Abstract
Apparent treatment-resistant hypertension (aTRH) is associated with adverse cardiovascular outcomes. aTRH is common and disproportionately affects African Americans. The objective of this study is to explore psychosocial correlates of aTRH in a population-based cohort of African Americans with hypertension. The sample included 1392 participants in the Jackson Heart Study with treated hypertension who reported being adherent to their antihypertensive medications. aTRH was defined as uncontrolled clinic BP (⩾140/90 mm Hg) with ⩾ 3 classes of antihypertensive medication or treatment with ⩾ 4 classes of antihypertensive medication, including a diuretic. Self-reported medication adherence was defined as taking all prescribed antihypertensive medication in the 24 h before the study visit. The association of psychosocial factors (chronic stress, depressive symptoms, perceived social support and social network) with aTRH was evaluated using Poisson regression with progressive adjustment for demographic, clinical and behavioural factors. The prevalence of aTRH was 15.1% (n = 210). Participants with aTRH had lower social network scores (that is, fewer sources of regular social contact) compared with participants without aTRH (P<0.01). No other psychosocial factors differed between groups. Social network was also the only psychosocial factor that was associated with aTRH prevalence in regression analyses. In age-, sex-adjusted and fully adjusted models, one additional unique source of social contact was associated with a 19% (PR = 0.81; 95% confidence interval (CI): 0.68–0.94, P = 0.001) and a 13% (PR = 0.87; 95% CI 0.74–1.0, P = 0.041) lower prevalence of aTRH, respectively. Social network was independently associated with aTRH and warrants further investigation as a potentially modifiable determinant of aTRH in African Americans.
INTRODUCTION
Apparent treatment-resistant hypertension (aTRH) is defined as clinic blood pressure (BP) that remains uncontrolled (BP ⩾ 140/90 mm Hg) despite the use of ⩾ 3 antihypertensive medication classes, including a diuretic, or the use of ⩾ 4 antihypertensive medication classes, including a diuretic, to achieve BP control.1 The prevalence of aTRH is common and African Americans have a higher prevalence of aTRH compared with Whites.2 Approximately 15% of adults taking antihypertensive medication have aTRH,3 which is associated with increased risk of adverse cardiovascular outcomes including incident myocardial infarction, heart failure, stroke and chronic kidney disease.4–6
Several studies have identified demographic and clinical risk factors associated with aTRH including male sex, older age, African American race, longer duration of hypertension and poorer cardiovascular risk profile.5,7 However, little is known about whether psychosocial factors may influence aTRH. Elevated stress, depression and low social resources have been linked to poor BP control8–10 and are each plausible risk factors for aTRH. Understanding the role that psychosocial factors may have in aTRH is important because a significant proportion of individuals with aTRH have uncontrolled BP despite being adherent to their medications4—that is—‘true’ TRH (hypertension that is inadequately controlled by medications) vs ‘pseudo’ TRH (hypertension that is inadequately controlled owing to medication non-adherence or white coat effect). Therefore, research is needed to identify adjunctive non-pharmacological targets (for example, poor coping skills, depression and low social resources) to improve BP that remains uncontrolled despite adherence to antihypertensive medications.
The objective of this cross-sectional analysis was to explore the psychosocial correlates of aTRH in participants with hypertension who were adherent to their antihypertensive medications in the Jackson Heart Study (JHS), an exclusively African American cohort. This investigation will help to inform whether modifiable psychosocial factors should be considered targets for treatment, concurrent with treatment using antihypertensive medications.
MATERIALS AND METHODS
Participants
The JHS is a population-based cohort study designed to investigate the causes of cardiovascular disease (CVD) in African Americans. A total of 5306 participants were enrolled from the Jackson, Mississippi metropolitan area between 2000 and 2004. Details of the study design, recruitment and data collection are published elsewhere.11 The study was approved by the institutional review boards of the participating institutions: The University of Mississippi Medical Center, Jackson State University and Tougaloo College. All participants provided informed consent. For this cross-sectional analysis, the sample was restricted to participants with hypertension who self-reported antihypertensive medication use in the last 2 weeks and had one or more classes of antihypertensive medication identified during a review of their pill bottles (n = 2462). Participants with missing clinic BP and/or antihypertensive medication adherence data were excluded (n = 15). Participants who had uncontrolled BP and were taking two or fewer classes of antihypertensive medication (n = 597) were additionally excluded because these participants could not be classified as having or not having aTRH using the s.d. Participants who had uncontrolled BP on three or more medications without a diuretic and controlled on four or more medications without a diuretic were also excluded (n = 25). Finally, participants who reported not taking one or more of their prescribed antihypertensive medications in the past 24 h (n = 433) were excluded to ensure that the sample was restricted to individuals who were less likely to be erroneously categorised as having aTRH based on medication non-adherence. After these exclusions, the final analytic sample included 1392 participants.
Data collection and BP measurement
Data for this study were collected during a baseline in-home interview and a baseline clinic visit, which followed the home interview. After a 5 min rest period, the mean of two clinic BP measurements, taken 1 min apart with a Hawksley random zero sphygmomanometer (Hawksley and Sons Ltd, Langing, UK), was used to assess baseline BP. Quality control was maintained by using an appropriately sized cuff, technician recertification, procedural checklists and data review.
Self-reported medication adherence
Information about self-reported medication adherence was collected during the baseline clinic visit, whereby participants were asked to bring in all medications that they had taken in the past 2 weeks. Study personnel recorded the names of these medications and asked participants whether they had taken each medication in the past 24 h. We categorised participants who had reported taking all of their prescribed antihypertensive medications in the past 24 h as being adherent. Those who reported that they did not take one or more antihypertensive medication were categorised as non-adherent and were excluded from analyses. Antihypertensive medications included the following classes: angiotensin converting enzyme inhibitors, beta blockers, calcium channel blockers, angiotensin receptor blockers, mineralcorticoid (aldosterone) receptor antagonists, alpha blockers, direct-acting vasodilators, renin inhibitors, central acting agents and diuretics.
Definition of aTRH
aTRH was defined as having uncontrolled clinic BP (systolic BP ⩾ 140 mm Hg or diastolic BP ⩾ 90 mm Hg) despite the use of ⩾ 3 antihypertensive medication classes (including a diuretic) or controlled BP with ⩾ 4 classes of antihypertensive medications (including a diuretic). Participants without aTRH, defined as taking ⩽ 3 classes of antihypertensive medication with controlled BP, served as the referent group.
Psychosocial factors
Chronic stress was measured using the Global Perceived Stress Scale,12 a measure of stress experienced over the prior 12 months in eight life domains including job, neighbourhood, caregiving, relationships, legal, medical, racism and discrimination, and meeting basic needs. Scores range from 0 to 24. Higher scores indicated greater chronic stress. Depressive symptoms were measured using the 20-item Center for Epidemiologic Studies Depression scale (CESD-R). Scores range from 0 to 60. Higher scores indicated higher levels of depressive symptoms in the past week.13 Perceived social support was assessed with a 16-item version of the Interpersonal Support Evaluation List, a measure of currently perceived availability of four types of support: tangible, emotional, belonging and self-esteem.14 Scores range from 0 to 48. Higher scores indicated greater perceived support. Social network was assessed with a 5-item measure adapted from the Berkman Social Network Scale,15 which assesses five different types/characteristics of social relationships: current cohabitation status, group membership, close friends, close relatives and frequency of social contact. Each item was coded dichotomously. For cohabitation, a score of 0 indicated living alone, and a 1 indicated living with a spouse or significant other. For group membership, close friends and close relatives (three separate items), a score of 0 reflected the absence of each type of social relationship. A score of 1 reflected having one or more groups, one or more close friends, and one or more close relatives, respectively. For frequency of social contact, a score of 0 indicated less than one contact with friends or relatives per month, and a score of 1 indicated at least one contact with friends or relatives per month. Total scores on this measure range from 0 to 5. Higher scores reflected a more diverse (that is, a greater number of different sources of social contact) and active social network.15
Covariates
Demographic, clinical and behavioural covariates that have been related to aTRH in prior investigations or may be plausibly linked with aTRH were included in the current analyses.
Demographic covariates.
Demographic factors included age, sex, education and income. A continuous measure of education was created based on methods used in prior JHS studies by assigning 12 years for a high school graduate equivalency degree, 13 years for a vocational or trade certificate or for some college but no degree, 14 years for an associate degree, 16 years for a bachelor degree, and 20 years for a graduate or professional degree.16 A continuous measure of annual family income was created using the median value of each of 11 income categories and adjusting for household size.
Clinical covariates.
Body mass index was calculated using height and weight measured at the baseline clinic visit. CVD was defined by self-reported history of myocardial infarction, stroke or coronary revascularisation procedures. Diabetes was defined by fasting glucose level ⩾ 126 mg dl−1 or haemoglobin A1c ⩾ 6.5% or use of diabetic medication within 2 weeks prior to the clinic visit (based on pill bottle review or self-reported). Albuminuria was defined by having a urine albumin to creatinine ratio >30 mg g−1 on either spot urine or 24 h urine measures. Estimated glomerular filtration rate was calculated using age, sex and Cleveland Clinic calibrated values of serum creatinine using the Chronic Kidney Disease Epidemiology Collaboration equation.17
Behavioural covariates.
Physical activity was measured using an 18-item scale that assessed three domains (active living, home and garden, and sport and exercise). Questions were modified from the Kaiser Physical Activity Survey, which was based on methods used in the Atherosclerosis Risk in Communities study and has recently been validated in a multiethnic sample of women.18 Total scores were categorised into poor, intermediate and ideal physical activity levels based on the American Heart Association Life’s Simple 7 guidelines. Current smoking was scored dichotomously and assessed by self-report. Alcohol use was scored dichotomously and assessed by any self-reported drinking in the past 12 months. Dietary factors including daily intake of sodium (mg) and potassium (mg) were extracted from responses to the Food Frequency Questionnaire, validated for use in the JHS sample.19
Statistical analyses
Covariates and psychosocial factors were compared between participants with and without aTRH using t-tests and χ2-tests. The association of each psychosocial factor (chronic stress, depressive symptoms, perceived social support and social network) with aTRH was examined in Poisson regression models with progressive adjustment for covariates. Our primary model included adjustment for age and sex. In sensitivity analyses, we also examined a model fully adjusted for covariates including age, sex income, education, clinical factors (body mass index, diabetes status, CVD status, albuminuria status and estimated glomerular filtration rate), as well as behavioural factors (alcohol use, smoking, sodium intake, potassium intake and physical activity). Other sensitivity analyses included testing the association of each of psychosocial factor with aTRH status when: (1) treatment with a diuretic was removed as a requisite for aTRH status and (2) participants with indeterminate aTRH (that is, participants taking ⩽ 2 classes of antihypertensive medication with uncontrolled BP) were included in the referent group without aTRH.
Age, income, years of education, body mass index, estimated glomerular filtration rate, sodium intake and potassium intake were treated as continuous covariates. Sex, diabetes status, CVD status, albuminuria status, smoking, alcohol use and physical activity were treated as categorical covariates. Multiple imputations using full conditional specification was used to impute missing values of covariates and predictors in all analyses. A total of 10 imputed data sets were created and predictor variables were standardised in each imputed data set so that all subsequent analyses using imputed data reflected pooled and standardised results. These methods have been used in recent studies using JHS data.20
Given our goal of generating hypotheses for future investigation, analyses were not corrected for multiple comparisons to minimise type II error, and to maximise power to detect potentially meaningful associations between the psychosocial factors and aTRH status.21,22 Power was further maximised by judiciously limiting predictors that have demonstrated associations with hypertension outcomes in prior studies.
RESULTS
Among the final sample of 1392 participants, 210 (15.1%) had aTRH. Participants with aTRH, compared with those without aTRH, were older; more likely to be male, and to have diabetes, CVD and albuminuria; had a lower mean estimated glomerular filtration rate and a lower mean dietary sodium (each P<0.05; Table 1). Participants with aTRH also had lower social network scores (P<0.01). Chronic stress, depressive symptoms and perceived social support did not differ significantly between participants with aTRH vs without aTRH.
Table 1.
Characteristics of the Jackson Heart Study participants, overall and by apparent treatment-resistant hypertension status
| Variable | Total (n = 1392) | Without aTRH (n = 1182) | aTRH (n = 210) |
|---|---|---|---|
| Demographic, clinical and behavioural factors | |||
| Age | 60.1 (0.3) | 59.8 (0.3) | 61.7 (0.7)* |
| Male gender, n (%) | 401 (28.8%) | 316 (26.7%) | 85 (40.5%)*** |
| Number of antihypertensive medication classes | 2.1 (0.0) | 1.8 (0.0) | 3.7 (0.0)*** |
| Body mass index, kg m−2 | 32.9 (0.2) | 32.7 (0.2) | 33.6 (0.5) |
| Income, $ | 18 459 (356.9) | 18 625 (391.6) | 17 524 (857.6) |
| Years of education | 13.5 (0.1) | 13.5 (0.1) | 13.2 (0.3) |
| Diabetes, n (%) | 489 (35.2%) | 378 (32.1%) | 111 (52.8%)*** |
| Cardiovascular disease, n (%) | 227 (16.3%) | 163 (13.8%) | 64 (30.3%)*** |
| Albuminuria, n (%)a | 244 (17.5%) | 184 (15.6%) | 60 (28.6%)*** |
| Estimated glomerular filtration rate, ml min−1b | 87.6 (0.6) | 88.9 (0.6) | 80.0 (1.7)*** |
| Alcohol use, n (%) | 505 (36.3%) | 440 (37.2%) | 65 (31.0%) |
| Current smoking, n (%) | 140 (10.1%) | 121 (10.2%) | 19 (9.0%) |
| Dietary sodium, mg | 3571.4 (53.0) | 3614.7 (58.4) | 3327.3 (124.7)* |
| Dietary potassium, mg | 2521.1 (33.4) | 2546.6 (36.5) | 2377.7 (82.6) |
| Physical activity, n (%) | |||
| Poor | 732 (52.6%) | 613 (51.9%) | 119 (56.7%) |
| Intermediate | 435 (31.2%) | 369 (31.2%) | 66 (31.4%) |
| Ideal | 225 (16.2%) | 200 (16.9%) | 25 (11.9%) |
| Psychosocial factors | |||
| Chronic stress | 4.7 (0.1) | 4.7 (0.1) | 4.7 (0.3) |
| Depressive symptoms | 11.3 (0.3) | 11.3 (0.3) | 11.8 (0.6) |
| Perceived social support | 36.9 (0.2) | 37.0 (0.2) | 36.1 (0.5) |
| Social network | 4.2 (0.0) | 4.3 (0.0) | 4.1 (0.1)** |
Abbreviation: aTRH, apparent treatment-resistant hypertension.
Albuminuria was defined as a urine albumin to creatinine ratio >30 mg g−1
Estimated glomerular filtration rate was calculated using age, sex and Cleveland Clinic calibrated values of serum creatinine using the Chronic Kidney Disease Epidemiology Collaboration equation. Note: all values are presented as mean (s.e.) unless noted otherwise.
P<0.05;
P<0.01;
P<0.001.
Psychosocial factors associated with aTRH
In regression analysis, social network was the only psychosocial factor that was significantly associated with aTRH prevalence (Table 2). Each additional unique type of social network was associated with a 19% lower prevalence of aTRH in our primary model, which adjusted for age and sex (prevalence ratio (PR) = 0.81; 95% confidence interval: 0.68–0.94, P = 0.001). Sensitivity analyses indicated that social network remained significantly associated with aTRH after further adjustment for income, education, clinical factors and behavioural factors (PR = 0.87; 95% confidence interval: 0.74–1.00, P = 0.041). Also the pattern and significance of these results were unaffected when treatment with a diuretic was removed as a requisite for aTRH status. Results were similarly unaffected when including participants with uncontrolled BP taking ⩽ 2 classes of antihypertensive medication in the referent group without aTRH. Figure 1 illustrates the linear association whereby the prevalence of aTRH was progressively lower with higher social network scores.
Table 2.
Prevalence ratios of apparent treatment-resistant hypertension associated with psychosocial factors
| Predictor | Primary model | Fully adjusted model |
|---|---|---|
| Prevalence ratio (95% CI) | Prevalence ratio (95% CI) | |
| Chronic stressk | 1.09 (0.97–1.22) | 1.09 (0.96–1.21) |
| Depressive symptoms | 1.09 (0.96–1.22) | 1.03 (0.89–1.16) |
| Perceived social support | 0.91 (0.79–1.03) | 0.96 (0.83–1.09) |
| Social network | 0.81 (0.68–0.94)** | 0.87 (0.74–1.00)* |
Abbreviation: CI, confidence interval. Numbers in table are prevalence ratio (95% confidence interval). Primary model: adjusted for age and sex. Fully adjusted model (sensitivity analysis): adjusted for age, sex, income, education, body mass index, diabetes status, cardiovascular disease status, albuminuria status, estimated glomerular filtration rate, alcohol use, smoking, sodium intake, potassium intake and physical activity. Note: as a categorical variable, social network is presented in original scale units. Other predictors (all except for social network) are reported in s.d. units. The s.d. are as follows: chronic stress s.d. = 4.22; depressive symptoms s.d. = 8.17; and perceived social support s.d. = 7.37.
P<0.05;
P<0.01.
Figure 1.
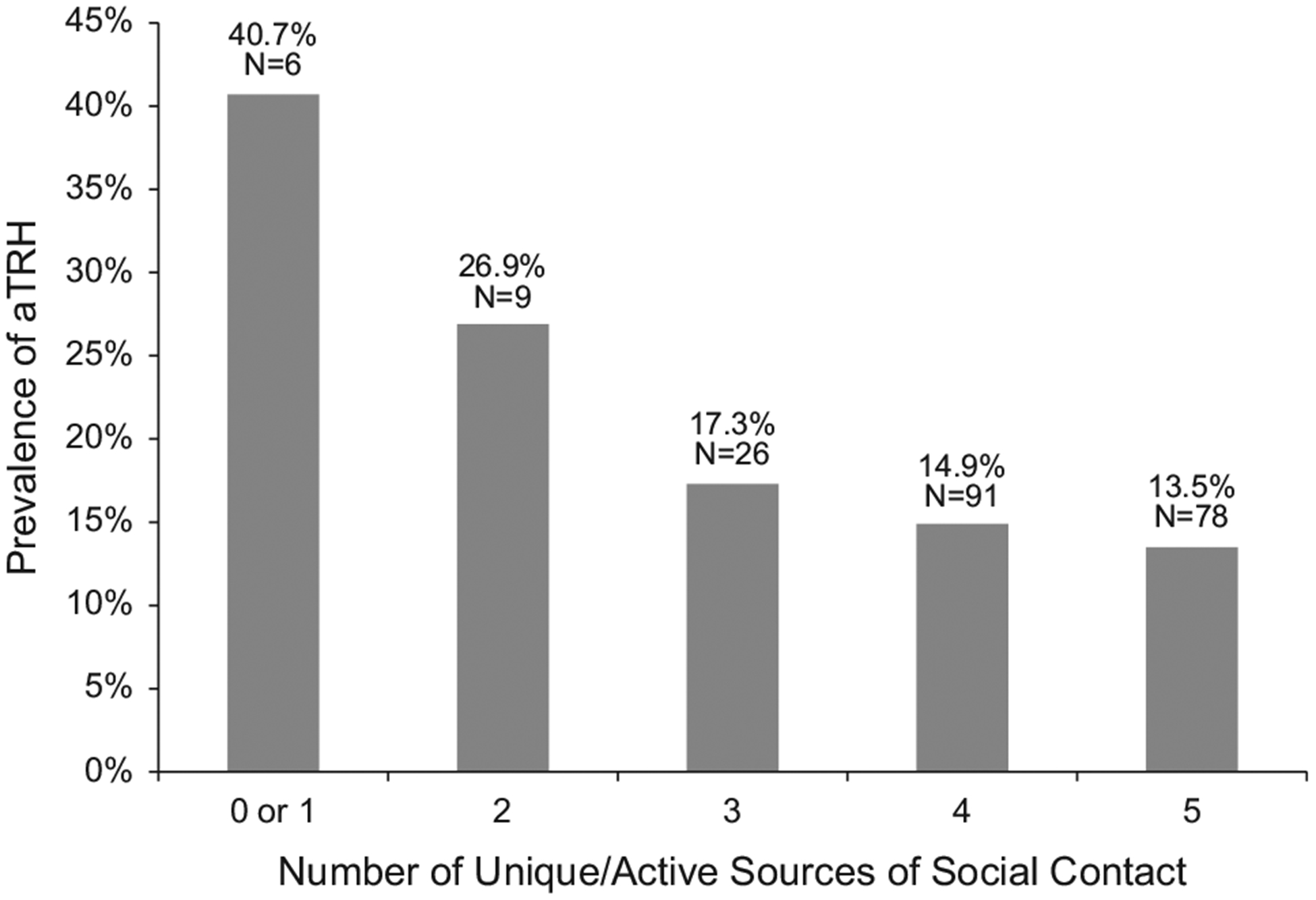
Prevalence of apparent treatment-resistant hypertension by social network (N = 1392). Note: Mantel–Haenszel test of linear association between aTRH prevalence and social network scores (P<0.01). A full colour version of this figure is available at the Journal of Human Hypertension journal online.
DISCUSSION
This study explored the association of psychosocial factors with aTRH in a large cohort of African Americans with hypertension who reported adherence to their antihypertensive medication. Results indicated that a broader (that is, more diverse) and more active social network was associated with a lower prevalence of aTRH. This association remained statistically significant after multivariable adjustment for demographic, clinical and behavioural factors. Chronic stress, depressive symptoms and perceived social support were not associated with aTRH.
This investigation is one of few studies to examine the association between psychosocial factors and aTRH. The finding that social network is a significant correlate of aTRH parallels growing evidence that larger social networks are associated with better physical health.23,24 In addition, the results of this study are consistent with findings from a large hypertension trial that demonstrated that African American patients who received a social network-based intervention were more likely to achieve an adequate BP treatment goal (systolic/diastolic BP <140/90 mm hg), compared with a control group receiving usual care.25
The finding that chronic stress and depressive symptoms, in particular, were not associated with aTRH is somewhat surprising, given evidence that each of these have been associated with hypertension in other studies.26 Prior investigations, however, have primarily demonstrated associations in younger African American samples and over long-term follow-up.27 Also, at least two prior studies have found depression and stress to be unrelated to hypertension in similar multiethnic cohort studies.8,28
The reason why social network, rather than a similar construct like perceived social support, is a correlate of aTRH may be because social network is a more objective marker of socio-emotional functioning29 and is also more stable over time.30 In addition, indirect evidence indicates that owing to exposure to race-related psychosocial stressors (for example, daily harassment), a broader social network may confer specific beneficial effects on BP control in African Americans.31 Additional research is necessary to determine the extent to which these benefits may exist among other racial/ethnic groups.
Although the observational study design prevents us from drawing conclusions about causality, social connectedness has been prospectively linked to cardiovascular outcomes, a finding that is consistent with a model whereby social network directly influences prevalence of aTRH.32,33 Both direct and indirect mechanisms have been hypothesised to explain the protective health effects of social network, including positive effects on physiological and behavioural influences, and buffering the negative effects of stress.34–36 We were unable to test mediational pathways, which require longitudinal data to confirm the time course of mechanisms. However, at least one large, racially diverse population study failed to find an association between unhealthy lifestyle factors (for example, physical activity, diet, smoking and alcohol consumption) and aTRH.7 These results are consistent with our findings whereby social network remained significantly associated with aTRH status after adjustment for clinical and behavioural factors. However, this association was weakened after including covariates. Thus, longitudinal studies are needed to conclusively determine the effects of social network on aTRH and the mechanisms underlying this association. Although social network was most strongly associated with aTRH, longitudinal studies may also reveal associations between other psychosocial factors and aTRH.
Strengths of this study include the large, population-based sample of African Americans, a population at high risk for aTRH, and the restriction to participants who reported being adherent to their antihypertensive medication and, thus, were most likely to have true vs pseudo TRH. This latter aspect is of particular importance given the dearth of studies that have the potential to inform non-pharmacological approaches to hypertension management in individuals whose BP remains uncontrolled despite taking antihypertensive medication. Also, the JHS involved extensive data collection, which allowed us to thoroughly examine the association between multiple psychosocial factors and aTRH while controlling for important demographic, clinical and behavioural factors.
Notwithstanding these strengths, several limitations are worth noting. Although the sample size of this investigation was comparable (if not larger) than similar studies,8,20,37 results must be considered in the context of limited statistical power, given that relatively few individuals had low social network scores. Confidence in our results is strengthened by the fact that results held when controlling for important demographic, clinical and behavioural confounders, and that findings replicated across multiple phenotypes of aTRH status. Also, results converge with theoretical considerations and empirical evidence demonstrating that social network may be an important correlate of hypertension outcomes.23,24 However, the possibility that the association between social network and aTRH is spurious cannot be ruled out, and results need to be confirmed in future studies.
Also, medication adherence was assessed by self-report and is therefore subject to social desirability and memory recall biases. This limitation is somewhat offset by the 24 h time reference for adherence, which is less likely to be influenced by inaccuracies in recollection. Still, objective measures of adherence such as electronic monitoring, pill counts or refill history would minimise subjective biases. A related limitation is that the 24 h time reference only captures very recent self-reported adherence to antihypertensive medications, which may have been overly inclusive of individuals who remembered to take their antihypertensive medications in the 24 h prior to the study visit, but who do not usually take their medications. Thus, some participants may not have ‘true’ TRH because their uncontrolled BP status may reflect ‘first-dose’ vs ‘steady-state’ effects.
Finally, ambulatory BP monitoring values were not considered in this study owing to a limited number of participants who had ambulatory BP monitoring performed in the JHS. Thus, we are unable to rule out pseudo TRH hypertension owing to a white coat effect.
CONCLUSIONS
Despite well-known clinical determinants of aTRH, little is known about the association between psychosocial factors and aTRH, particularly, among individuals who are adherent to their antihypertensive medication. This study demonstrates that a more diverse (that is, a greater number of different sources of social contact) and active social network is associated with a lower prevalence of aTRH. Important areas of future research include characterising the most beneficial types and sources of social relationships and the longitudinal effects of these networks on incident aTRH and hypertension-related outcomes. Given the high prevalence of aTRH among African Americans and the associated increased cardiovascular risk, the role of social network as a potentially modifiable correlate warrants further investigation. Findings from this study suggest that social network might be a potential target for interventions designed to reduce the prevalence of aTRH in African Americans with hypertension.
What is known about this topic?
Apparent treatment-resistant hypertension (aTRH) is common, disproportionately affects African Americans and is associated with adverse cardiovascular outcomes.
A significant proportion of individuals have ‘true’ TRH, whereby blood pressure remains uncontrolled despite being adherent to antihypertensive medications.
Demographic and clinical risk factors associated with aTRH are well known (male sex, older age, African American race, longer duration of hypertension and poorer cardiovascular risk profile), but it is not clear whether psychosocial factors may influence aTRH.
What this study adds?
This is the first study to test whether a range of theoretically plausible psychosocial factors are associated with aTRH.
Greater diversity of social networks is associated with reduced prevalence of aTRH in a large cohort of African Americans who are adherent to their antihypertensive medications and thus likely to have ‘true’ TRH.
This investigation lays the groundwork for future studies to test whether social networks are a viable target for the management of hypertension in individuals whose blood pressure remains uncontrolled despite taking antihypertensive medication.
ACKNOWLEDGEMENTS
We thank the participants and data collection staff of the Jackson Heart Study. The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung and Blood Institute; the National Institutes of Health; or the US Department of Health and Human Services. The Jackson Heart Study is supported by contracts HHSN268201300046C, HHSN268201300047C, HHSN268201300048C, HHSN268201300049C, HHSN268201300050C from the National Heart, Lung and Blood Institute, and the National Institute on Minority Health and Health Disparities.
Footnotes
CONFLICT OF INTEREST
The authors declare no conflict of interest.
REFERENCES
- 1.Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD et al. Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation 2008; 117: e510–e526. [DOI] [PubMed] [Google Scholar]
- 2.Howard VJ, Tanner RM, Anderson A, Irvin MR, Calhoun DA, Lackland DT et al. Apparent treatment-resistant hypertension among individuals with history of stroke or transient ischemic attack. Am J Med 2015; 128: 707–714, e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Judd E, Calhoun DA. Apparent and true resistant hypertension: definition, prevalence and outcomes. J Hum Hypertens 2014; 28: 463–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Irvin MR, Shimbo D, Mann DM, Reynolds K, Krousel-Wood M, Limdi NA et al. Prevalence and correlates of low medication adherence in apparent treatment-resistant hypertension. J Clin Hypertens 2012; 14: 694–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sim JJ, Bhandari SK, Shi J, Liu IL, Calhoun DA, McGlynn EA et al. Characteristics of resistant hypertension in a large, ethnically diverse hypertension population of an integrated health system. Mayo Clin Proc 2013; 88: 1099–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tanner RM, Calhoun DA, Bell EK, Bowling CB, Gutierrez OM, Irvin MR et al. Prevalence of apparent treatment-resistant hypertension among individuals with CKD. Clin J Am Soc Nephrol 2013; 8: 1583–1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shimbo D, Levitan EB, Booth JN 3rd, Calhoun DA, Judd SE, Lackland DT et al. The contributions of unhealthy lifestyle factors to apparent resistant hypertension: findings from the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study. J Hypertens 2013; 31: 370–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ford CD, Sims M, Higginbotham JC, Crowther MR, Wyatt SB, Musani SK et al. Psychosocial factors are associated with blood pressure progression among African Americans in the Jackson Heart Study. Am J Hypertens 2016; 29: 913–924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cornwell EY, Waite LJ. Social network resources and management of hypertension. J Health Soc Behav 2012; 53: 215–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steptoe A, Kivimaki M. Stress and cardiovascular disease: an update on current knowledge. Annu Rev Public Health 2013; 34: 337–354. [DOI] [PubMed] [Google Scholar]
- 11.Taylor HA Jr, Wilson JG, Jones DW, Sarpong DF, Srinivasan A, Garrison RJ et al. Toward resolution of cardiovascular health disparities in African Americans: design and methods of the Jackson Heart Study. Ethn Dis 2005; 15: S6–4–17. [PubMed] [Google Scholar]
- 12.Payne TJ, Wyatt SB, Mosley TH, Dubbert PM, Guiterrez-Mohammed ML, Calvin RL et al. Sociocultural methods in the Jackson Heart Study: conceptual and descriptive overview. Ethn Dis 2005; 15(Suppl 6): S6–38–48. [PubMed] [Google Scholar]
- 13.Radloff LS. The CES-D scale: a self report depression scale for research in the general population. Appl Psychol Meas 1977; 1: 385–401. [Google Scholar]
- 14.Cohen S, Hoberman H. Positive events and social supports as buffers of life change stress. J Appl Soc Psychol 1983; 13: 99–125. [Google Scholar]
- 15.Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol 1979; 109: 186–204. [DOI] [PubMed] [Google Scholar]
- 16.Hickson DA, Diez Roux AV, Wyatt SB, Gebreab SY, Ogedegbe G, Sarpong DF et al. Socioeconomic position is positively associated with blood pressure dipping among African-American adults: the Jackson Heart Study. Am J Hypertens 2011; 24: 1015–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stevens LA, Schmid CH, Greene T, Zhang YL, Beck GJ, Froissart M et al. Comparative performance of the CKD Epidemiology Collaboration (CKD-EPI) and the Modification of Diet in Renal Disease (MDRD) Study equations for estimating GFR levels above 60 mL/min/1.73 m2. Am J Kidney Dis 2010; 56: 486–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smitherman TA, Dubbert PM, Grothe KB, Sung JH, Kendzor DE, Reis JP et al. Validation of the Jackson Heart Study Physical Activity Survey in African Americans. J Phys Act Health 2009; 6: S124–S132. [DOI] [PubMed] [Google Scholar]
- 19.Carithers T, Dubbert PM, Crook E, Davy B, Wyatt SB, Bogle ML et al. Dietary assessment in African Americans: methods used in the Jackson Heart Study. Ethn Dis 2005; 15: S6–49–55. [PubMed] [Google Scholar]
- 20.Spruill TM, Shallcross AJ, Ogedegbe G, Chaplin WF, Butler M, Palfrey A et al. Psychosocial correlates of nocturnal blood pressure dipping in African Americans: The Jackson Heart Study. Am J Hypertens 2016; 29: 904–912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maxwell SE. The persistence of underpowered studies in psychological research: causes, consequences, and remedies. Psychol Methods 2004; 9: 147–163. [DOI] [PubMed] [Google Scholar]
- 22.Perneger TV. What’s wrong with Bonferroni adjustments. BMJ 1998; 316: 1236–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berkman LF. Social support, social networks, social cohesion and health. Soc Work Health Care 2000; 31: 3–14. [DOI] [PubMed] [Google Scholar]
- 24.Eng PM, Rimm EB, Fitzmaurice G, Kawachi I. Social ties and change in social ties in relation to subsequent total and cause-specific mortality and coronary heart disease incidence in men. Am J Epidemiol 2002; 155: 700–709. [DOI] [PubMed] [Google Scholar]
- 25.Shaya FT, Chirikov VV, Daniel Mullins C, Shematek J, Howard D, Foster C et al. Social networks help control hypertension. J Clin Hypertens 2013; 15: 34–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pickering TG. Mental stress as a causal factor in the development of hypertension and cardiovascular disease. Curr Hypertens Rep 2001; 3: 249–254. [DOI] [PubMed] [Google Scholar]
- 27.Davidson K, Jonas BS, Dixon KE, Markovitz JH. Do depression symptoms predict early hypertension incidence in young adults in the CARDIA study? Coronary Artery Risk Development in Young Adults. Arch Intern Med 2000; 160: 1495–1500. [DOI] [PubMed] [Google Scholar]
- 28.Delaney JA, Oddson BE, Kramer H, Shea S, Psaty BM, McClelland RL. Baseline depressive symptoms are not associated with clinically important levels of incident hypertension during two years of follow-up: the multi-ethnic study of atherosclerosis. Hypertension 2010; 55: 408–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Heaney CA, Israel BA. Social networks and social support In: Glanz K, Rimer BK, Lewis FM (eds). Health Behavior and Health Education: Theory, Research and Practice, 3rd edn Jossey-Bass: San Francisco, CA, USA, 2002, pp 185–209. [Google Scholar]
- 30.Kossinets G, Watts DJ. Empirical analysis of an evolving social network. Science 2006; 311: 88–90. [DOI] [PubMed] [Google Scholar]
- 31.Schoenthaler AM, Schwartz J, Cassells A, Tobin JN, Brondolo E. Daily interpersonal conflict predicts masked hypertension in an urban sample. Am J Hypertens 2010; 23: 1082–1088. [DOI] [PubMed] [Google Scholar]
- 32.Kawachi I, Colditz GA, Ascherio A, Rimm EB, Giovannucci E, Stampfer MJ et al. A prospective study of social networks in relation to total mortality and cardiovascular disease in men in the USA. J Epidemiol Community Health 1996; 50: 245–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J Am Coll Cardiol 2005; 45: 637–651. [DOI] [PubMed] [Google Scholar]
- 34.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull 1985; 98: 310–357. [PubMed] [Google Scholar]
- 35.Uchino BN, Cacioppo JT, Kiecolt-Glaser JK. The relationship between social support and physiological processes: a review with emphasis on underlying mechanisms and implications for health. Psychol Bull 1996; 119: 488–531. [DOI] [PubMed] [Google Scholar]
- 36.Umberson D, Crosnoe R, Reczek C. Social relationships and health behavior across life course. Annu Rev Sociol 2010; 36: 139–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Diaz KM, Veerabhadrappa P, Brown MD, Whited MC, Dubbert PM, Hickson DA. Prevalence, determinants, and clinical significance of masked hypertension in a population-based sample of African Americans: The Jackson Heart Study. Am J Hypertens 2015; 28: 900–908. [DOI] [PMC free article] [PubMed] [Google Scholar]


