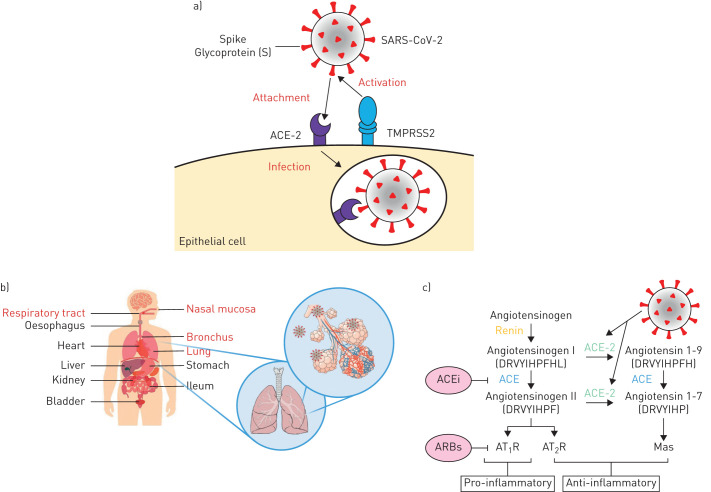
FIGURE 1.
Schematic representation of a) severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) binding to the angiotensin-converting enzyme 2 (ACE-2) receptor following activation of the spike protein (s) by transmembrane serine protease 2 (TMPRSS2), which leads to endocytosis and infection. b) Human organs that have been reported by Zou et al. [105] to show ACE2 expression, with the respiratory system highlighted in red. c) The renin–angiotensin system (RAS) and the proposed SARS-CoV-2 action. The generation of angiotensin II from angiotensin I by angiotensin-converting enzyme (ACE) induces vasoconstriction of blood vessels and pro-inflammatory effects through the binding of angiotensin II receptor type 1 (AT1R), while the receptor type 2 (AT2R) may negatively regulate this pathway. ACE inhibitors (ACEi) and angiotensin II receptor blockers (ARBs) are very successful anti-hypertensives by promoting vasodilation of blood vessels. ACE-2 inhibits the activity of angiotensin II by converting angiotensin I to angiotensin 1–9 and angiotensin II to angiotensin 1–7, which binds to the MAS1 proto-oncogene (Mas) receptor with anti-inflammatory effects. Upon SARS-CoV-2 binding to ACE-2, there is a shift in the ACE/ACE-2 balance towards a predominance of ACE, resulting in increased pro-inflammatory effects and tissue damage.