Purpose:
The COVID-19 pandemic has brought unprecedented challenges for oculoplastic surgeons worldwide, in terms of care delivery, medical equipment and at-risk patient management. To date, there are no centralized or compiled international COVID-19 guidelines for oculoplastic surgeons.
Methods:
We examined COVID-19 guidelines published by oculoplastic societies worldwide. All countries around the world were initially considered in this study, but only 9 oculoplastic societies met the inclusion criteria: (1) publicly available guidelines displayed on the oculoplastic society’s website, or (2) guidelines received from the oculoplastic society after contacting them twice using the contact information on their website.
Results:
The 9 oculoplastic societies examined include: the American Society of Ophthalmic Plastic and Reconstructive Surgery, the British Oculoplastic Surgery Society, the Canadian Society of Oculoplastic Surgery, the European Society of Ophthalmic Plastic and Reconstructive Surgery, la Sociedad Española de Cirugía Plástica Ocular y Orbitaria, la Asociación Colombiana de Cirugía Plastica Ocular, the Asia Pacific Society of Ophthalmic Plastic & Reconstructive Surgery, the Oculoplastics Association of India, and the Philippine Society of Ophthalmic Plastic and Reconstructive Surgery. They all agree that urgent procedures should not be delayed, while non-necessary procedures (including all elective clinic services) should be postponed. When adequate protective equipment is available, oculoplastic surgeons must treat urgent cases. Eight out of 9 societies have provided recommendations on personal protective equipment use in order to prevent the spread of COVID-19 and to adequately protect mucous membranes. Other recommendations provided by certain societies are related to shelter in place measures, hand hygiene and surface disinfection protocols, patient triage, and thyroid eye disease management.
Conclusions:
All 9 societies with published recommendations have provided valuable recommendations to their members, regarding urgency of care and infection control solutions (personal protective equipment, hand hygiene, telemedicine, and social isolation).
Nine major oculoplastic societies have issued recommendations related to proper patient care, social distancing, and personal protective equipment use, to ensure that oculoplastic surgeons adopt the best clinical and hospital-based practices during the COVID pandemic.
Supplemental Digital Content is available in the text.
According to data compiled by the World Health Organization on May 27, 2020, the coronavirus disease 2019, also referred to as COVID-19 or SARS-CoV-2, has affected more than 5 million people and caused approximately 350,000 deaths.1 An ophthalmologist in Wuhan first warned the public about this novel severe acute respiratory virus’ emergence in December 2019, and later passed away from COVID-19.2 As the virus spread globally, the outbreak was declared a Public Health Emergency of International Concern by the World Health Organization on January 30, 2020, and since then, the pandemic has disrupted essential medical and surgical services in most specialties.3 Articles reviewing COVID-19 surgical recommendations (in general and aesthetic surgery, ophthalmology, and otolaryngology) reported that guidelines were quickly implemented without evidence-based data, which resulted in a lack of consensual framework for essential medical and surgical service management across institutions.4–7
Similar to most respiratory viruses, this seventh known human coronavirus is transmitted via large droplets. COVID-19 is particularly contagious, as it can affect asymptomatic patients, may be found in tears and stool, and has airborne spread potential.8–10 Recent studies suggest that the virus stays in the air for 3 hours and on surfaces for up to 72 hours.11 Physicians are therefore at increased risk of contracting the virus due to their close proximity to patients. In the clinic, ophthalmologists may be at even greater risk since they examine patients, face to face, at less than 20 cm with slit-lamps and even closer during direct ophthalmoscopy. Other physicians, such as critical care doctors, who regularly intubate COVID-19 patients, are also at increased risk due to the high-risk aerosolizing procedures they perform.5 As the viral load is greater in the nasal cavity than in the throat, operations involving the nasolacrimal area (lacrimal drainage system and sinuses) pose an even higher risk for oculoplastic surgeons (and otolaryngologists), compared to ophthalmologists and other physicians.5,12 (Fig. 1)
FIG. 1.
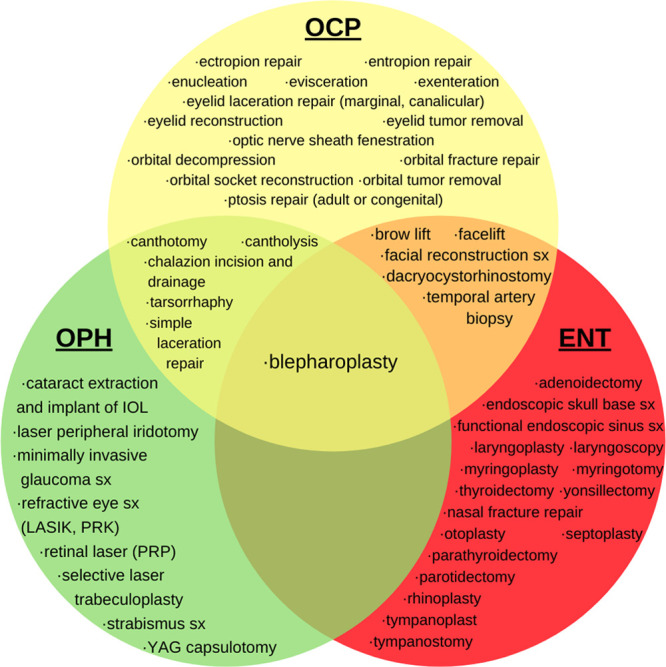
Most common surgical procedures performed in oculoplastics, ophthalmology and otolaryngology. ENT, otolaryngology; OCP, oculoplastics; OPH, ophthalmology; SX, surgery.
This article assesses guidelines provided by major international oculoplastic societies on urgency of care, patient triage, social distancing, and personal protective equipment (PPE) use when caring for oculoplastic patients during the COVID-19 pandemic. This article will help familiarize oculoplastic surgeons with the current COVID-19 guidelines worldwide to enable best medical and surgical practices based on these recommendations.
METHODS
All nations were originally considered in this study (Fig. 2 and Table 1, Supplemental Digital Content 1, available at http://links.lww.com/IOP/A233). More specifically, we searched for all 235 countries and areas included in the United Nations 2019 revision of World population prospects.13 Out of these 235 countries, 30 had a national oculoplastic society. We cross-referenced the websites associated with these national oculoplastic societies, and included 8 other oculoplastic societies covering greater regions like continents. Out of these 38 oculoplastic societies, 6 had publicly available COVID-19 guidelines, and 10 did not have information to contact the society (no website, no functional email on the website, or no functional contact portal page). We surveyed the 22 remaining societies (attempted to contact via email or the society’s contact page twice) to inquire about the status of their society’s current status concerning COVID-19 guidelines for oculoplastic surgeons (1 - recommendations available, 2 - recommendations available for members only, 3 - referral to another society’s guidelines, 4 - no recommendations available), and gave them a total of 10 days to reply to the message. Seven of these societies replied: 3 of them sent us their society’s guidelines and 4 of them indicated that they followed recommendations from other ophthalmology or oculoplastic societies.
FIG. 2.
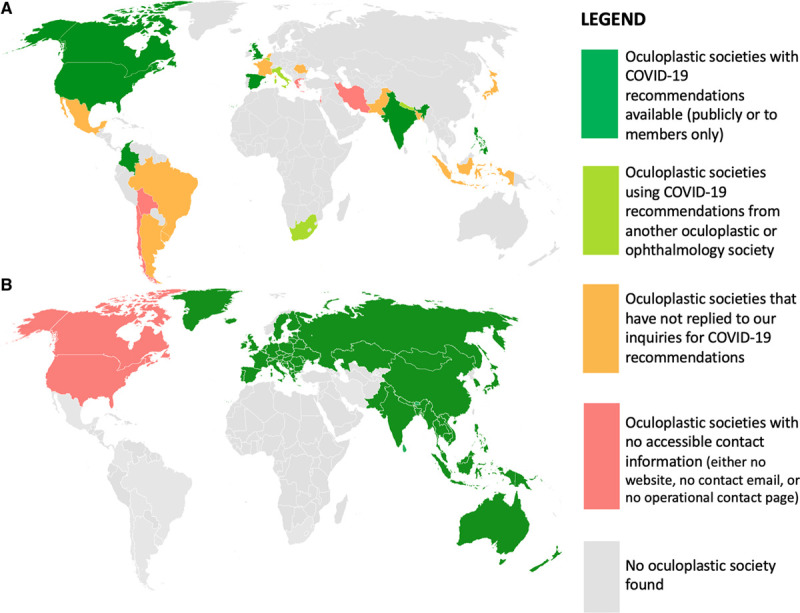
Maps of COVID-19 recommendations by available oculoplastic societies around the world. A, Per country (ex. ASOPRS). B, Per region greater than a country (ex. NASAOS).
TABLE 1.
International oculoplastic surgery societies examined
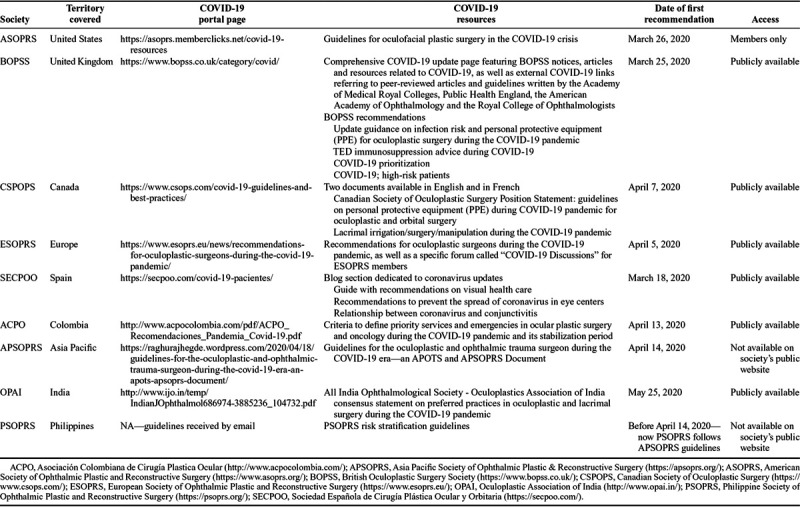
This study compares and contrasts all accessible COVID-19 recommendations from 9 major oculoplastic societies around the world (Table 1). We included COVID-19 recommendations from these oculoplastic societies: American Society of Ophthalmic Plastic and Reconstructive Surgery (ASOPRS), British Oculoplastic Surgery Society (BOPSS), Canadian Society of Oculoplastic Surgery (CSPOPS), European Society of Ophthalmic Plastic and Reconstructive Surgery (ESOPRS), Sociedad Española de Cirugía Plástica Ocular y Orbitaria (SECPOO), Asociación Colombiana de Cirugía Plastica Ocular (ACPO), Asia Pacific Society of Ophthalmic Plastic & Reconstructive Surgery (APSOPRS), Oculoplastics Association of India (OPAI), and Philippine Society of Ophthalmic Plastic and Reconstructive Surgery (PSOPRS).
The data displayed on these societies’ official websites and received by the societies were extracted, translated into English when applicable (SECPOO and ACPO) and analyzed in this study.
It is important to note that this study reflects the societies’ respective status as of May 27, 2020 and that these guidelines might be subject to change.
RESULTS
Overview of Oculoplastic Societies and COVID-19 Information.
Table 1 highlights the COVID-19 resources accessible on the 9 oculoplastic surgery societies’ websites. ASOPRS, ESOPRS, and ACPO provide 1 document with guidelines for oculoplastic surgeons. CSPOPS has 2 documents related to PPE and oculoplastic procedures. BOPSS and SECPOO have an entire section dedicated to coronavirus updates. APSOPRS, OPAI, and PSOPRS have 1 document with guidelines for their members. PSOPRS wrote their guidelines during their quarantine period, and no longer uses them as they now refer their members to the APSOPRS guidelines. Oculoplastic surgery societies have emitted their first COVID-19 guidelines from March 18 (SECPOO) to May 25, 2020 (OPAI). Guidelines differ from 1 society to another, as they take into account their respective region’s health policies. The societies also mention that the guidelines are not standard of care, as individual factors must be taken into consideration (i.e., vision status of the contralateral eye, general health, patient age).
Urgency of Care.
All 9 societies agree that urgent procedures should not be delayed, while non-necessary procedures (including all elective clinic services) should be delayed. Specific oculoplastic procedures per society are highlighted and compared in Table 2.
TABLE 2.
Comprehensive list of urgent and non-urgent procedures listed on the oculoplastic societies’ COVID-19 portal
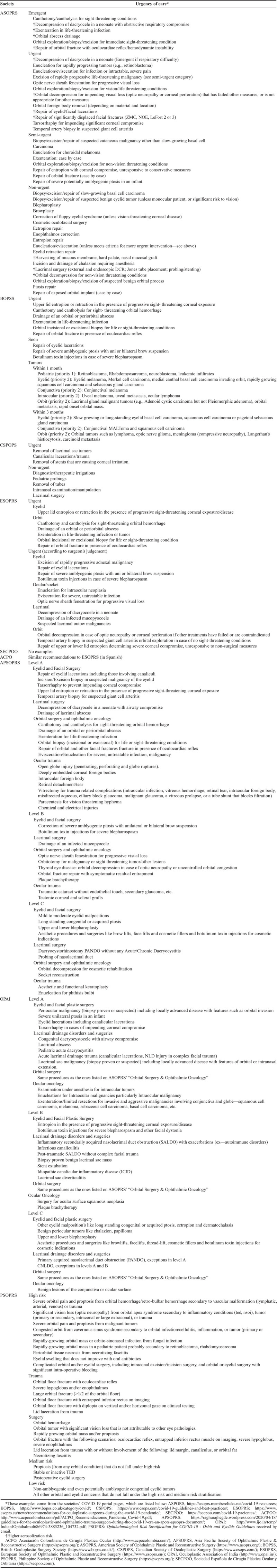
ASOPRS’ list is the most comprehensive and includes 6 emergent, 12 urgent, 6 semi-urgent, and 18 non-urgent scenarios, with 11 procedures considered at higher aerosolization risk.
BOPSS provides a few examples of urgent and less urgent situations. Its recommendation on tumor management is the most exhaustive one, as it classifies different tumors per type (pediatric, eyelid, conjunctival, intraocular, orbital), per priority (level 1: emergency operation within 72 hours, level 2: elective surgery prioritized within 4 weeks, level 3: elective surgery postponed for 10–12 weeks) and per time (within 1 month or 3 months).
As CSPOP recommends its members to follow their local guidelines, it only provides a few examples of procedures that are deemed urgent and should be performed safely, such as lacrimal sac tumor removal, canalicular trauma, and stent removal. CSPOP contrasts these surgeries with elective procedures, such as tube removal and pediatric lacrimal probings.
In order to better guide its members, ESOPRS lists 5 procedures that are urgent at all times, including 1 related to the eyelids and 4 to the orbit. ESOPRS also indicates 14 procedures (4 related to the eyelids, 3 to the eye surface, 3 to the lacrimal duct, and 4 to the orbit) that are urgent depending on the surgeon’s expert opinion.
SECPOO is the only society, out of the 9 examined, that does not provide concrete urgent and elective procedure examples.
ACPO mentions that oculoplastic surgeons have the duty to treat urgent cases, such as severe infections, trauma, tumors, and acute optic neuropathy, and then lists the same procedures as ESOPRS concerning urgent patient care.
APSOPRS provides specific guidelines on which oculoplastic procedures qualify as emergent, urgent, or elective. Specifically, they stratify procedures into level A (urgent surgery required in 4–72 hours), B (non-urgent surgery that can be delayed beyond 3–4 weeks), and C (non-urgent surgery that can be deferred beyond 3 months). They further stratify procedures into different clinical subtypes including eyelid, lacrimal, and orbital surgeries. Eyelid procedures qualifying as emergent (level A) included laceration repair (including canalicular lacerations), incisional or excisional biopsy of eyelid malignancies, tarsorrhaphy and/or lid retraction or entropion repair (in setting of significant corneal damage), and temporal artery biopsy to aid in the diagnosis of giant cell arteritis. Lacrimal procedures qualifying as emergent included lacrimal abscess drainage and dacryocystocele decompression causing airway compromise in neonates. Orbital procedures considered emergent included canthotomy and cantholysis in the setting of retrobulbar hemorrhage, orbital abscess drainage, exenteration in the setting of life-compromising infection such as mucormycosis, and orbital fracture repair (if signs of muscle entrapment with oculocardiac reflex).
OPAI also classifies procedures into similar categories of level A (emergent surgery required in 4–72 hours), B (non-urgent surgery that can be delayed up to 4 weeks), and C (non-urgent surgery that can be delayed beyond 6 weeks). Emergent orbital, eyelid, and lacrimal surgeries overlapped with all those previously described by APSOPRS above, with the addition of eyelid surgery for cases of congenital ptosis with concern for amblyopia, surgical management for pediatric acute dacryocystitis, and excision of lacrimal sac malignancies.
PSOPRS stratifies the risk associated with oculoplastic conditions into high risk (in-person consultation required), medium risk (ideally seen in clinic within 1–3 months, but acceptable to consult via telemedicine while on quarantine) and low risk (postpone clinic visit >4 months). This risk stratification plan is no longer recommended to PSOPRS members, as the society refers them to the more updated and comprehensive APSOPRS guidelines.
Shelter in Place and Telemedicine.
While all 9 oculoplastic surgery societies recommend postponing non-urgent eye examinations and procedures, only 4 societies highlight shelter in place recommendations.
Following instructions from the United Kingdom’s Chief Medical Officer and the Academy of Medical Royal Colleges, BOPSS encourages its members to proactively identify patients who are at very high morbidity and mortality risk from COVID-19 (i.e., solid organ transplant recipients, people with severe respiratory conditions, cancer and immunosuppressed patients), and send them a template letter written by the UK National Health Service urging them to self-isolate for 12 weeks.
CSPOPS mentions in the introduction of its position statement on PPE during COVID-19 that social distancing is an important public health measure to limit person-to-person transmission. SECPOO reminds all patients, via its website, that it is crucial that they stay at home and take care of themselves. ACPO also emphasizes sheltering in place and following social distancing recommendations to prevent disease spread. Furthermore, ACPO recommends that oculoplastic surgeons perform their initial patient assessment via teleconsultation, video calls, or image review and medical history summary when possible. ASOPRS, ESOPRS, APSOPRS, OPAI, and PSOPRS do not specifically mention guidelines regarding stay at home orders or telemedicine.
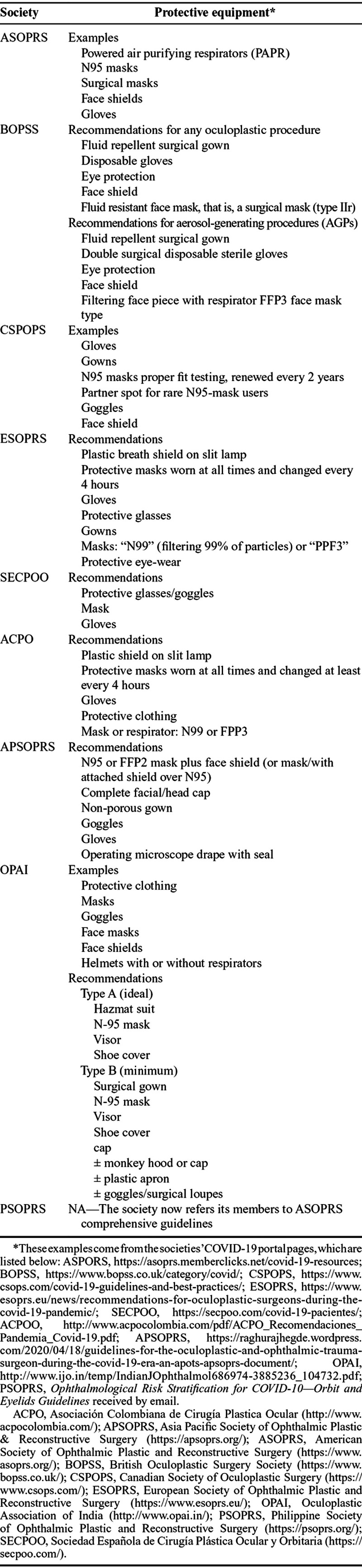
PPE Use and Engineering Controls.
When adequate protective equipment is available, oculoplastic surgeons must treat urgent cases. All societies, except PSOPRS, have therefore provided PPE use recommendations to prevent COVID-19 spread and to adequately protect mucous membranes (Table 2).
ASOPRS mentions the need for full PPE for operating room staff and provides a few PPE examples (i.e., masks, face shields, gloves).
BOPSS urges oculoplastic surgeons performing any oculoplastic procedure to use disposable gloves, eye protection, face shield, and surgical mask. BPOSS also acknowledges that certain procedures, notably aerosol-generating procedures (AGPs), pose a greater risk for surgeons. In those AGPs (i.e., lacrimal procedures, orbital surgery using power tools, open suctioning, procedures involving the nasal or sinus cavities), all people in the operating room must double glove and use a filtering face piece with respirator filtering face piece, type 3 (FFP3) face mask type. The patient must also be draped and masked, as an additional and effective barrier to exhaled air between the patient and surgeons. Furthermore, BOPSS emphasizes proper used PPE disposal as healthcare waste.
Similar to BOPSS, CSPOPS recommends appropriate PPE, especially for AGPs like lacrimal irrigation, manipulation, or surgery. Moreover, CSPOPS emphasizes the need for proper PPE fit and use to effectively protect surgeons. As the greatest self-contamination risk occurs during doffing, it also recommends its members to revise local donning and doffing instructions. While it acknowledges that most centers recommend N95 masks and that institutional recommendations must be followed, CSPOPS does mention that there is currently a lot of debate regarding airborne transmission in COVID-19. Filtering masks aiming to minimize airborne transmission are therefore precautionary measures.
Both ESOPRS and ACPO recommend plastic slit lamp breath shields, as well as protective masks worn at all times and changed every 4 hours. In addition to standard universal precautions, ESOPRS particularly recommends N99 or PPF3 mask use with protective eyewear for operating staff. ACPO makes same recommendation and highlights the distinction between those 2 masks: N99 follows the American National Institute for Occupational Safety and Health respirator certification program, while FFP3 follows the European Standard (EN 149:2001).14 National Institute for Occupational Safety and Health certification is based on oil resistances (N, not resistant to oil; R, resistant to oil; P, oil-proof): N95, R95, and P95 masks are not resistant to oil (95% filtration efficiency); N99, R99, and P99 are resistant to oil (99% filtration efficiency); N100, R100, and P100 are oil-proof masks (100% filtration efficiency). FPP masks are categorized according to their filtration efficiency: FFP1 (78% filtration efficiency), FFP2 (92% filtration efficiency), and FFP3 (98% filtration efficiency).
OPAI recommends at least minimum PPE for all oculoplastic procedures where they define minimum PPE as a surgical gown, N95, visor, shoe covers, surgical cap ± monkey hood, plastic apron, goggles, or surgical loupes. They define ideal PPE as a Hazmat suit with N95 mask, visor, and shoe covers. Use of ideal versus minimum PPE is left up to the clinician depending on the risk of the procedure to be performed and PPE availability.
APSOPRS similarly recommends the use of at least minimum PPE for all procedures, which they define as N95 or FFP2 mask, face shield, complete facial/head cap, non-porous gown, goggles, and gloves. Where available, they recommend use of FPP3 or PAPR over N95 masks.
All of them, except ACPO, refer their members to other organizations to have the most up-to-date advice regarding adequate PPE and hygiene recommendations. ASOPRS encourages its members to follow CDC and local institutional guidelines. BOPSS follows Public Health England advice and the Royal College of Ophthalmologists PPE and staff protection requirements for ophthalmology. CSPOPS recommends standard universal precautions according to their hospital protocols. ESOPRS puts forward the European Centre for Disease Prevention and Control guidance documents. SECPOO highlights the Pan-American Association of Ophthalmology webinar on PPE and safety (using gloves, masks, protective glasses; no accompanying person when possible; patients wearing masks at all times) and the American Ophthalmological Society recommendations on surface disinfection (using alcohol-based solution, cleaning metal, and plastic surfaces thoroughly, disinfecting all potentially contaminated material).
Surface Disinfection and Hand Hygiene.
CSOPRS reminds members that viral particles can survive for up to 4 days on contaminated surfaces. Full disinfection of all surfaces (i.e., doors, cranks, tables, and switches), especially between consultations, is therefore recommended by ESOPRS, SECPOO, and ACPO.
In addition to recommending frequent 20-second hand washing, SECPOO reminds patients and doctors to avoid rubbing or touching their eyes, and advises them to follow proper protocols when coughing and sneezing, which involves “covering their mouth and nose with a bent elbow or tissue when you cough or sneeze,” as well as “discard the tissue immediately.”
In addition to hand hygiene, disinfection and preparation of patients in the operating room is also of critical importance. APSOPRS and OPAI both recommend the use of povidone-iodine for disinfection in endonasal lacrimal and orbital procedures. In particular, studies have shown that 0.5% of povidone-iodine has viricidal activity against coronaviruses related to SARS-Cov-2 (article—Kirk-Bayley et al. The use of Povidone Iodine Nasal Spray and Mouthwash During the Current COVID-19 Pandemic May protect healthcare workers and reduce cross-infection).
General Surgical Recommendations.
ASOPRS recommends COVID-19 testing, in accordance with local testing guidelines, before any procedure involving a mucosal surface. BOPSS encourages surgeons to minimize dialogue and procedure length, especially in the context of APGs. Even though CSPOP considers that some AGPs are unlikely to result in viral transmission, CSPOP reminds surgeons to take extra precautions and recommends them to follow a detailed algorithm for risk stratification and PPE determination in patients potentially infected by COVID-19. ACPO strongly suggests that surgeons establish triage systems to identify patients with COVID-19 symptoms, including examination for acute conjunctivitis and travel history.
APSOPRS and OPAI provide specific recommendations on altering surgical techniques and equipment used in the operating room. For instance, they recommend avoiding the use of monopolar cautery in making skin incisions, particularly those involving mucosal surfaces, and instead using scalpels as this may decrease aerosolization of viral particles. Similarly, they recommend avoiding use of high-powered drills during osteotomies whenever possible which may also increase aerosolization risk. Avoidance of prolonged or excessive irrigation and suctioning of tissues, particularly mucosal tissues, is also advised against by both societies.
Other Recommendations.
BOPSS is the only society that provides detailed advice concerning thyroid eye disease patient management during COVID-19. Intravenous steroids must not be given to moderate to severe thyroid eye disease patients during the COVID pandemic because they will be immunosuppressed, but each individual case must be dealt with individually and at the discretion of the physician.
DISCUSSION
Oculoplastic surgeons are at particularly high-risk for transmission of COVID-19 given the specific procedures they perform. Similarly, physicians performing procedures on the head and neck such as otolaryngologists, oral maxillofacial surgeons, facial plastics surgeons, and neurosurgeons are also at high-risk. The field of oculoplastic surgery focuses on the eyelids, orbit, ocular adnexa, and nasolacrimal duct system. Given the fact that oculoplastic surgeons operate on the nasolacrimal region as well as the orbit and sinuses, they are at risk for aerosolization of viral particles from nasal mucosa and/or other mucosal surfaces. Common oculoplastic examination techniques and procedures are now being deferred or reconsidered given the COVID-19 pandemic.
Oculoplastic surgeons regularly perform examination techniques such as probing and irrigation of the nasolacrimal duct system to assess for the etiology of epiphora with subsequent correction by either external or endoscopic dacryocystorhinostomy. Such procedures including in-office probing and/or removal of lacrimal stents are now being deferred in some countries due to concern for aerosolization of viral particles from the nasal mucosa which has been found to have a high viral load. For similar reasons, use of drilling devices in orbital cases requiring osteotomy has also been discouraged in some countries. Use of scalpels for skin incisions has similarly been recommended over monopolar cautery, particularly those involving the mucosa.
While some high-risk oculoplastic procedures are non-emergent and easily postponed, many surgeries within the field are still considered emergent and necessary amidst the current pandemic. In particular, the oculoplastic surgeon frequently encounters life and vision-threatening conditions requiring surgical intervention including but not limited to removal of eyelid and orbital malignancies, repair of traumatic injuries, and drainage or debridement of eyelid and/or orbital infections such as necrotizing fasciitis, mucormycosis, and invasive fungal sinusitis. It is thus of the utmost importance that oculoplastic surgeons have a centralized resource including recommendations from major oculoplastic societies across the world in order to understand all evidence-based recommendations regarding patient care during the COVID-19 pandemic.
ASOPRS, BOPSS, CSPOPS, ESOPRS, ACPO, APSOPRS, OPAI, and PSOPRS have all provided urgent and non-urgent care examples for oculoplastic surgeons during the COVID-19 pandemic. ASOPRS provides the most detailed information, as it is the only society that classifies oculoplastic procedures into 4 distinct categories: emergent (life or sight-threatening conditions requiring treatment within 24 hours), urgent (treatment within 1 week), semi-urgent (within 8 weeks), and non-urgent procedures that can be performed once COVID-19 transmission risks are reduced (Table 2).
Eight out of 9 societies recommend control solution implementation, pertaining to 4 out of 5 steps in the National Institute for Occupational Safety and Health’s hierarchy of controls (Fig. 3). Indeed, all societies except PSOPRS recommended a few of these common measures: PPE, administrative controls (telemedicine, hand hygiene), engineering controls (physical barriers), and elimination (physical isolation).
FIG. 3.
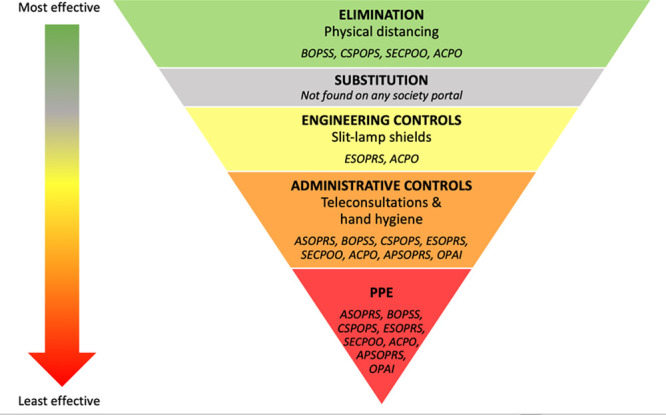
Infection control hierarchy, with examples of measures recommended by major oculoplastic societies during the COVID-19 pandemic, adapted from NIOSH (https://www.cdc.gov/niosh/topics/hierarchy/default.html).
Even though PPE is shown to be the least effective measure in infection control, most societies have specific recommendations concerning adequate PPE use to protect healthcare workers. While ASOPRS and CSPOPS only provide a few commonly used PPE examples, other societies make direct recommendations to their members. Notably, BOPSS distinguishes AGPs (higher risk, requiring respirator face mask and double gloves) from other oculoplastic procedures.
All societies, except ASOPRS and PSOPRS, remind their members about the importance of surface disinfection and meticulous hand hygiene to prevent the spread of the SARS-CoV-2 (Table 3).
TABLE 3.
Summary of protective equipment recommendations for oculoplastic surgeons during the COVID-19 pandemic
ESOPRS and ACPO are the only 2 societies that recommend physical barriers like plastic slit lamp shields.
Four societies (BOPSS, CSPOPS, SECPOO, ACPO) briefly recommend social isolation measures.
These 9 major oculoplastic societies do not provide data regarding the number of operations postponed nor recommendations regarding post-pandemic assessment and planning.
CONCLUSIONS
Major oculoplastic societies have provided COVID-19 specific guidelines to help their members make adequate decisions regarding patient care, PPE use, telemedicine, social isolation, and priority-setting during this global pandemic. As oculoplastic surgeons are at high risk of contracting COVID-19 infection, it is imperative that they follow best practices based on recommendations from health authorities. This comprehensive overview of the main recommendations by 9 major oculoplastic societies (ASOPRS, BOPSS, CSPOPS, ESOPRS, SECPOO, ACPO, APSOPRS, OPAI, and PSOPRS) will facilitate the difficult choices faced by oculoplastic surgeons to overcome challenges in caring for patients during the COVID-19 pandemic. Knowledge of current COVID-19 guidelines will allow oculoplastic surgeons to follow the best medical and surgical practices recommended.
Supplementary Material
Footnotes
The authors have no financial or conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (www.op-rs.com).
REFERENCES
- 1.The World Health Organization. Coronavirus disease: Situation report – 128. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200527-covid-19-sitrep-128.pdf?sfvrsn=11720c0a_2. Accessed May 27, 2020.
- 2.Hu K, Patel J, Patel BC. Ophthalmic manifestations of coronavirus (COVID-19). Statpearls. 2020Treasure Island (FL): StatPearls Publishing LLC. [PubMed] [Google Scholar]
- 3.Davidson H. First COVID-19 Case Happened in November, China Government Records Show - Report. 2020London, England: The Guardian; [Google Scholar]
- 4.Soreide K, Hallet J, Matthews JB, et al. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services [published online ahead of print, 2020 Apr 30]. Br J Surg. 2020 doi: 10.1002/bjs.11670. doi:10.1002/bjs.11670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vukkadala N, Qian ZJ, Holsinger FC, et al. COVID-19 and the otolaryngologist: Preliminary evidence-based review [published online ahead of print, 2020 Mar 26]. Laryngoscope. 2020 doi: 10.1002/lary.28672. doi:10.1002/lary.28672. [DOI] [PubMed] [Google Scholar]
- 6.Al-Benna S. Availability of COVID-19 Information from National and International Aesthetic Surgery Society websites. Aesthetic Plast Surg 2020;44:1043–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Olivia Li JP, Shantha J, Wong TY, et al. Preparedness among ophthalmologists: during and beyond the COVID-19 Pandemic. Ophthalmology 2020;127:569–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wong SH, Lui RN, Sung JJ. COVID-19 and the digestive system. J Gastroenterol Hepatol 2020;35:744–8. [DOI] [PubMed] [Google Scholar]
- 9.Seah IYJ, Anderson DE, Kang AEZ, et al. Assessing viral shedding and infectivity of tears in coronavirus disease 2019 (COVID-19) patients. Ophthalmology. 2020;127(7):977–979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xia J, Tong J, Liu M, et al. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol 2020; 92(6):589–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl J Med 2020;382:1564–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. World Health Organization. Modes of transmission of virus causing COVID-19: Implications for IPC precaution recommendations. Available at: https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations. 2020. Accessed 2020.
- 13.The United Nations. The 2020 revision of world population prospects. Available at: https://population.un.org/wpp/Download/Standard/Population/. 2019. Accessed May 27, 2020.
- 14.Lee SA, Hwang DC, Li HY, et al. Particle size-selective assessment of protection of European standard FFP respirators and surgical masks against particles-tested with human subjects. J Healthc Eng 2016;2016;8572493. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


