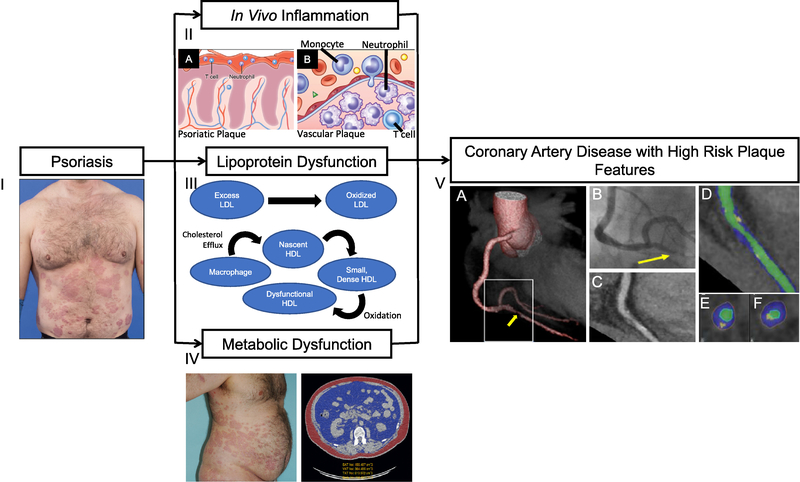
Figure 1:
Psoriasis is a chronic inflammatory skin disease associated with cardiometabolic disease. (I) Psoriasis patients may develop thick, extensive cutaneous plaques. (II) Psoriasis exhibits infiltration of T cells and neutrophils in (A) the cutaneous plaque as well as high systemic inflammation where the (B) vessel wall is infiltrated through a complex interplay of pro-inflammatory cellular components including T cells, monocytes, and neutrophils, leading to atherosclerotic cardiovascular disease. (III) Psoriasis associates with abnormal lipid profile and impaired HDL function, which in combination with residual inflammatory stress accelerates the formation of oxidation-modified lipoproteins, such as oxidized LDL and oxidized HDL. (IV) Transverse computed tomography (CT) images of an obese patient with psoriasis at the level of the abdominal aorta depicting high visceral adiposity (blue) in comparison with subcutaneous adiposity (red). Psoriasis and concomitant cardiometabolic disease are associated with high body mass index and waist-to-hip ratio. (V) CT 3D reconstruction model of a heart (A) depicting critical stenosis (B) due to a high-risk plaque, which was subsequently found to be a culprit for an ST-elevation myocardial infarction during follow-up. (C) Planar reconstruction of vessel demonstrating high-risk plaque. (D) Color-coded, curved multiplanar reconstruction (green, vessel lumen; blue, non-calcified plaque component; yellow, calcified plaque component). (E) and (F) Cross-sectional images. The plaque is only partially calcified, showing spotty calcification and some positive remodeling.