Abstract
Background
Intolerance of uncertainty—the tendency to overestimate the chance of and be unwilling to accept potential, but unlikely, negative outcomes in uncertain situations—is a cognitive construct that has been shown to affect symptoms and limitations for patients with traumatic and nontraumatic upper-extremity conditions. Cognitive flexibility and tolerance of uncertainty can be trained and practiced, with the potential to increase musculoskeletal health. However, to our knowledge, the degree to which intolerance of uncertainty might be associated with symptom intensity and the magnitude of limitations in adults with upper-extremity problems has not been characterized.
Questions/purposes
After accounting for personal and social factors, is intolerance of uncertainty independently associated with (1) the magnitude of physical limitations and (2) pain intensity?
Methods
In this cross-sectional, observational study, 139 new and returning patients presenting to one of four orthopaedic offices in a large urban area completed the Intolerance of Uncertainty Scale (a validated measure of the level of comfort with uncertain situations), the Patient-reported Outcomes Measurement Information System—Physical Function Upper Extremity computer adaptive test (to measure the magnitude of limitations), and an 11-point ordinal measure of pain intensity. The mean age of the 139 participants was 51 years ± 16 years and 55% (76 of 139) were men. Participants presented to the clinics with a wide variety of upper-extremity conditions, such as trigger finger, distal radius fractures, lateral epicondylitis, or non-specific shoulder pain. We also assessed sex, race, marital status, education level, income, public versus private insurance, area deprivation index, and the participant’s self-perception of their healthcare experience through a multiple-choice question (answer choices: none, some, a little, and a lot of experience). The following patient characteristics were more common in our study participants: white, employed, part of a married or unmarried couple, and private insurance coverage. We created two multivariable linear regression models to assess factors independently associated with the magnitude of limitations and pain intensity.
Results
After controlling for potentially confounding variables including sex, insurance, area deprivation index, and type of visit, we found that fewer physical limitations were associated with a greater intolerance of uncertainty (regression coefficient [β] -0.30; 95% confidence interval, -0.50 to -0.10; p = 0.003; semi-partial r2 = 0.07; adjusted r2 for the full model = 0.16), as was being a man (β 3.2; 95% CI, 0.08-6.3; p = 0.045; semi-partial r2 = 0.03) and having private insurance coverage (β 5.2; 95% CI, 2.1-8.2; p = 0.001; semi-partial r2 = 0.08). After controlling for one important potentially confounding variable, the level of education, greater pain intensity was associated with a greater intolerance of uncertainty (β 0.08; 95% CI, 0.02-0.14; p = 0.009; semi-partial r2 = 0.05; adjusted r2 for the full model = 0.08).
Conclusions
Intolerance of uncertainty—a byproduct of cognitive bias and error, which are elements of the normal functioning of the human mind—increases limitations and pain intensity across diagnoses, independent of demographic and social factors. Future studies can address the effect of strategies that incorporate mindset training (for example, cognitive behavioral therapy and its derivatives) on musculoskeletal symptoms and limitations.
Level of Evidence
Level II, prognostic study.
Introduction
Psychological distress (for example, the symptoms of anxiety and depression) and the effectiveness of coping strategies (such as less-catastrophic thinking and greater self-efficacy) seem to account for more of the variation in symptom intensity and magnitude of limitations than variations in pathophysiology, and these findings are consistent for several musculoskeletal problems and anatomic regions [27-29]. Cognitive fusion—the tendency to view thoughts and emotions as reality instead of merely cognitive events—is connected to pain intensity and the magnitude of limitations, particularly in people with persistent pain [34, 41-43]. Cognitive fusion is believed to be the basis for symptoms of depression and anxiety and less-effective cognitive coping strategies such as catastrophic thinking [11, 29].
Intolerance of uncertainty—the tendency to overestimate the chance of and be unwilling to accept potential, but unlikely, negative outcomes in uncertain situations—is a cognitive construct similar to cognitive fusion. Intolerance of uncertainty is also related to symptoms and limitations. Prior investigations have found high levels of intolerance of uncertainty in patients with generalized anxiety disorder [15, 40]. These high levels were also found in people with obsessive-compulsive disorder, social phobia, posttraumatic stress disorder, major depressive disorders, eating disorders, and psychosis [5, 6, 8, 11, 17, 23, 26, 35, 36, 39, 40, 44]. Lower intolerance of uncertainty correlates with health anxiety, greater magnitude of limitations, and greater intensity of pain [4, 16]. Training and practice in more-effective cognitive coping strategies through interventions such as cognitive behavioral therapy may limit symptoms and limitations [20, 37]. This warrants additional investigation into the relationship between uncertainty and physical symptoms and limitations to develop targeted interventions that will help people become and stay healthy.
Cognitive behavioral therapy-based interventions for heterogeneous anxiety and depressive disorders decrease intolerance of uncertainty and the symptoms of anxiety and depression [7]. Individuals with a greater intolerance of uncertainty have greater health anxiety and increased threat perception, and feel less in control [2, 13, 14, 19, 24, 25, 32, 38]. Intolerance of uncertainty may help explain patients’ health experiences, particularly those involving mental health [2]. A prior study of patients’ upper-extremity musculoskeletal problems found that intolerance of uncertainty was responsible for part of the effect of pain anxiety on pain intensity and physical function [16]. In this study, we addressed whether this relationship was independent of demographic and social factors. Social situations with certain levels of uncertainty (such as financial, housing, or job stress) may accustom an individual to uncertainty in health or illness.
Specifically, we asked, after accounting for personal and social factors, is intolerance of uncertainty independently associated with (1) the magnitude of physical limitations and (2) pain intensity?
Patients and Methods
Study Design
After institutional review board approval of this cross-sectional, observational study, we prospectively enrolled 139 patients during a 1-month period, between May 16, 2018 and June 22, 2018. Patients were evaluated by one of six surgeons at four orthopaedic surgery offices in a large urban area. We included all new and returning English-speaking patients with an upper-extremity problem aged between 18 and 89 years. We excluded patients who could not read or speak English fluently and those who could not provide informed consent. Research assistants, who were not involved in treatment, described the study to eligible patients before or after the visit with the surgeon. All patients who were invited agreed to participate. We were granted a waiver of documentation of informed consent, and completion of the surveys by the patient indicated informed consent.
Measurements
Patients were asked to complete a set of questionnaires in the following order: (1) the Intolerance of Uncertainty Scale—short form (IUS-12); (2) Patient-reported Outcomes Measurement Information System—Physical Function Upper Extremity (PROMIS PF UE) computerized adaptive test; (3) pain intensity as measured with an 11-point ordinal rating scale; and (4) a demographic illness questionnaire consisting of age, sex, race or ethnicity, level of education, work status, marital status, insurance, annual household income, residential ZIP code, type of visit, and experience receiving health care.
The IUS-12, a 12-item questionnaire, was used to measure intolerance of uncertainty [12]. It is a shortened version of and strongly correlates with the original 27-item questionnaire [9]. Items are rated on a five-point Likert scale ranging from 1 (“not at all characteristic of me”) to 5 (“entirely characteristic of me”). The total score is the sum of all item scores (5-60), with higher scores representing higher intolerance of uncertainty, ambiguous situations, and the future [12].
The PROMIS PF UE was used to measure upper-extremity disability, and higher scores indicate better physical function [30, 31].
The 2000 area deprivation index (ADI) and ZIP code provided by each participant was used to calculate the ADI score [22]. The ADI score is a geographic area-based measure of the socioeconomic deprivation experienced by a neighborhood [22]. The index was constructed by considering 21 socioeconomic indicators that approximate the material and social conditions and relative socioeconomic disadvantage in a community [33]. The ADI database set has a mean of 100 and standard deviation of 20, with higher scores indicating areas with lower incomes, less education, underemployment, and other factors. ADI is derived from the nine-digit ZIP code [22]. Social deprivation may accustom individuals to varying levels of uncertainty. We were only able to collect five-digit ZIP codes. Although less accurate, we decided to average all nine-digit ZIP code ADI scores that fit in each five-digit ZIP code to determine an ADI score corresponding with the various five-digit ZIP codes.
After participants completed the questionnaires, the surgeon filled in the diagnosis (see Appendix, Supplemental Digital Content 1, http://links.lww.com/CORR/A255). All questionnaires were completed by the patient before their visits with the surgeon on an encrypted tablet via a Health Insurance Portability and Accountability Act-compliant electronic platform: Research Electronic Data Capture, a secure internet-based application for building and managing online surveys and databases [21].
Study Population
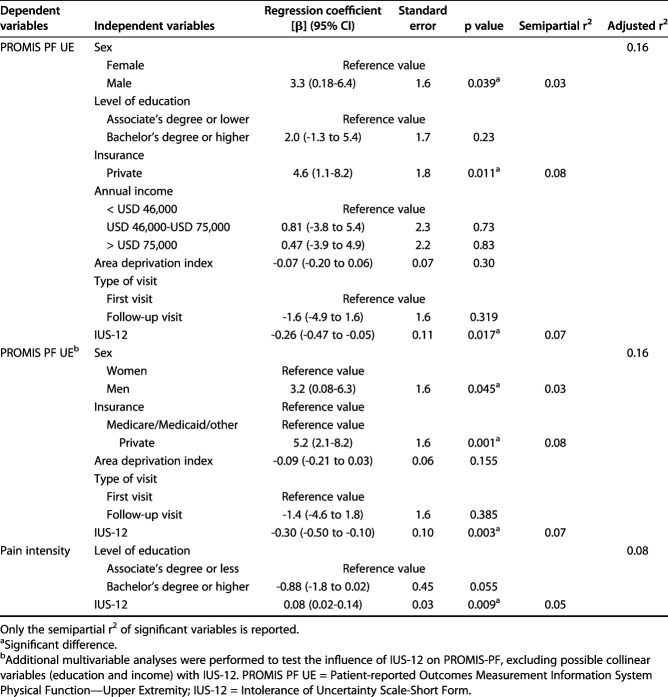
No patients were excluded from the analysis. The mean age of the 139 patients was 51 years ± 16 years and 55% (76 of 139) were men (Table 1). Forty-five percent of the patients (62 of 129) believed they had substantial healthcare experience (a lot). We enrolled patients at multiple offices in the large urban area to diversify the participant population. The mean scores were 27 ± 7.6 for the IUS-12, 43 ± 9.6 for the PROMIS PF UE, and 4.2 ± 2.7 for pain intensity.
Table 1.
Patient and clinical characteristics
Statistical Analysis
The distributions of continuous variables and assumptions concerning normality were assessed to determine the appropriateness of the statistical tests. Continuous variables are presented as the mean ± SD and discrete data are presented as proportions. We used Pearson’s correlation tests for the relationships between continuous variables, ANOVA for categorical variables, and t-tests to assess differences between continuous variables. We created two multivariable linear regression models to assess whether patient demographics (sex, level of education, insurance, annual income, ADI score, type of visit, or intolerance of uncertainty) were independently associated with PROMIS PF UE scores and pain intensity. We included all variables with p < 0.10 in the bivariate analysis in the final models (see Appendix, Supplemental Digital Content 2, http://links.lww.com/CORR/A256). All variance inflation factors were less than 2.3, indicating no collinearity. Although the variance inflation factors were all below 10 in the multivariable analysis, we tested the association between IUS-12 and other variables (not in tables) to look for a possible correlation. We found associations between the IUS-12 and education and income. Therefore, we added a third multivariable analysis excluding those variables to see whether the coefficient of IUS-12 would change. The regression coefficient (β) indicates the change in the value of a dependent variable corresponding to the unit change in the independent variable. The higher the absolute value of the coefficient, the stronger the effect of the relationship. There were no fixed cutoff scores. The adjusted r2 indicates the amount of variability in the dependent variable the model accounts for. The semi-partial r2 expresses the specific variability of a given independent variable in the model. We considered p values < 0.05 to be significant. An a priori power analysis indicated that a minimum sample of 136 participants would provide 80% statistical power (with alpha set at 0.05 for a regression with five predictors) if intolerance of uncertainty would account for 5% or more of the variability in physical function and our complete model would account for 15% of the overall variability. To account for 2% incomplete responses, we enrolled 139 patients.
Results
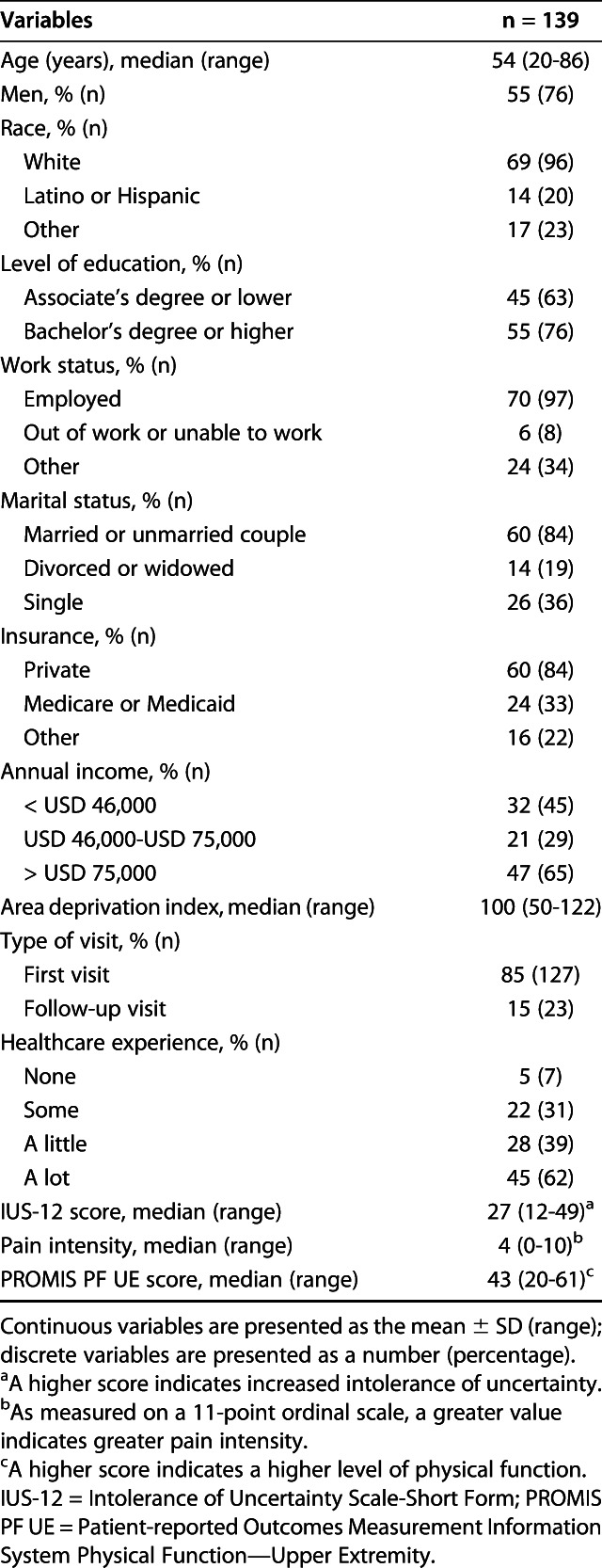
As intolerance of uncertainty increased, physical function decreased slightly (r = -0.26; p = 0.017) (see Appendix, Supplemental Digital Content 2, http://links.lww.com/CORR/A256). After controlling for potentially confounding variables including sex, insurance, ADI, and type of visit, we found that greater intolerance of uncertainty, indicated by higher IUS-12 scores, was independently associated with better physical function (measured with the PROMIS PF UE) (regression coefficient [β] -0.26; 95% confidence interval, -0.47 to -0.05; p = 0.017; semi-partial r2 = 0.04; adjusted r2 for the full model = 0.16) (Table 2). This means that for every one-point increase in intolerance of uncertainty (IUS-12 score), there was a 0.26-point decrease in physical function (PROMIS PF UE score), which means that a 38-point increase in intolerance of uncertainty would result in a single SD decrease in the PROMIS PF UE score (10 points). In this same model, we also found that better physical function was independently associated with being a man (β 3.3; 95% CI, 0.18-6.4; p = 0.039; semi-partial r2 = 0.03), as was having private insurance (β 4.6; 95% CI, 1.1-8.2; p = 0.011; semi-partial r2 = 0.04). In our tertiary analysis, excluding possible collinear variables (education and income) with the IUS-12, we found a change in the regression coefficient of IUS-12 from -0.26 to -0.30 (Table 2). In this model, lower intolerance of uncertainty was independently associated with better physical function (β -0.30; 95% CI, -0.50 to -0.10; p = 0.003; semi-partial r2 = 0.07; adjusted r2 for the full model = 0.16), being a man (β 3.2; 95% CI, 0.08-6.3; p = 0.045; semi-partial r2 = 0.03), and having private insurance (β 5.2; 95% CI, 2.1-8.2; p = 0.001; semi-partial r2 = 0.08).
Table 2.
Multivariable linear regression analysis of factors independently associated with PROMIS PF and pain intensity
As intolerance of uncertainty increased, pain intensity increased slightly (r = 0.08; p = 0.009). After controlling for a potentially confounding variable, the level of education, we found that greater intolerance of uncertainty was independently associated with greater pain intensity (measured with an 11-point ordinal rating scale) (β 0.08; 95% CI, 0.02-0.14; p = 0.009; semi-partial r2 = 0.05; adjusted r2 for the full model = 0.08) (Table 2). This means that for every one-point increase in intolerance of uncertainty (IUS-12 score), there was a 0.08-point increase in pain intensity (11-point ordinal scale), with a minimal clinically important difference of 1 to 2 points, depending on the context [1].
Discussion
People with intolerance of uncertainty tend to have distressful emotions, thoughts, and behaviors in response to uncertain events and situations [7, 10]. This study assessed the correlations of intolerance of uncertainty with the magnitude of limitations and pain intensity in adults with upper-extremity conditions, both directly and accounting for other demographic or social factors such as patient sex, age, and level of education. The finding that intolerance of uncertainty leads to greater symptoms and limitations suggests that efforts to improve psychological flexibility could be further investigated for their potential to enhance musculoskeletal health.
There are some limitations to this study. First, our decision to average the nine-digit ZIP code ADI scores in each five-digit ZIP code might not sufficiently account for variations in deprivation in a relatively large area. Future studies could use the newly released 2013 ADI dataset and nine-digit ZIP codes (not available for use when we initiated our study) for more-accurate comparisons between socioeconomic deprivation and clinical outcomes. Second, data were collected from English-speaking patients in one urban area. Despite attempts to enroll patients from various offices in the large urban area, most participants were white or employed, had private insurance coverage, and were part of a married or unmarried couple, which might limit the generalizability of our results to other populations with different demographic distributions. Despite our attempts to minimize bias and approach every patient during the period of enrollment, and even though all agreed to participate, our resulting population was not very diverse. It may be worthwhile to repeat this study but include non-English-speaking participants and a larger number of participants with a lower socioeconomic status, and even collect nine-digit ZIP codes to account for variations in ADI scores or deprivation. Third, the inclusivity of the study with a range of diagnoses, typical of people seeing an upper-extremity specialist, has advantages and disadvantages. It represents daily practice, but there may be varied findings relating to intolerance of uncertainty to physical function or pain by specific diagnosis.
We found that greater intolerance of uncertainty was associated with a greater magnitude of upper extremity-specific limitations, independently of other factors. This finding is consistent with a previous study of patients with upper-extremity conditions finding that anxiety in response to nociception (pain anxiety) mediates (explains the process underlying) the relationship between pain intensity and physical limitations [16]. This prior study also found that intolerance of uncertainty moderates or conditionally determines whether this mediation occurs [16]. The finding that private insurance was independently associated with better physical function likely reflects a better socioeconomic status, which often entails having a meaningful position in society by virtue of employment. This line of evidence establishes that the notable variation in symptom intensity and magnitude of variation for a given nociception (pathophysiology) is, in part, accounted for by one’s cognitive experience. The possibility that maladaptive cognitive experiences such as intolerance of uncertainty and psychological distress (for example, pain anxiety) are alleviated by mindset training (such as cognitive behavioral therapy and its derivatives) expands important treatment options for people with musculoskeletal illness.
We also found that greater intolerance of uncertainty was associated with greater pain intensity. The combined evidence of our study and a prior study confirms that intolerance of uncertainty has an indirect or direct effect on pain intensity and the magnitude of limitations [16]. Another study exploring the impact of intolerance of uncertainty in healthy adults on pain intensity found that intolerance of uncertainty was moderately correlated with pain intensity in response to transcutaneous electrical stimulations and was associated with worsened subjective pain [3]. Identification of intolerance of uncertainty early during treatment might help limit the transition from acute to persistent pain, especially given the uncertainty inherent in most orthopaedic illnesses [16]. A study examining the relationship between intolerance of uncertainty and opioid use found that individuals with opioid dependence exhibit higher levels of intolerance of uncertainty than people who do not regularly use opioids [18]. The weight of evidence to date indicates there is merit in investigating the prevalence of intolerance of uncertainty in patients with orthopaedic conditions and the effectiveness of treatment strategies that can help people be more comfortable with uncertainty. These findings can then be used as evidence to warrant interventions that address cognitive coping strategies in patients.
Our results and evidence to date suggest that in a variety of traumatic and nontraumatic orthopaedic conditions, intolerance of uncertainty affects symptom intensity and the magnitude of disability, independent of demographic and social factors [16]. Ultimately, clinicians should help patients share their concerns, particularly regarding uncertain aspects of their illness, and work with patients to manage and increase their comfort with uncertainty, which is inherent in sickness and even health. Intolerance of uncertainty can be quantified using the IUS-12, which our study found to be a useful measure for people with upper-extremity conditions. Clinicians could also identify intolerance of uncertainty in the form of verbal and non-verbal indicators. When substantial uncertainty is identified, the surgeon can reflect it back to the patient to forward the discussion: “The uncertainty about how this will turn out seems to be uncomfortable for you.” In this way, patients are prompted to consider and then communicate their feelings by agreeing or disagreeing with this statement. The surgeon can normalize this discomfort as a part of the illness and indicate that developing tolerance to this uncertainty can help the patient feel better and improve their experience. People who show insight (agree that they are uncomfortable with uncertainty) and express interest in working to increase their tolerance of this uncertainty can be offered support. This may be in the form of workbooks, websites or applications, or formal cognitive behavioral therapy and related approaches [16]. Surgeons should be patient with this development of insight, working to develop a trusting relationship and being incremental (distributing this effort and care over the course of multiple visits) in their care strategy. An important aspect of this strategy is resisting the pressure to order tests and treatments that are unlikely to address pathophysiology in a useful way, and risk reinforcing maladaptive cognitive coping strategies or false hope. The results of this study substantiate the need for providers to offer support to their patients that directly addresses psychological distress and the less-effective coping strategies patients may use to manage their intolerance of uncertainty.
Acknowledgements
None.
Footnotes
Each author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Dell Medical School, the University of Texas, Austin TX, USA.
References
- 1.AbilityLab. Numeric pain rating scale. Available at: https://www.sralab.org/rehabilitation-measures/numeric-pain-rating-scale. Accessed October 17, 2019.
- 2.Alschuler KN, Beier ML. Intolerance of uncertainty: shaping an agenda for research on coping with multiple sclerosis. Int J MS Care. 2015;17:153-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Belanger C, Blais Morin B, Brousseau A, Gagne N, Tremblay A, Daigle K, Goffaux P, Leonard G. Unpredictable pain timings lead to greater pain when people are highly intolerant of uncertainty. Scand J Pain. 2017;17:367-372. [DOI] [PubMed] [Google Scholar]
- 4.Blackburn J, Fischerauer SF, Talaei-Khoei M, Chen NC, Oh LS, Vranceanu AM. What are the implications of excessive internet searches for medical information by orthopaedic patients? Clin Orthop Relat Res. 2019:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boelen P. Intolerance of uncertainty and emotional distress following the death of a loved one. Anxiety Stress Coping. 2010;23:471-478. [DOI] [PubMed] [Google Scholar]
- 6.Boelen PA, Reijntjes A. Intolerance of uncertainty and social anxiety. J Anxiety Disord. 2009;23:130-135. [DOI] [PubMed] [Google Scholar]
- 7.Boswell JF, Thompson-Hollands J, Farchione TJ, Barlow DH. Intolerance of uncertainty: a common factor in the treatment of emotional disorders. J Clin Psychol. 2013;69:630-645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Broome MR, Johns LC, Valli I, Woolley JB, Tabraham P, Brett C, Valmaggia L, Peters E, Garety PA, McGuire PK. Delusion formation and reasoning biases in those at clinical high risk for psychosis. Br J Psychiatry Suppl. 2007;51:s38-42. [DOI] [PubMed] [Google Scholar]
- 9.Buhr K, Dugas MJ. The Intolerance of Uncertainty Scale: psychometric properties of the English version. Behav Res Ther. 2002;40:931-945. [DOI] [PubMed] [Google Scholar]
- 10.Buhr K, Dugas MJ. The role of fear of anxiety and intolerance of uncertainty in worry: an experimental manipulation. Behav Res Ther. 2009;47:215-223. [DOI] [PubMed] [Google Scholar]
- 11.Butzer B, Kuiper NA. Relationships between the frequency of social comparisons and self-concept clarity, intolerance of uncertainty, anxiety, and depression. Personality and Individual Differences. 2006;41:167-176. [Google Scholar]
- 12.Carleton RN, Norton MA, Asmundson GJ. Fearing the unknown: a short version of the Intolerance of Uncertainty Scale. J Anxiety Disord. 2007;21:105-117. [DOI] [PubMed] [Google Scholar]
- 13.Costa-Requena G, Rodriguez A, Fernandez R, Palomera E, Gil FL. Cognitive processing variables in breast cancer: worry and distress at the end of treatment. J Cancer Educ. 2011;26:375-379. [DOI] [PubMed] [Google Scholar]
- 14.Coutu MF, Durand MJ, Marchand A, Labrecque ME, Berbiche D, Cadieux G. Factors associated with generalized anxiety in workers undergoing work rehabilitation for persistent musculoskeletal pain. Disabil Rehabil. 2013;35:1599-1607. [DOI] [PubMed] [Google Scholar]
- 15.Dugas MJ, Gagnon F, Ladouceur R, Freeston MH. Generalized anxiety disorder: a preliminary test of a conceptual model. Behav Res Ther. 1998;36:215-226. [DOI] [PubMed] [Google Scholar]
- 16.Fischerauer SF, Talaei-Khoei M, Vissers FL, Chen N, Vranceanu AM. Pain anxiety differentially mediates the association of pain intensity with function depending on level of intolerance of uncertainty. J Psychiatr Res. 2018;97:30-37. [DOI] [PubMed] [Google Scholar]
- 17.Frank GK, Roblek T, Shott ME, Jappe LM, Rollin MD, Hagman JO, Pryor T. Heightened fear of uncertainty in anorexia and bulimia nervosa. Int J Eat Disord. 2012;45:227-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garami J, Haber P, Myers CE, Allen MT, Misiak B, Frydecka D, Moustafa AA. Intolerance of uncertainty in opioid dependency - relationship with trait anxiety and impulsivity. PLoS One. 2017;12:e0181955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gerolimatos LA, Edelstein BA. Predictors of health anxiety among older and young adults. Int Psychogeriatr. 2012;24:1998-2008. [DOI] [PubMed] [Google Scholar]
- 20.Han PK, Klein WM, Arora NK. Varieties of uncertainty in health care: a conceptual taxonomy. Med Decis Making. 2011;31:828-838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Area HIPxChange. Deprivation Index Datasets. Available at: https://www.hipxchange.org/ADI. Accessed April 26, 2019.
- 23.Holaway RM, Heimberg RG, Coles ME. A comparison of intolerance of uncertainty in analogue obsessive-compulsive disorder and generalized anxiety disorder. J Anxiety Disord. 2006;20:158-174. [DOI] [PubMed] [Google Scholar]
- 24.Kirby SE, Yardley L. Cognitions associated with anxiety in Meniere's disease. J Psychosom Res. 2009;66:111-118. [DOI] [PubMed] [Google Scholar]
- 25.Kirby SE, Yardley L. The contribution of symptoms of posttraumatic stress disorder, health anxiety and intolerance of uncertainty to distress in Meniere's disease. J Nerv Ment Dis. 2009;197:324-329. [DOI] [PubMed] [Google Scholar]
- 26.Lind C, Boschen MJ. Intolerance of uncertainty mediates the relationship between responsibility beliefs and compulsive checking. J Anxiety Disord. 2009;23:1047-1052. [DOI] [PubMed] [Google Scholar]
- 27.Nota SP, Bot AG, Ring D, Kloen P. Disability and depression after orthopaedic trauma. Injury. 2015;46:207-212. [DOI] [PubMed] [Google Scholar]
- 28.Nunez F, Vranceanu AM, Ring D. Determinants of pain in patients with carpal tunnel syndrome. Clin Orthop Relat Res. 2010;468:3328-3332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ozkan S, Zale EL, Ring D, Vranceanu AM. Associations between pain catastrophizing and cognitive fusion in relation to pain and upper extremity function among hand and upper extremity surgery patients. Ann Behav Med. 2017;51:547-554. [DOI] [PubMed] [Google Scholar]
- 30.PROMIS. PROMIS Measures. Available at: http://www.promishealth.com. Accessed April 26, 2019.
- 31.PROMIS. PROMIS PF Scoring. Available at: http://www.healthmeasures.net/administrator/components/com_instruments/uploads/PROMIS%20Physical%20Function%20Scoring%20Manual.pdf. Accessed April 26, 2019.
- 32.Rosen NO, Knauper B, Di Dio P, Morrison E, Tabing R, Feldstain A, Amsel R, Mayrand MH, Franco EL, Rosberger Z. The impact of intolerance of uncertainty on anxiety after receiving an informational intervention about HPV: a randomised controlled study. Psychol Health. 2010;25:651-668. [DOI] [PubMed] [Google Scholar]
- 33.Singh GK. Area deprivation and widening inequalities in US mortality, 1969-1998. Am J Public Health. 2003;93:1137-1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sole E, Tome-Pires C, de la Vega R, Racine M, Castarlenas E, Jensen MP, Miro J. Cognitive fusion and pain experience in young people. Clin J Pain. 2016;32:602-608. [DOI] [PubMed] [Google Scholar]
- 35.Sternheim L, Konstantellou A, Startup H, Schmidt U. What does uncertainty mean to women with anorexia nervosa? An interpretative phenomenological analysis. Eur Eat Disord Rev. 2011;19:12-24. [DOI] [PubMed] [Google Scholar]
- 36.Sternheim L, Startup H, Schmidt U. An experimental exploration of behavioral and cognitive-emotional aspects of intolerance of uncertainty in eating disorder patients. J Anxiety Disord. 2011;25:806-812. [DOI] [PubMed] [Google Scholar]
- 37.Strout TD, Hillen M, Gutheil C, Anderson E, Hutchinson R, Ward H, Kay H, Mills GJ, Han PKJ. Tolerance of uncertainty: a systematic review of health and healthcare-related outcomes. Patient Educ Couns. 2018;101:1518-1537. [DOI] [PubMed] [Google Scholar]
- 38.Taha S, Matheson K, Cronin T, Anisman H. Intolerance of uncertainty, appraisals, coping, and anxiety: the case of the 2009 H1N1 pandemic. Br J Health Psychol. 2014;19:592-605. [DOI] [PubMed] [Google Scholar]
- 39.Tolin DF, Abramowitz JS, Brigidi BD, Foa EB. Intolerance of uncertainty in obsessive-compulsive disorder. J Anxiety Disord. 2003;17:233-242. [DOI] [PubMed] [Google Scholar]
- 40.Wever M, Smeets P, Sternheim L. Neural correlates of intolerance of uncertainty in clinical disorders. J Neuropsychiatry Clin Neurosci. 2015;27:345-353. [DOI] [PubMed] [Google Scholar]
- 41.Wicksell RK, Lekander M, Sorjonen K, Olsson GL. The Psychological Inflexibility in Pain Scale (PIPS)--statistical properties and model fit of an instrument to assess change processes in pain related disability. Eur J Pain. 2010;14:771 e771-714. [DOI] [PubMed] [Google Scholar]
- 42.Wicksell RK, Olsson GL, Hayes SC. Psychological flexibility as a mediator of improvement in acceptance and commitment therapy for patients with chronic pain following whiplash. Eur J Pain. 2010;14:1059 e1051-1059 e1011. [DOI] [PubMed] [Google Scholar]
- 43.Wicksell RK, Renofalt J, Olsson GL, Bond FW, Melin L. Avoidance and cognitive fusion--central components in pain related disability? Development and preliminary validation of the Psychological Inflexibility in Pain Scale (PIPS). Eur J Pain. 2008;12:491-500. [DOI] [PubMed] [Google Scholar]
- 44.Yook K, Kim KH, Suh SY, Lee KS. Intolerance of uncertainty, worry, and rumination in major depressive disorder and generalized anxiety disorder. J Anxiety Disord. 2010;24:623-628. [DOI] [PubMed] [Google Scholar]