Abstract
Context:
Alloplastic temporomandibular joint (TMJ) replacement is a treatment strategy for segmental mandibular defects with occlusal abnormalities.
Aims:
To describe our experience with extended total TMJ replacement (eTMJR) by reporting operative obstacles, complications, and patient-reported outcomes, as well as to suggest a subclassification system and paradigm shift.
Setting and Design:
University hospital and private clinic; case series with retrospective follow-up.
Methods and Materials:
Five patients (6 eTMJRs) were followed for more than 1 year after surgery. Patient-reported outcomes were assessed using FACE-Q™ “Satisfaction with Outcome” questionnaires (sum and corresponding transformed Rasch scores).
Statistical Analysis:
Descriptive analyses were performed.
Results:
Problems were related to contralateral mandibular osteotomy healing (if performed), keying the prosthetic condyle into the fossa component, intra- and postoperative prosthetic lag, and intraoperative proper establishment of the occlusion when unilateral replacement was performed. Patients reported high satisfaction with the outcome, with a mean Rasch score of 89.2/100.
Conclusions:
Unilateral eTMJR obstacles related to three-dimensional rotational repositioning of the remaining mandible. We suggest a paradigm shift, considering primary alloplastic replacement instead of microvascular osseous transplantation for reconstruction when radiotherapy is not required. This can avoid donor site morbidity and long reconstructive surgery. An autologous osseous transplant is still available in case of implant failure. A subclassification system is proposed for eTMJR, which accounts for contour corrections, occlusal adjustments, and simultaneous contralateral mandibular osteotomy.
Keywords: Arthroplasty, temporomandibular joint, total joint replacement
INTRODUCTION
Extended temporomandibular joint (TMJ) prostheses replace not only joint components but also adjacent mandibular and/or temporal bone defects.[1] We recently shifted from autologous to alloplastic replacement for a number of segmental mandibular defects, considering autologous replacement as a salvage procedure for implant failure. A similar strategy was advocated in 1999 by Peckitt in oncological cases.[2] It was heavily criticized and did not become popular in the pre-three-dimensional (3D) printing era. We herein review our experience with total alloplastic extended TMJ replacement (eTMJR), describing intraoperative obstacles and deficiencies in occlusal and esthetic outcomes. Our experience may guide future reconstructive surgeries.
MATERIALS AND METHODS
We analyzed the records of all patients who received an additively manufactured eTMJR (CADSkills bv, Gent, Belgium) [Figure 1] implant in 2017 and 2018. All operations were performed by the same surgeon (MYM). The following information was extracted from the records: age, sex, diagnosis, Elledge classification,[3] simultaneous corrections of occlusion and facial contours, intraoperative obstacles, and postoperative complications.
Figure 1.

Rendered basilar view of the eTMJR of Case #2 showing its components. (A) Mandibular component three-dimensional printed out of Titanium Grade 23. (B) Cranial base part of the fossa component, three-dimensional printed out of Titanium Grade 23. (C) Caudal part of the fossa component, CNC-milled out of UHMWPE enriched with alpha-tocopherol and crosslinked using 100 Gy gamma irradiation. Note the posterior lip extending caudally. CNC=Computer numerical controlled; UHMWPE=Ultra-high-molecular-weight polyethylene
To evaluate patient satisfaction with their results, independent of the clinician's perception, all patients completed the standardized FACE-Q™ “Satisfaction with Outcome” questionnaire at the latest follow-up consultation.[4] Both the sum scores (maximum of 24) and corresponding transformed Rasch scores (maximum of 100) were determined. Statistical analysis was limited to descriptive statistics, with calculation of the mean Rasch score.
RESULTS
All patients were followed up for at least 1 year after their eTMJR surgery. In all patients, healing occurred without any complications, such as infection, dehiscence, or implant exposure.
Case #1
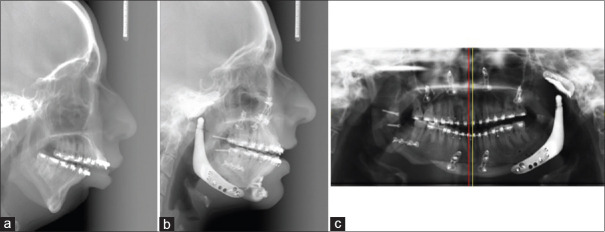
This patient had Pruzansky-Kaban Type IIb hemifacial microsomia. The planned position of the mandibular component at the lateral mandibular surface required changing intraoperatively because of severe lateral deviation of the occlusion, despite resection of the coronoid process. The vertical ramus compartment probably lacked neuromuscular support because of the underlying microsomia. Although neutral occlusion and midline correction were obtained during surgery, they were not fully maintained postoperatively [Figures 2 and 3]. Subsequent elastic traction and orthodontic treatment resulted in functional occlusion but with midline deviation.
Figure 2.
Case #1. Planning in ProPlan CMF (Materialize, Leuven, Belgium). (A) Frontal view. (B) Frontal view. Planned maxillary and mandibular rotation repositioning osteotomy. The arrow indicates the sagittal split osteotomy on the side contralateral to the extended temporomandibular joint replacement. (C) Left profile view. (D) Left profile view. Planned maxillary and mandibular rotation repositioning osteotomy planned. The arrow indicates the coronoidotomy
Figure 3.
Case #1 continued. (a) Preoperative profile cephalogram. (b) Postoperative profile cephalogram. (c) Orthopantomogram. The red line indicates the upper dental midline, and the yellow line indicates the lower dental midline
Case #2
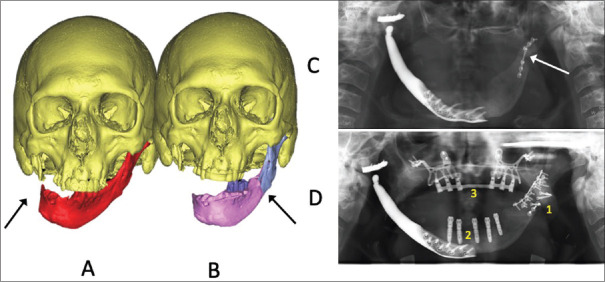
This patient sustained traumatic facial injuries when her village was bombed in 2007. She initially underwent reconstruction surgery in Germany, including polyether ether ketone zygoma replacement and placement of an artificial eye. The mandibular reconstruction subsequently failed, and she presented to our institution with a chronic plate infection, malunion, a mandibular defect, and fibrous TMJ ankylosis on the affected side [Figure 4]. During eTMJR, it was extremely difficult to seat the prosthetic condyle in the fossa component. The mandibular component was pushed inwardly by the scarred soft tissues at the mandibular angle. The reconstruction plate had been segmented out and was removed during implant insertion. The residual bony and titanium irregularities were difficult to match in the parasymphyseal region [Figure 4]. Finally, the bony surface was smoothened, and extreme force was required to guide the condyle into a proper position mediolaterally. Intraoperative 3D Pulsera imaging (Phillips, Eindhoven, The Netherlands) was repeated three times. Stable occlusion and articulation were achieved, with full occlusal contact at both sides checked with thin double-sided articulating paper and a spontaneous maximal mouth opening of 31 mm. Still, the alloplastic condyle seemed caudally positioned in relationship to the fossa on the computed tomography (CT) scan, even taking into account, the ultra-high-molecular-weight polyethylene part of the fossa component being radiolucent.
Figure 4.

Case # 2. Planning and postoperative result. (A) Surface tesselation language render with arrow indicating the mandibular defect. The left zygoma was replaced with a polyether ether ketone implant (blue). (B) Surface tesselation language render with the arrow indicating bony irregularities at the mandibular border after virtual removal of the titanium reconstruction plate using segmentalization. (C) Surface tesselation language render with the extended temporomandibular joint replacement indicated in gray. (D) Postoperative frontal view of the computerized scan of the cranium showing the condylar sag (arrow)
Case #3
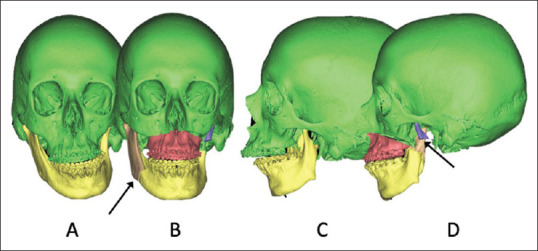
This patient initially had pericoronitis of the lower right third molar, and subsequently developed osteomyelitis after the tooth was extracted. The infection did not resolve with antibiotics and decortication, so the patient underwent resection with microvascular fibula flap reconstruction of the mandibular defect and this also had failed. By the time we saw the patient, there was extra bony ankylosis of the TMJ and extra- and intra-oral fistulization. Intravenous and prolonged peroral antibiotic treatment eradicated the infection. Segmentation of the CT DICOM dataset was performed using Mimics inPrint 3.0 (Materialise, Leuven, Belgium), with repositioning of the residual mandible using ProPlan CMF (Materialise, Leuven, Belgium). The latter needed a repositioning osteotomy on the left [Figure 5]. eTMJR and unilateral sagittal osteotomy were thereby performed simultaneously. Malunion, plate fracture, and cranial rotation of the left-sided proximal segment necessitated revision surgery using an iliac bone graft and comprehensive intraoral plating during a second surgical session, at which time root implants were placed in the anterior mandible. Blood analysis did not show any abnormalities of bone metabolism. The patient received an additively manufactured subperiosteal jaw implant under general anesthesia during a third operation and is currently undergoing prosthetic rehabilitation.
Figure 5.
Case # 3. (A) Surface tesselation language render with the arrow indicating the defect. (B) Surface tesselation language render with planned reotational repositioning of the mandible. The arrow indicates the sagittal split osteotomy contralateral to the extended temporomandibular joint replacement. (C) Orthopantomogram demonstrating an osteosynthesis plate fracture (arrow). (D) Orthopantomogram demonstrating extensive osteosynthesis and iliac bone grafting (1), root-shaped dental implants (2), and an additively manufactured subperiosteal jaw implant (3) one has the impression that mandible was splitted at a higher position than indicated in B. This is due to the fact that the proximal segment rotated anterocranially because of the malunion and because of the projective geometry of orthopantomogram technology
Case #4
This patient previously underwent bimaxillary surgery alio loco for Class II, open bite occlusion[Figure 6]. She presented with bilateral condylar resorption and extreme pain (10 on a 0–10 visual analog scale). Conservative measures, including bite splint, physiotherapy, pain medications, and steroid injections, over 1 year did not help. The patient developed mental depression, at which time, it was decided that she should undergo bilateral eTMJR, together with surgically-assisted maxillary expansion using a transpalatal distraction device (Surgi-Tec, Gent, Belgium), to replace the missing bone, correct the mandibular position, and remove the source of pain. Asymmetry at the gonial angles was managed with augmentation of the eTMJR. We planned to not fully correct the left side for two reasons. One reason was that the patient would have required an extended period of treatment, beginning with surgery to correct the transverse relapse of the upper dental arch, followed by orthodontic treatment, and then, the eTMJR operation after a considerable amount of time. Because of her pain, depression, and marital relationship, such prolonged treatment was deemed inappropriate. The second reason was that with her rotated mandible, the subcondylar area on the left would show a concavity if the angle were symmetrically augmented.
Figure 6.
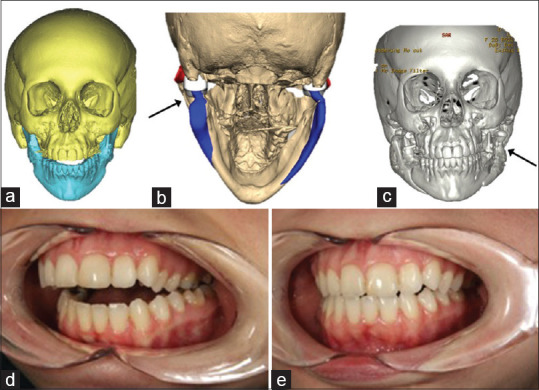
Case # 4. (a) Surface tesselation language render before planning demonstrating the anterior open bite. (b) Surface tesselation language render after planning for bilateral extended temporomandibular joint replacement and mandibular repositioning. The arrow indicates the concavity in the subcondylar area secondary to postoperative maintenance of the yaw position of the mandible and the attempt to symmetrize the mandibular angle area by augmentation. (c) Postimplantation computed tomography scan, frontal view. The arrow indicates the mid-cheek concavity. (d) Left — profile view of the preoperative occlusion. (e) Left — profile view of the post-extended temporomandibular joint replacement. occlusion
Case #5
This patient was initially treated for fibrous dysplasia with continuity resection at her left mandibular angle [Figure 7]. The defect was reconstructed using a free iliac bone graft, which failed. She was left with a dangling mandible for 2.5 years. During the eTMJR surgery, optimal occlusion could not be achieved. Manipulation at the resection stump was difficult because of the resistance to upward rotation and our decision to not lengthen the submandibular incision. Orthodontic treatment was resumed 1 year after the surgery. Prosthetic rehabilitation is planned for.
Figure 7.
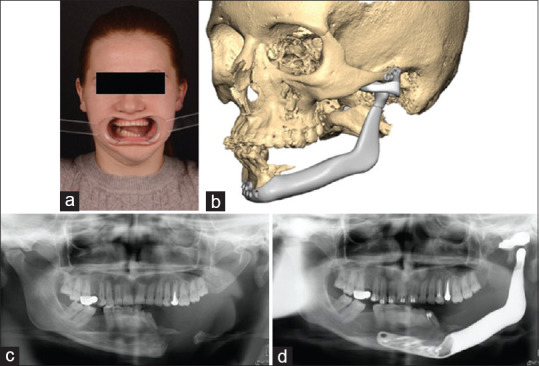
Case # 5. (a) Preoperative facial frontal view with open mouth. (b) Surface tesselation language render of the planned extended temporomandibular joint replacement. (c) Orthopantomogram showing the preoperative occlusion and left-sided mandibular defect. (d) Orthopantomogram showing the postoperative occlusion and extended temporomandibular joint replacement in situ
The results of the FACE-Q™ questionnaire are presented in [Tables 1 and 2]. While one patient reported a lower Rasch score (59/100), all other patients evaluated their satisfaction with the implant between 87/100 and 100/100, representing excellent results. The mean Rasch score was 89.2/100.
Table 1.
Number of patients reporting each FACE-Q™ “Satisfaction with outcome” rating
| Outcome | Very dissatisfied | Somewhat dissatisfied | Somewhat satisfied | Very satisfied |
|---|---|---|---|---|
| I am pleased with the result | 0 | 0 | 1 | 4 |
| The result turned out great | 0 | 0 | 1 | 4 |
| The result was just as I expected | 0 | 0 | 1 | 4 |
| I am surprised at how good I look in the mirror | 0 | 0 | 1 | 4 |
| The result is fantastic | 0 | 0 | 1 | 4 |
| The result is miraculous | 0 | 0 | 2 | 3 |
Table 2.
FACE-Q™ “Satisfaction with outcome” scores for each patient
| Case | Sum score (maximum, 24) | Equivalent Rasch transformed score (maximum, 100) |
|---|---|---|
| # 1 | 18 | 59 |
| # 2 | 23 | 87 |
| # 3 | 24 | 100 |
| # 4 | 24 | 100 |
| # 5 | 24 | 100 |
DISCUSSION
During eTMJR surgery, we encountered a number of obstacles. Adjustment at both sides of the implant was the most frequent (Cases #1, #4, and #5). Neuromuscular deficiency of the pterygomasseteric sling was likely the reason for the occlusal deviation observed in case #1 [Figure 3]. Lack of manual control over the vertical position of the condyle in the fossa before the screw fixation was likely the reason in case #2 [Figure 4]. The difficulty in retrieving the proper position at the symphysis, necessitating modification of the contact surfaces, probably contributed to the slight malpositioning as well. Both of these patients also had facial paresis on the affected side, but that was probably a coincidence. The solution could involve suture suspension of the prosthetic condyle to the prosthetic fossa and proper fixation of the pterygomasseteric sling through holes in the gonial region [Figure 8].[5] Case #3 had a diminutive and mostly cortical area on the contralateral osteotomy side, with rotation of the segments in three planes; there was considerable space between the segments but no space for bicortical screw osteosynthesis. Delayed union was also observed after revision surgery, involving extensive osteosynthesis plus addition of a cancellous bone block and particulate cancellous bone between the repositioned segments [Figure 5].
Figure 8.
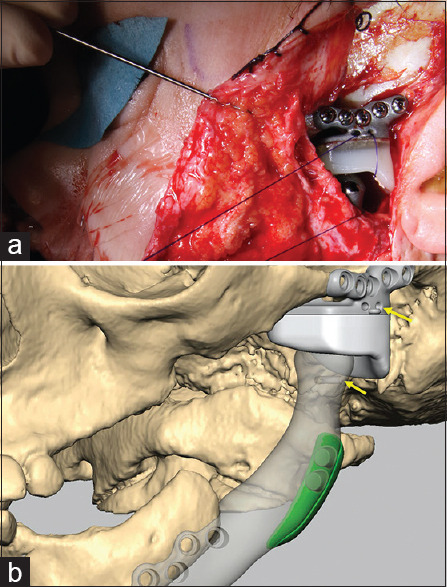
The condyle is sutured suspended to the fossa. (a) Intraoperative view of a case not presented in this article. (b) Render of the eTMJ of the case in A, demonstrating the tunnels in the fossa and the condyle (yellow arrows) meant for suture suspension
Facial contouring can be performed with eTMJR. The less than ideal outcome in case #4 was related to the decision to not delay the eTMJR surgery. The importance of facial contouring and correct anatomical reconstruction of the face was clear when evaluating patient-reported outcomes with the FACE-Q™ “Satisfaction with outcome” questionnaire. While four of our five patients reported a perfect or excellent score, case #1 reported a considerably lower score (59/100). It should, however, be noted that this patient had hemifacial microsomia and underwent several other treatments (e.g., autologous ear reconstruction and free gluteal fat grafting) before and after eTMJR and facial rotation surgery to improve her facial appearance. As such, only partial esthetic facial reconstruction could be achieved by eTMJR, which likely explained the reported esthetic result.
Elledge et al. stated that any classification system for eTMJR must be “unambiguous and easy to use; exhaustive and mutually exclusive so that each possibility exists in only one class; clinically relevant and appropriate; and flexible enough to accommodate any advances or changes in technology.”[3] Considering our (albeit limited) experience, it appeared that unidimensional extension was not the only factor affecting technical difficulties and outcomes. Indeed, we found no difference between M1 and M2 eTMJR with respect to surgical difficulties or clinical outcomes. In contrast, mandibular repositioning in three dimensions to deal with dental occlusion, with or without contralateral mandibular osteotomies, posed major obstacles and complications. Contour corrections increased the difficulty of implantation and resulted in compromised esthetic outcomes. Elledge et al. agreed that other subclassifications can be considered when autogenous tissue transfer is used in conjunction with eTMJR.[3] We, therefore, suggest adding the aforementioned potential obstacles (contour corrections, occlusal adjustments, and simultaneous contralateral mandibular osteotomy) as a subclassification system [Table 3]. Identification and anticipation of these obstacles may lead to facilitating actions.
Table 3.
Patient demographics, pathology, surgery classification and subclassification, and additional treatments
| Patient #, sex | Pathology | Age at eTMJR (years) | Laterality | Cl | Div | Other corrective osteotomies | Other procedures at a later date |
|---|---|---|---|---|---|---|---|
| 1, female | Hemifacial microsomia | 22 | Left | M0 | O, C, A | Le Fort I-type osteotomy, sliding genioplasty | Free gluteal fat transplantation |
| 2, female | Posttraumatic angle defect and malunion | 43 | Left | M2 | O | - | - |
| 3, male | TMJ ankylosis and osteomyelitis with failed microvascular fibula replacement | 46 | Right | M2 | O, C | - | AMSJI, root implants |
| 4, female | Condylar resorption after bimaxillary surgery | 25 | Left and right | M0 | O, A | TPD | - |
| 5, female | Resection of fibrous dysplasia and loss of subsequent iliac bone graft | 25 | Left | M2-3 | O | - | - |
AMSJI=Additively manufactured subperiosteal jaw implant; Cl=Classification according to Elledge et al.[3]; Div=Suggested subclassification according to occlusal correction (O), C=Contralateral mandibular osteotomy; A=Extra contour correction by augmentation (A); eTMJR=Extended alloplastic TMJ replacement; TMJ=Temporomandibular joint; TPD=Transpalatal distraction osteogenesis
Bredell et al.[6] described 15 patients requiring ablative surgery of the mandible (including the condyles), mainly for oncological reasons. Two patients received a reconstruction plate with a metallic condyle, whereas the others underwent autologous replacement, primarily with a free fibula flap. The authors focused on complications and concluded that “free vascularized grafts, specifically fibula, appear to be the option with the lowest surgical complication rate and good function that must be weighed against donor-site morbidity in high-risk cases.” However, additive manufacturing was not yet an option between 2001 and 2012, when that study was conducted. Our indications for surgery differed from those in the Bredell et al.[6] study, and we consider autologous reconstruction to be a second-choice option when dealing with nonmalignant tumors or other conditions. In addition to the advantage of more anatomically accurate reconstruction of the mandible with alloplastic eTMJR, the durations of both surgery and hospital stay are shorter with alloplastic reconstruction than with free vascularized grafts. Although the costs of materials may be relatively high with alloplastic eTMJR, the shorter durations not only lower morbidity risks but also reduce total costs, compared to autologous treatment options.[7,8] Furthermore, graft resorption, fracturing, malunion, nonvascularization, and donor-site morbidity are all potential complications of autologous flaps, which have not been observed with eTMJR.[9,10] A literature research conducted by Kearns et al.[11] evaluated donor-site morbidity according to patient-reported outcomes and showed that all frequently used autologous flaps, except the scapular flap, are susceptible to chronic pain, scarring, and sensory abnormalities at the donor site. Furthermore, during the early postoperative period after a free vascularized graft, surgeons often opt for intermaxillary fixation to improve the likelihood of flap healing, but this reduces total joint mobility, and thereby increased the risk of (recurrent) ankylosis. In contrast, eTMJR permits early mobilization, which has been shown to improve functional outcomes, when compared with immobilization after surgery.[12,13]
When comparing outcomes between eTMJR and autologous reconstruction, an objective measure of functionality is required. This can involve evaluating parameters such as maximal mouth opening or lateral excursion, as well as postoperative pain and dietary function. These data are readily available for alloplastic TMJ reconstruction but not for autologous reconstruction of the TMJ and mandible. Saeed et al.[13] compared 49 patients who underwent autologous treatment with a costochondral graft with 50 patients who underwent TMJR. Patients undergoing alloplastic TMJR exhibited better results for all outcomes, including dietary function, pain, and maximal mouth opening. However, it should be noted that no patient in the study had a mandibular defect other than the condylar abnormality.
One disadvantage of using eTMJR is that in Elledge M3 and M4 cases, occlusal rehabilitation would not be feasible, whereas an osseous flap would offer the possibility for root-shaped implants. Elledge M2 cases could, however, still be helped with an extended wrap around the bridge, based on root-shaped implants in the symphyseal region. Further comparative studies are necessary to determine the patient groups, for which eTMJR is most appropriate and accompanied by the highest patient satisfaction.
CONCLUSION
Obstacles during unilateral alloplastic eTMJR surgery relate to 3D rotations of the remaining mandible. Sagging of the prosthesis was noted in patients with neuromuscular deficiency, for which suspension techniques are proposed. Patients reported high satisfaction with the procedure. We suggest a treatment paradigm shift, with consideration of alloplastic eTMJR as the primary surgical approach, instead of reconstruction through microvascular osseous transplantation, in patients not requiring radiotherapy. This will avoid donor-site morbidity and lengthy reconstructive surgery while leaving autologous osseous transplantation available as a future possibility in case of implant failure. A subclassification system of eTMJR is proposed that takes into account three potential obstacles: contour corrections, occlusal adjustments, and simultaneous contralateral mandibular osteotomy.
Financial support and sponsorship
Nil.
Conflicts of interest
Professor Mommaerts is co-owner and innovation ambassador at CADskills bv, the company that designes and manufactures the patient specific implants discussed in the article.
REFERENCES
- 1.Vega LG, Meara D. Temporomandibular Joint Total Joint Replacement – J TJR. Cham: Springer; 2016. [Google Scholar]
- 2.Peckitt NS. Stereoscopic lithography: Customized titanium implants in orofacial reconstruction. A new surgical technique without flap cover. Br J Oral Maxillofac Surg. 1999;37:353–69. doi: 10.1054/bjom.1999.0070. [DOI] [PubMed] [Google Scholar]
- 3.Elledge R, Mercuri LG, Speculand B. Extended total temporomandibular joint replacements: A classification system. Br J Oral Maxillofac Surg. 2018;56:578–81. doi: 10.1016/j.bjoms.2018.06.002. [DOI] [PubMed] [Google Scholar]
- 4.Klassen AF, Cano SJ, Schwitzer JA, Scott AM, Pusic AL. FACE-Q scales for health-related quality of life, early life impact, satisfaction with outcomes, and decision to have treatment: Development and validation. Plast Reconstr Surg. 2015;135:375–86. doi: 10.1097/PRS.0000000000000895. [DOI] [PubMed] [Google Scholar]
- 5.Farzad P. Reconstruction of nongrowing hemifacial microsomia patient with custom-made unilateral temporomandibular joint total joint prosthesis and orthognathic surgery. J Oral Biol Craniofac Res. 2017;7:62–6. doi: 10.1016/j.jobcr.2016.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bredell M, Grätz K, Obwegeser J, Gujer AK. Management of the temporomandibular joint after ablative surgery. Craniomaxillofac Trauma Reconstr. 2014;7:271–9. doi: 10.1055/s-0034-1378181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Moraissi EA, El-Sharkawy TM, Mounair RM, El-Ghareeb TI. A systematic review and meta-analysis of the clinical outcomes for various surgical modalities in the management of temporomandibular joint ankylosis. Int J Oral Maxillofac Surg. 2015;44:470–82. doi: 10.1016/j.ijom.2014.10.017. [DOI] [PubMed] [Google Scholar]
- 8.Sidebottom AJ. Alloplastic or autogenous reconstruction of the TMJ. J Oral Biol Craniofac Res. 2013;3:135–9. doi: 10.1016/j.jobcr.2013.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vega LG, González-García R, Louis PJ. Reconstruction of acquired temporomandibular joint defects. Oral Maxillofac Surg Clin North Am. 2013;25:251–69. doi: 10.1016/j.coms.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 10.De Meurechy NK, Loos PJ, Mommaerts MY. Postoperative physiotherapy after open temporomandibular joint surgery: A 3-step program. J Oral Maxillofac Surg. 2019;77:932–50. doi: 10.1016/j.joms.2018.12.027. [DOI] [PubMed] [Google Scholar]
- 11.Kearns M, Ermogenous P, Myers S, Ghanem AM. Osteocutaneous flaps for head and neck reconstruction: A focused evaluation of donor site morbidity and patient reported outcome measures in different reconstruction options. Arch Plast Surg. 2018;45:495–503. doi: 10.5999/aps.2017.01592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mercuri LG. Total joint reconstruction – Autologous or alloplastic. Oral Maxillofac Surg Clin North Am. 2006;18:399–410, vii. doi: 10.1016/j.coms.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 13.Saeed N, Hensher R, McLeod N, Kent J. Reconstruction of the temporomandibular joint autogenous compared with alloplastic. Br J Oral Maxillofac Surg. 2002;40:296–9. doi: 10.1016/s0266-4356(02)00139-0. [DOI] [PubMed] [Google Scholar]