Dear Editor,
We read with great interest an article from Li et al 1 describing “The Neuroinvasive Potential of SARS‐CoV2 May Play a Role in the Respiratory Failure of COVID‐19 Patients.” Here, we describe subarachnoid hemorrhage (SAH) as a severe neurological manifestation associated with pediatric COVID‐19.
A 9‐year‐old boy presented with cardiopulmonary arrest and low Glasgow Coma Scale (GCS) and COVID‐19 symptoms, including respiratory insufficiency, fever, nausea, abdominal pain, headache, anorexia, and fatigue. He had no past medical history and close contact with a person who tested positive for COVID‐19. Reverse transcription‐polymerase chain reaction (RT‐PCR) from nasopharyngeal swab specimens confirmed positive COVID‐19. Laboratory testing (Table 1) revealed the development of nonoliguric renal failure due to a fourfold increase in creatinine. The patient blood‐type was A+. He received intravenous dopamine for low blood pressure and fresh frozen plasma (FFP) in addition to meropenem, vancomycin, azithromycin, oseltamivir, levofloxacin, lopinavir/ritonavir, and hydroxychloroquine. Chest computed tomography (CT) scan (Figure 1) was performed two times: On the first day of hospitalization, the scan exhibited consolidation at posterior basal segments of both lungs with air bronchogram sign and on the second day, it revealed a consolidation with the progression of air bronchogram and a mild right‐sided pleural effusion occurred.
Table 1.
Clinical laboratory results
| Measure | Day 1 | Day 1 | Day 2 |
|---|---|---|---|
| pH | 6.7a | 6.86 | 6.82 |
| PCO2, mm Hg | 31a | 152 | 163 |
| PO2, mm Hg | 37a | 81 | 146 |
| HCO3, mEq/L | 4.4a | 27.5 | 26 |
| BE, mmol/L | −28 | −10 | −11 |
| Urea, mg/dL | 20 | ⋯ | 100 |
| Creatinine, mg/dL | 0.5 | ⋯ | 2 |
| White blood cell count, ×103/μL | 5.3 (N: 70%, L: 25%) | ⋯ | 9.3 |
| Platelet count, ×103/μl | 133 | ⋯ | 174 |
| Mean corpuscular volume, FL | 87 | ⋯ | 82 |
| Hemoglobin, g/dL | 18.5 | ⋯ | 19 |
| Blood sugar, mg/dL | 244 | ⋯ | ⋯ |
| C‐reactive protein | +2 | ⋯ | ⋯ |
| Urine blood | 0 | 0 | 0 |
| Urine RBC | 0 | 0 | 0 |
| Hemoglobin A1c % | 5 | ⋯ | ⋯ |
On the basis of venous blood gas analysis.
Figure 1.
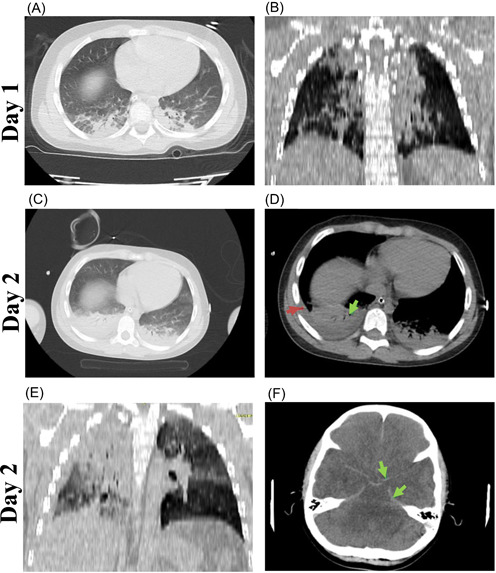
A 9‐year‐old boy presented with cardiopulmonary arrest, fever, nausea, abdominal pain, headache, anorexia, and fatigue. Day 1: A, Axial computed tomographic (CT) scan in parenchymal view showing consolidation at both posterior basal segments with air bronchogram sign. B, Coronal reconstructed CT image in parenchymal view showing consolidation in both lungs. Day 2: C, Axial CT scan in parenchymal view showing consolidation at both posterior basal segments with air bronchogram sign, which has progressed, in comparison to day 1. D, Axial CT scan in mediastinal view showing consolidation with air bronchogram sign (green arrow). Also, a mild pleural effusion at the right side (red arrow). E, Coronal reconstructed CT image in parenchymal view showing consolidation in both lungs, more prominent at right hemithorax. F, Axial CT scan of the brain showing hyperdensity at basal cisterns, interhemispheric, and bilateral Sylvian fissures in favor of subarachnoid hemorrhage, without intraventricular hemorrhage and hydrocephalus (green arrow); decreased density of white matter in favor of brain edema
Due to fixed and dilated pupils on the second day, the brain CT scan (Figure 1F) uncovered the hyperdensity at basal cisterns, interhemispheric and bilateral Sylvian fissures in favor of SAH, and reduction of white matter density in favor of brain edema. The World Federation of Neurologic Surgeons grading scale for SAH was 5. Timely follow‐up chest CT along with RT‐PCR confirmed COVID‐19 pneumonia in which pediatric pulmonary damage and hypoxemia affected multiorgan systems owing to the involvement of the lung parenchyma. Finally, he died after 2 days of hospitalization. Furthermore, there were no lesions in anatomical pathways of cerebral arteries in favor of cerebral aneurysm and no suspected parenchymal lesions observed for arteriovenous malformation. We speculate that infection as a miscellaneous cause of SAH had taken place, based on previous data that showed infection triggers SAH. 2
1. DISCUSSION
Pediatric COVID‐19 appeared with mild symptoms 3 with severe complications of COVID‐19 less frequent than adults. 4 However, the clinical course and complications related to the COVID‐19 in children are still unclear. One of the reasons is that parents show immense fear to take the children to the hospital during the coronavirus crisis.
Striking evidence exhibited that COVID‐19 impacts multiorgan system in adults, including the central nervous system (CNS) and cerebrovascular events (CVEs) including intracranial hemorrhage, has been published in association with this infection. 5 While infections have been described in relation to SAH little is known about the pediatric COVID‐19 infection. 2 Severe COVID‐19 may cause neurologic manifestations because the virus has the potential to enter the CNS through hematogenous spread or retrograde neuronal route. 6 The expression of angiotensin‐converting enzyme 2 (ACE2) as the SARS‐CoV‐2 main receptor in the brain may promote virus entry. 7 The direct route of neuroinvasion has not been established for SARS‐CoV‐2 so far but the virus or its particles were present in brain autopsy samples. 8 Aside from direct CNS infection, consequences of peripheral infection such as hyperinflammation and cytokine storm, endothelial injury, coagulopathy, and unopposed Ang II activation due to ACE2 reduction leading to vasoconstriction and hypertension are possible mechanisms for CVEs. 9 An increase in leukocyte count and elevated C‐reactive protein (CRP) in the presented case might be interpreted as activation of the immune system and inflammation that can be associated with both COVID‐19 and SAH. CRP is an inflammatory marker that has been revealed to be associated with the severity of COVID‐19. 10 A recent report of SAH in a SARS‐COV‐2‐infected adult patient linked the event with abnormal coagulation or cytokine storm. 11
Moreover, ABO blood‐type might have a prognostic role in the severity of COVID‐19. There is a positive association between ACE activity and the GATC haplotype of the ABO gene, which is prevalent in non‐O blood group. Thus, patients with blood‐type O might have protection against severe COVID‐19. 12 However, patients with blood group type A, as the patient described in this report, might be more predisposed to severe infection.
Overall, we describe a pediatric COVID‐19 case associated with nonoliguric renal injury and SAH. The presented case of pediatric COVID‐19 developing SAH, while he had no underlying neurological disease, highlights that children are at risk of severe complications of COVID‐19 and immediate medical care is required.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
REFERENCES
- 1. Li YC, Bai WZ, Hashikawa T. The neuroinvasive potential of SARS‐CoV2 may play a role in the respiratory failure of COVID‐19 patients. J Med Virol. 2020;92(6):552‐555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sebastian S, Stein LK, Dhamoon MS. Infection as a stroke trigger: associations between different organ system infection admissions and stroke subtypes. Stroke. 2019;50(8):2216‐2218. [DOI] [PubMed] [Google Scholar]
- 3. Cai J, Xu J, Lin D, et al. A case series of children with 2019 novel coronavirus infection: clinical and epidemiological features. Clin Infect Dis. 2020. 10.1093/cid/ciaa198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shekerdemian LS, Mahmood NR, Wolfe KK, et al. Characteristics and outcomes of children with coronavirus disease 2019 (COVID‐19) infection admitted to US and Canadian pediatric intensive care units. JAMA Pediatr. 2020. 10.1001/jamapediatrics.2020.1948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Reddy ST, Garg T, Shah C, et al. Cerebrovascular disease in patients with COVID‐19: a review of the literature and case series. Case Rep Neurol. 2020;12(2):199‐209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Baig AM, Khaleeq A, Ali U, Syeda H. Evidence of the COVID‐19 virus targeting the CNS: tissue distribution, host–virus interaction, and proposed neurotropic mechanisms. ACS Chem Neurosci. 2020;11(7):995‐998. [DOI] [PubMed] [Google Scholar]
- 7. Bittmann S, Luchte E, Bittmann L, Moschüring‐Alieva E, Weissenstein A, Villalon G. COVID‐19: expression of ACE2‐receptors in the brain suggest neurotropic damage. J Regen Biol Med. 2020;2(3):1‐3. [Google Scholar]
- 8. Solomon IH, Normandin E, Bhattacharyya S, et al. Neuropathological features of Covid‐19 [published online ahead of print Jun 12, 2020]. N Engl J Med. 2020. 10.1056/NEJMc2019373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Spence JD, de Freitas GR, Pettigrew LC, et al. Mechanisms of stroke in COVID‐19. Cerebrovasc Dis [Internet]. 2020. https://www.karger.com/DOI/10.1159/000509581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zeng F, Huang Y, Guo Y, et al. Association of inflammatory markers with the severity of COVID‐19: A meta‐analysis. Int J Infect Dis. 2020;96:467‐474. 10.1016/j.ijid.2020.05.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Craen A, Logan G, Ganti L. Novel coronavirus disease 2019 and subarachnoid hemorrhage: a case report. Cureus. 2020;12:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dai X. ABO blood group predisposes to COVID‐19 severity and cardiovascular diseases. Eur J Prevent Cardiol. 2020;2047487320922370:1‐2. 10.1177/2047487320922370 [DOI] [PMC free article] [PubMed] [Google Scholar]
Contributor Information
Sedigheh Basirjafari, Email: sed_basir_6886@yahoo.com.
Mohammad Zarei, zareim@email.chop.edu, Email: Biotech.zarei@gmail.com.


