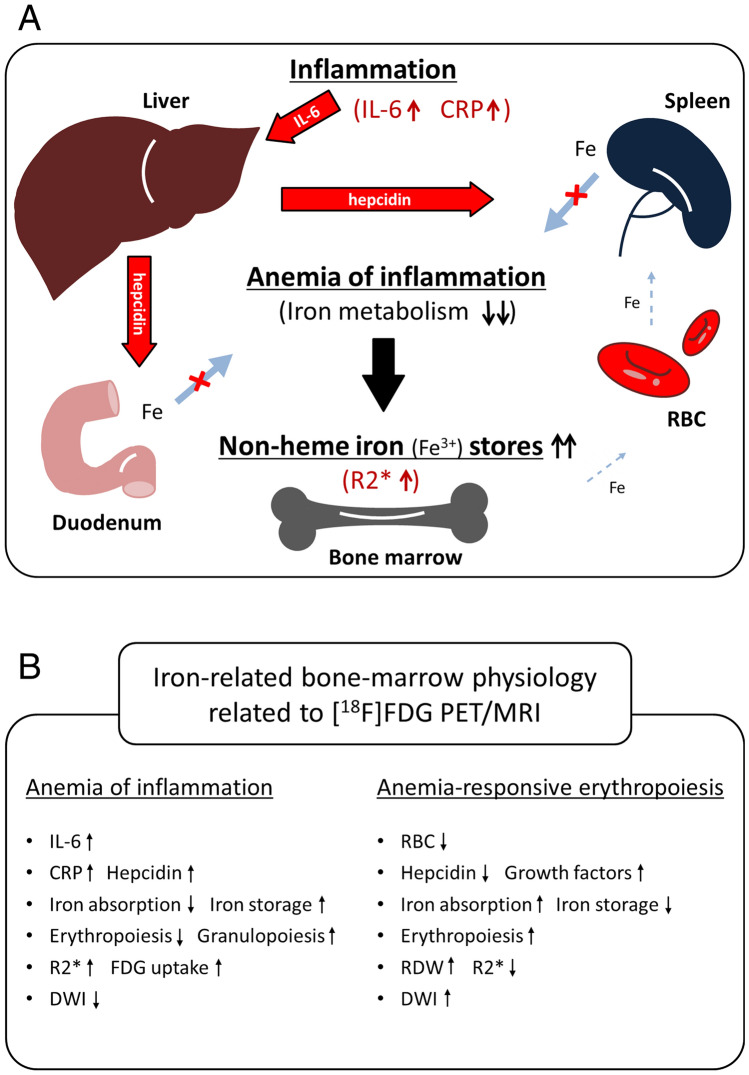
Figure 6.
A Assumed relationship between bone-marrow R2* and CRP. Under inflammatory conditions, inflammatory cytokines, such as interleukin 6 (IL-6), induce excess synthesis of CRP and the iron-regulatory hormone hepcidin secreted by hepatocytes, which inhibits iron entry into plasma by binding to and inactivating the iron exporter ferroportin in target cells such as duodenal enterocytes and tissue macrophages. These conditions lead to inadequate erythrocyte production in the setting of low serum iron despite preserved or even increased macrophage iron stores in the bone marrow: anemia of inflammation. Stored iron exists in a state of non-heme Fe3+, such as ferritin and hemosiderin, which shortens the T2* relaxation time, resulting in an increased R2* relaxation rate. B Comparison of two distinct types of iron-related bone-marrow physiology related to [18F]FDG PET/MRI. In the setting of anemia of inflammation, inflammatory cytokines and hepcidin suppress iron absorption and erythropoiesis, and increase non-heme iron storage in the marrow, resulting in high R2* relaxation rates and decreased bone-marrow signals on DWI. Stimulated granulopoiesis in the marrow induces an increased [18F]FDG uptake. On the other hand, in a state of anemia-responsive erythropoiesis, iron metabolism and erythropoiesis (RDW) are increased, and iron storage (R2*) is decreased by hepcidin insufficiency, leading to an increase in bone-marrow DWI signals.