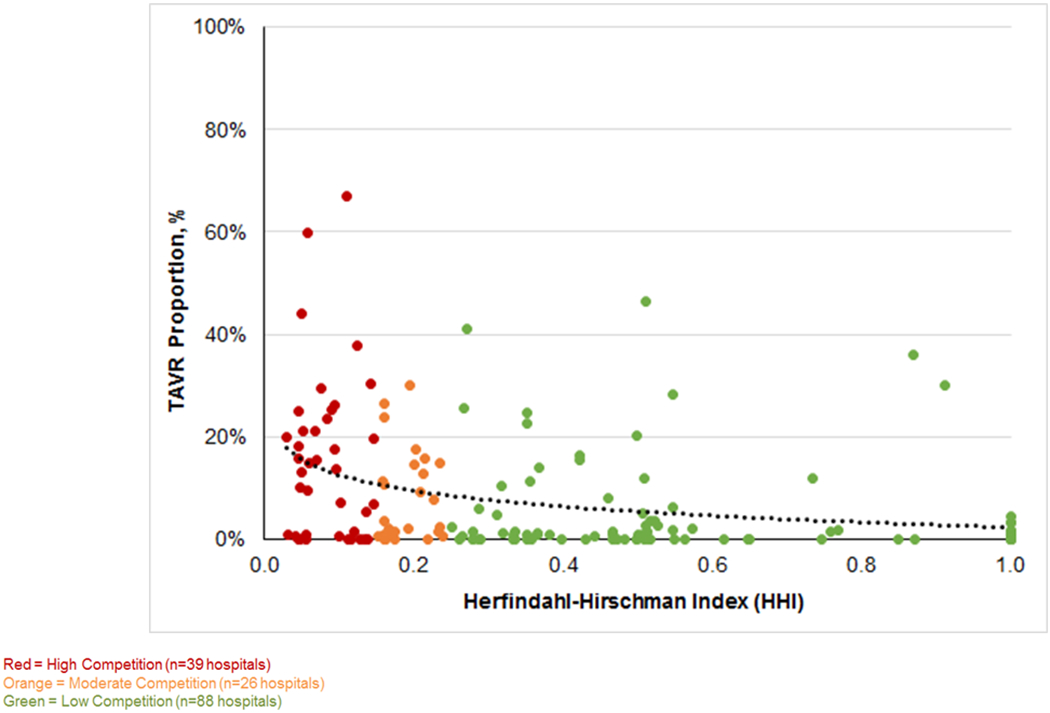
Scatterplot of hospital HHI and % TAVR.
Results of the hierarchical logistic regression models for the association between HHI category and TAVR vs SAVR utilization are presented in Table 2. Before adjustment, high (odds ratio [OR], 6.30; 95% confidence interval [CI], 3.68-10.8) and moderate market competition (OR, 2.27; 95% CI, 1.21-4.26) were significantly associated with increased TAVR utilization, relative to low-competition HHI. This association persisted after adjustment for patient-level factors. After adjustment for both patient-level and hospital-level factors in the final model, a significant association was observed among patients treated at high-competition vs low-competition centers (adjusted OR, 5.31; 95% CI 2.10-13.4, p < 0.01), but not those treated at moderate-competition centers. The unadjusted and adjusted ORs for all covariates in the final model are reported in Supplemental Table 2. When HHI was calculated using core-based statistical areas, a 15-mile fixed radius, or 90% variable radius market definition, our results were qualitatively unchanged (Supplemental Table 3).
Table 2.
Association of HHI with odds of TAVR.
| Model | Proportion of patients receiving TAVR | OR (CIs) | p-value |
|---|---|---|---|
| HHI, Unadjusted | |||
| High Competition | 23.4% (3048/13037) | 6.30 (3.68-10.8) | <0.01 |
| Moderate Competition | 11.0% (672/6136) | 2.27 (1.21-4.26) | <0.01 |
| Low Competition | 10.8% (1840/16985) | Ref | Ref |
| HHI, Adjusted for patient-level factorsa | |||
| High Competition | 23.4% (3048/13037) | 11.5 (6.09-21.6) | <0.01 |
| Moderate Competition | 11.0% (672/6136) | 2.91 (1.51-5.60) | <0.01 |
| Low Competition | 10.8% (1840/16985) | Ref | Ref |
| HHI, Adjusted for patient-, and hospital-level factorsb | |||
| High Competition | 23.4% (3048/13037) | 5.31 (2.10-13.4) | <0.01 |
| Moderate Competition | 11.0% (672/6136) | 1.82 (0.79-4.22) | 0.16 |
| Low Competition | 10.8% (1840/16985) | Ref | Ref |
Adjusted for: Year of procedure, sex, race, procedure status, admission from home paralysis, chronic lung disease, coagulation deficiency, congestive heart failure, deficiency anemias, depression, diabetes, electrolyte disorders, hypertension, hypothyroidism, neurologic disorders (not including paralysis), obesity, peripheral vascular disease, pulmonary circulatory disease, renal failure, valvular disease
Adjusted for patient-level factors, as well as for teaching hospital status, ownership status, bed size, and safety net status
When examining trends over time, we found that TAVR utilization was significantly associated with year of procedure, both overall and by HHI category (Figure 2) (all p-values < 0.01). The effect of time on TAVR utilization did not differ by HHI category, as demonstrated by the nonsignificant interaction terms reported in Supplemental Table 4.
Figure 2.
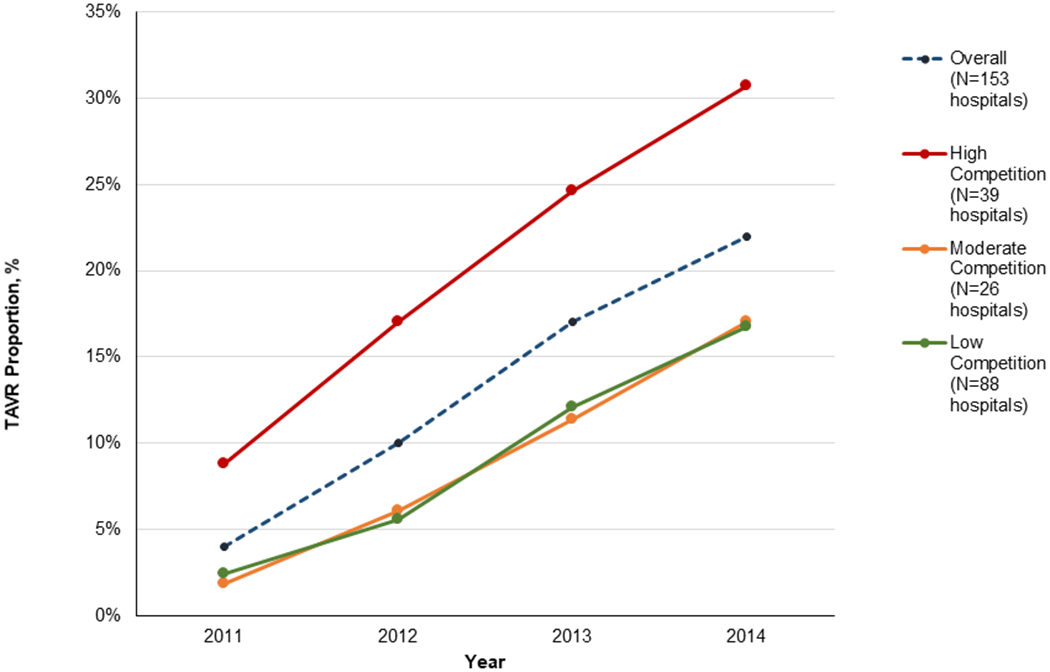
Proportion of TAVR by HHI category.
Finally, we found no association between market competition and in-hospital mortality or hospital LOS in either the combined TAVR + SAVR cohort or the procedure-specific cohorts (Table 3). Within the combined TAVR + SAVR cohort, patients treated at high-competition hospitals had higher 2.39 higher odds of being discharged to home, relative to patients treated at low-competition hospitals (p < 0.01). A significant association between high competition and discharge to home was also observed among the SAVR-only cohort (adjusted OR, 2.27; 95% CI, 1.15-4.50). This effect was not significant in the TAVR-only cohort.
Table 3.
Clinical outcomes for TAVR and SAVR by HHI categorya
| In-hospital mortality | Hospital LOS (days) | Discharge to Home | |||||
|---|---|---|---|---|---|---|---|
| Patient Population | Market Competition | N (%) | OR (95% CI) | Mean (SD) | Diff (95% CI) | N (%) | OR (95% CI) |
| TAVR and SAVR | High | 398 (3.05) | 0.95 (0.79-1.30) | 9.89 (9.02) | 0.020 (−0.74, 0.79) | 3923 (30.1) | 2.39 (1.23-4.66) |
| Moderate | 232 (3.78) | 1.12 (0.85-1.48) | 9.72 (8.81) | −0.31 (−1.00,0.38) | 1876 (30.6) | 1.38 (0.75-2.54) | |
| Low | 556 (3.27) | ref | 9.62 (7.91) | ref | 4134 (24.34) | ref | |
| TAVR | |||||||
| High | 135(4.43) | 1.15 (0.69-1.91) | 8.17 (6.65) | −0.20 (−1.33, 0.93) | 943 (30.9) | 2.18 (0.93-5.11) | |
| Moderate | 37 (5.51) | 1.40 (0.85-2.33) | 8.76 (8.81) | 0.66 (−0.43, 1.76) | 161 (24.0) | 0.92 (0.41-2.06) | |
| Low | 71 (3.86) | ref | 7.50 (6.64) | ref | 478 (26.0) | ref | |
| SAVR | |||||||
| High | 263 (2.63) | 0.92 (0.66-1.29) | 10.4 (9.6) | 0.16 (−0.62, 0.95) | 2980 (29.83) | 2.27 (1.15-4.50) | |
| Moderate | 195 (3.57) | 1.11 (0.83-1.47) | 9.84 (8.8) | −0.39 (−1.10,0.31) | 1715 (31.4) | 1.44 (0.77-2.68) | |
| Low | 485 (3.20) | ref | 9.88 (8.01) | ref | 3656 (24.1) | ref | |
Results of multi-level generalized linear mixed modeling, adjusting for patient- and hospital-level factors, as well as time. Hospital modeled as random effect.
Comment
The primary objective of this study was to assess the relationship between hospital market competition and TAVR utilization among patients undergoing aortic valve replacement. We found a significant, positive association between increasing hospital market competition and TAVR utilization, independent of patient and hospital characteristics. Patients treated at hospitals in high-competition markets had 5 times higher odds of undergoing TAVR, relative to patients treated in low-competition markets. Additionally, we observed that while TAVR utilization was significantly associated with time, trends in TAVR use over time did not differ by HHI category. Finally, we found that TAVR and SAVR quality of care was largely similar across hospital market competition categories.
We recognize the limitations of the present study. First, our cohort was derived from inpatient administrative data, which lacks clinical detail necessary for rigorous risk adjustment. Replication of these analyses in a clinical database, such as the Society of Thoracic Surgeons/American College of Cardiology’s Transcatheter Valve Therapy registry, would provide more clinically-relevant patient characteristics to include in risk-adjustment. However, we used established methods to identify major comorbidities within claims data and adjusted for these as well as demographic and hospital-level factors in our modeling[18]. Second, we acknowledge that HHI may misidentify market competition for some hospitals. We undertook sensitivity analyses utilizing alternative definitions of market competition to assess the robustness of our findings. Third, HHI is calculated at the hospital-level and is not a cardiac service line-specific measure of competition. However, hospital-level HHI is routinely utilized for similar procedure-specific analyses and is an appropriate approximation of competition at the cardiac surgical service line level[8–10]. Fourth, our study period is limited to the first 3 years after TAVR approval in the United States and may not completely reflect current clinical and market conditions. We observed that the effect of competition on TAVR utilization was stable over time, suggesting that this remains an important determinant of this technology’s dissemination. Last, our findings may not be generalizable outside of the 5 states included in the study. Nevertheless, the states included are geographically diverse, and we adjusted for demographic and hospital-level characteristics, which may vary by state.
Market competition has frequently been shown to be an important factor influencing the utilization of novel cardiovascular therapies. In 1983, Robinson and colleagues[9] found that hospitals in markets with more than 20 competing centers were 166% more likely to offer coronary angioplasty and 147% more likely to offer bypass surgery than hospitals with no competitors in their market. In 2003, Karaca-Mandic and colleagues[10] demonstrated that patients undergoing percutaneous coronary intervention in cardiology practice markets falling within the fourth quartile of HHI (lowest competition) were significantly less likely to receive drug-eluting stents, relative to those in first HHI quartile. These patterns are also consistent among other novel surgical technologies - the use of robotic-assisted surgery in patients undergoing radical prostatectomy, total nephrectomy, partial nephrectomy, hysterectomy, or oophorectomy was more frequent in hospitals located in more competitive markets[8]. Our findings add to this literature by suggesting that, over and above the factors we adjust for, hospitals located in competitive markets are more likely to utilize TAVR vs SAVR.
We also found that market competition was not significantly associated with quality of care in our cohort, as measured by in-hospital mortality or hospital LOS. These findings are in contrast to most existing literature, which suggests that market competition is positively associated with quality of care. In a study of Medicare beneficiaries admitted with a primary diagnosis of acute myocardial infarction (AMI) from 1985 to 1994, Kessler and McClellan[11] reported that risk-adjusted mortality was significantly higher for patients treated in less competitive markets. The authors built upon this finding in 2005 by demonstrating that among high-risk AMI patients (defined as those patients with a previous hospitalization for AMI in the past year), decreased market competition was associated with significantly worse outcomes - patients in the upper quartile of HHI (low competition) had 0.82% higher 1-year mortality than those in the bottom quartile of HHI (high competition)[12]. However, Gowrisankaran and Town[13] found that while mortality was significantly lower for health maintenance organization patients treated for AMI at high-competition centers, mortality was significantly higher for Medicare patients treated at the same high-competition centers. It is worthwhile to note that while we assessed short-term outcomes, these studies assessed long-term outcomes (ie, in-hospital vs. 1-year mortality) - it is possible that competition’s effect on quality differs over time. Ultimately, further study of the effect market competition has on quality of care in TAVR and SAVR is warranted.
It remains unclear, however, whether the additional growth in TAVR observed among high-competition centers relative to medium-competition and low-competition centers has occurred at the expense of clinical appropriateness. Historically, intense competition for case volume by hospitals has been suggested as a driver of less appropriate use of healthcare resources. The certificate of need (CON) program, which seeks to limit the number of hospitals providing particular services in a state, offers a unique window into how policy efforts to influence competition may impact utilization. Ross and colleagues[19] compared appropriateness of cardiac catheterization in states with and without CON regulation and found that CON regulation was significantly associated with lower rates of catheterization in patients with weak or equivocal indications. It is likely that the United States’ initial experience with TAVR was influenced by hospital market competition to a lesser degree, with early adoption of the technology largely limited to tertiary care hospitals. However, the number of sites performing TAVR has since expanded and the results of the PARTNER (Placement of Aortic Transcatheter Valve Trial) 3 and Evolut low-risk trials suggest that centers wishing to care for patients with aortic stenosis will increasingly desire to offer TAVR as a therapeutic option[20–21]. This increase in supply of TAVR, coupled with the increase in demand for TAVR secondary to our aging population and approval decisions by the Centers for Medicare and Medicaid Services, suggests that hospital market competition’s influence on TAVR utilization is likely to be as important if not greater in the future. As TAVR continues to mature as a therapeutic option for patients with severe aortic stenosis, it will be critical to explore options to ensure that its use is clinically appropriate.
In summary, we report a significant, positive association between increasing market competition and TAVR utilization among patients undergoing TAVR or SAVR in a large, multistate inpatient administrative database. Future studies should examine the impact of competition on quality of care and appropriateness among patients undergoing aortic valve replacement.
Supplementary Material
Acknowledgments
Disclosures
Raymond Strobel was supported by Michigan Institute for Clinical and Health Research, University of Michigan (Ann Arbor, MI) TL1 Grant (TL1TR002242). Dr Likosky received extra-mural support from the Agency for Healthcare Research and Quality (R01HS026003), U.S. Department of Health and Human Services. Dr Brescia was supported by the National Research Service Award postdoctoral fellowship (5T32HL076123). The opinions expressed in this document are those of the authors and do not reflect the official position of the Agency for Healthcare Research and Quality or the U.S. Department of Health and Human Services.
Footnotes
Meeting Presentation: This work was presented as an oral presentation at the Society of Thoracic Surgeons 55th Annual Meeting on January 27-29th, in San Diego, CA.
References
- [1].Cribier A The development of transcatheter aortic valve replacement (TAVR). Glob Cardiol Sci Pract 2016;2016:e201632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Leon MB, Smith CR, Mack M, Miller DC, Moses JW, Svensson LG, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med 2010;363:1597–607. [DOI] [PubMed] [Google Scholar]
- [3].Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW, Svensson LG, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med 2011;364:2187–98. [DOI] [PubMed] [Google Scholar]
- [4].Leon MB, Smith CR, Mack MJ, Makkar RR, Svensson LG, Kodali SK, et al. Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. N Engl J Med 2016;374:1609–20. [DOI] [PubMed] [Google Scholar]
- [5].Grover FL, Vemulapalli S, Carroll JD, Edwards FH, Mack MJ, Thourani VH, et al. 2016 Annual Report of The Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry. J Am Coll Cardiol 2017;69:1215–30. [DOI] [PubMed] [Google Scholar]
- [6].Messenger JC. Trends in United States TAVR Practice. Cardiac Interventions Today Mar-Apr 2018;12:46–50. [Google Scholar]
- [7].Wilson CB. Adoption of new surgical technology. BMJ 2006;332:112–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Wright JD, Tergas AI, Hou JY, Burke WM, Chen L, Hu JC, et al. Effect of Regional Hospital Competition and Hospital Financial Status on the Use of Robotic-Assisted Surgery. JAMA Surg 2016;151:612–20. [DOI] [PubMed] [Google Scholar]
- [9].Robinson JC, Garnick DW, McPhee SJ. Market and regulatory influences on the availability of coronary angioplasty and bypass surgery in U.S. hospitals. N Engl J Med 1987;317:85–90. [DOI] [PubMed] [Google Scholar]
- [10].Karaca-Mandic P, Town RJ, Wilcock A. The Effect of Physician and Hospital Market Structure on Medical Technology Diffusion. Health Serv Res 2017;52:579–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Kessler DP, McClellan MB. Is Hospital Competition Socially Wasteful? Q J Econ 2000;115:577–615. [Google Scholar]
- [12].Kessler D, Geppert J. The Effects of Competition on Variation in the Quality and Cost of Medical Care. Cambridge, MA: National Bureau of Economic Research; 2005. doi: 10.3386/w11226. [DOI] [Google Scholar]
- [13].Gozvrisankaran G, Town RJ. Competition, payers, and hospital quality. Health Serv Res 2003;38:1403–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Agency for Healthcare Research and Quality. HCUP Home. Healthcare Cost and Utilization Project (HCUP) n.d. https://www.hcup-us.ahrq.gov/home.jsp (accessed January 22, 2019). [PubMed]
- [15].Herfindahl OC. Concentration in the steel industry. Columbia University; New York, 1950. [Google Scholar]
- [16].Hirschman AO. National Power and the Structure of Foreign Trade. University of California Press; 1980. [Google Scholar]
- [17].Baker LC. Measuring competition in health care markets. Health Serv Res 2001;36:223–51. [PMC free article] [PubMed] [Google Scholar]
- [18].Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care 1998;36:8–27. [DOI] [PubMed] [Google Scholar]
- [19].Ross JS, Ho V, Wang Y, Cha SS, Epstein AJ, Masoudi FA, et al. Certificate of need regulation and cardiac catheterization appropriateness after acute myocardial infarction. Circulation 2007;115:1012–9. [DOI] [PubMed] [Google Scholar]
- [20].Mack Michael J., Leon Martin B., Thourani Vinod H., Makkar Raj, Kodali Susheel K., Russo Mark, Kapadia Samir R., et al. 2019. “Transcatheter Aortic-Valve Replacement with a Balloon-Expandable Valve in Low-Risk Patients.” The New England Journal of Medicine, March 10.1056/NEJMoa1814052. [DOI] [Google Scholar]
- [21].Popma Jeffrey J., Deeb G. Michael, Yakubov Steven J., Mumtaz Mubashir, Gada Hemal, O’Hair Daniel, Bajwa Tanvir, et al. 2019. “Transcatheter Aortic-Valve Replacement with a Self-Expanding Valve in Low-Risk Patients.” The New England Journal of Medicine, March 10.1056/NEJMoa1816885. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


