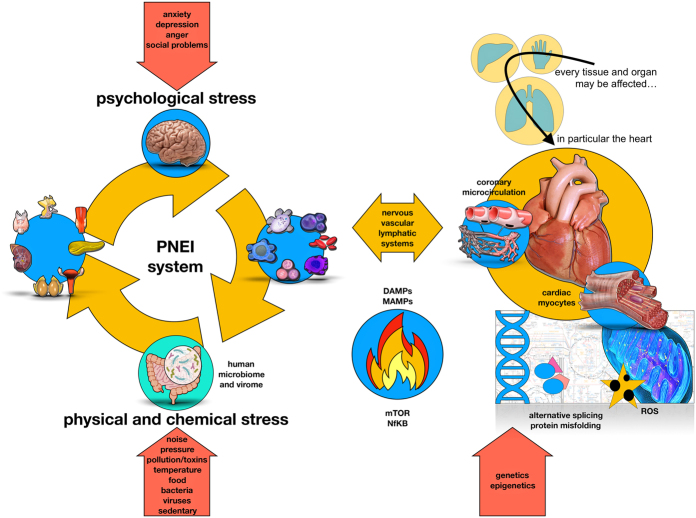
Figure 2.
The human organism always tries to maintain its stability by adapting (allostasis) to external (physical and chemical) or internal (psychological) stimuli. In particular, stimuli are divided into physiological or non-physiological. Non-physiological stimuli (physical/chemical and psychological) are able to stress our psycho-neuro-endocrine-immune adaptation system (PNEI) (35) (left panel). Along with neurotransmitters, hormones and cytokines, also the human microbiome (and virome) plays an important role in the pathogenesis of many immune-mediated diseases, including cardiovascular disorders (29). The resulting immune activation can potentially affect all tissues. At the cardiovascular level, immune cells (activated either by a psychological or physical stressor) interact with endothelial cells, cardiac stromal cells and cardiomyocytes, which adapt their metabolism to support the ongoing inflammatory process (upper part right panel). In the heart (lower side of the right panel), the stress signal can mediate the activation of the intracellular transduction pathways linked to mTOR (39) and NfKB (40) genes through the mediators of the PNEI system (i.e hormones, neurotransmitters and cytokines). This will influence the cellular energy metabolism with high oxidative stress and damage from free radicals (41), misfolding of proteins (42) or their abnormal synthesis (alternative splicing) (43). Thus, cardiac cells expose danger signals that are detected by the immune system. The whole process can be resolved with regeneration/repair (depending on the tissue potential) in case of control and resolution of the acute stimulus or with tissue destruction in case of stress persistence and chronic processes. Of note, the ‘cardioimmune’ inflammatory activation can be activated by psychological stress and the stress activated patterns can be transmitted across generations via epigenetic modulation (44, 45).

 This work is licensed under a
This work is licensed under a