Abstract
Background
Magnetic resonance imaging (MRI) is widely used to diagnose acute abdominal pain; however, it remains unclear which pulse sequence has priority in acute abdominal pain.
Purpose
To investigate the diagnostic accuracy of MRI and to assess the conspicuity of each pulse sequence for the diagnosis of acute abdominal pain due to gastrointestinal diseases
Material and Methods
We retrospectively enrolled 60 patients with acute abdominal pain who underwent MRI for axial and coronal T2-weighted (T2W) imaging, fat-suppressed (FS)-T2W imaging, and true-fast imaging with steady-state precession (True-FISP) and axial T1-weighted (T1W) imaging and investigated the diagnosis with endoscopy, surgery, histopathology, computed tomography, and clinical follow-up as standard references. Two radiologists determined the diagnosis with MRI and rated scores of the respective sequences in assessing intraluminal, intramural, and extramural abnormality using a 5-point scale after one month. Diagnostic accuracy was calculated and scores were compared by Wilcoxon-signed rank test with Bonferroni correction.
Results
Diagnostic accuracy was 90.0% and 93.3% for readers 1 and 2, respectively. Regarding intraluminal abnormality, T2W, FS-T2W, and True-FISP imaging were superior to T1W imaging in both readers. FS-T2W imaging was superior to True-FISP in reader 2 (P < 0.0083). For intramural findings, there was no significant difference in reader 1, whereas T2W, FS-T2W, and True-FISP imaging were superior to T1W imaging in reader 2 (P < 0.0083). For extramural findings, FS-T2W imaging was superior to T2W, T1W, and True-FISP imaging in both readers (P < 0.0083).
Conclusion
T2W and FS-T2W imaging are pivotal pulse sequences and should be obtained before T1W and True-FISP imaging.
Keywords: Ultrafast magnetic resonance image, pulse sequence, acute abdominal pain, gastrointestinal disease
Introduction
Acute abdominal pain is a common presentation that accounts for 4%–8% of all emergency department admissions and can represent life-threatening conditions (1,2). Therefore, prompt and correct diagnosis is essential for acute abdominal pain that requires urgent management, including surgery. For patients with acute abdominal pain, computed tomography (CT) is an essential modality that provides quick and objective evaluation of the entire abdomen and the potential pathology within; 10 min; however, CT is not the best modality for pregnant patients and children due to radiation exposure (3,4). Furthermore, iodine contrast media, required for precise CT diagnosis, has potential adverse effects, including anaphylaxis and contrast media-induced nephropathy (5,6). Conversely, magnetic resonance imaging (MRI) is suitable for pregnant patients and children as well as patients with renal dysfunction or contraindications to contrast-enhanced CT (7–9). However, one of the major disadvantages of MRI for the diagnosis of acute abdominal pain is motion artifacts caused by bowel peristalsis, respiratory movement, and vascular pulsation that deteriorate image quality (10). Therefore, MRI is more frequently utilized for the diagnosis of hepatobiliary and gynecological diseases rather than the evaluation of gastrointestinal diseases (11,12). However, recent technical development including the reduction of motion artifacts has enabled indication of MRI in diagnosing acute appendicitis (13–19), especially in pediatric and pregnant patients (20–24).
Utilization of the ultrafast imaging protocol instead of conventional turbo spin-echo sequences is one of the solutions of this limitation and efficacy of various such pulse sequences, including single-shot T2-weighted (T2W) imaging, fat-suppressed (FS) single-shot T2W imaging, T1-weighted (T1WI) imaging, and true-fast imaging with steady-state precession (True-FISP), etc. is being investigated and has been presented in recent review articles (2); however, specific sequences that should be obtained and its priority in acute abdominal pain caused by gastrointestinal diseases have still not been determined (25). The requirement for MRI in the use of acute abdominal pain is to provide highly accurate images with less artifacts within a limited examination time. Therefore, the acquisition time of pulse sequences should be short, allowing for the patient’s breath holding, and the whole examination time needs to be reduced by selecting an essential imaging pulse sequence; in imaging, sequences should be performed to obtain more information because the examination may have to be stopped due to the patient’s condition.
The aims of the present study was therefore to reveal the diagnostic accuracy of ultrafast MRI and to assess the conspicuity of each pulse sequence in the diagnosis of acute abdominal pain due to gastrointestinal diseases.
Material and Methods
Patients
This single-center retrospective study was approved by the institutional review board and written informed consent was waived. MRI indications for acute abdominal pain at the study institution were as follows: pregnant female patients; female patients with suspicious pregnancy; and pediatric patients aged ≤20 years who were initially assessed by ultrasound that did not lead to a diagnosis. In addition, in patients aged 21–30 years and in those with renal function impairment or iodine contrast allergy who underwent non-contrast CT as the first imaging evaluation that did not lead to a diagnosis, MRI instead of contrast-enhanced CT was performed to reduce exposure to radiation and avoid the adverse effects of iodine contrast media.
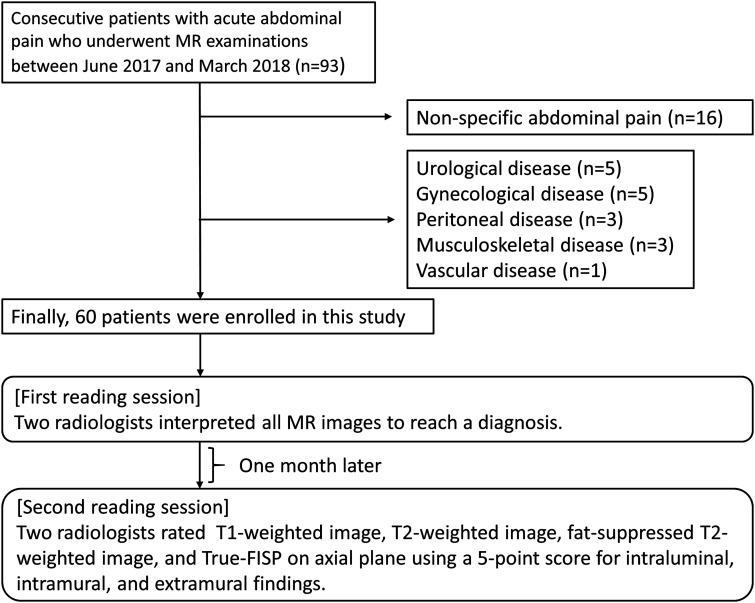
Between June 2017 and March 2018, a total of 93 patients with acute abdominal pain suggesting gastrointestinal disease or that with a non-specific origin based on physical examination underwent MRI examination. A non-reader radiologist with 12 years of experience in emergency imaging searched the clinical diagnosis from the medical records, including blood tests, ultrasound, CT, endoscopy, laparotomy, pathology, findings, and the clinical course. Non-specific abdominal pain (n = 16) that showed no abnormal finding on other examinations and naturally improved without treatment such as medication or surgery was excluded. After the exclusion of patients diagnosed with urological (n = 5), gynecological (n = 5), musculoskeletal (n = 3), peritoneal (n = 3), and vascular (n = 1) diseases, a total of 60 patients (32 male patients, 38 female patients; average age = 46.5 years; age range = 9–91 years) with acute gastrointestinal lesion were included in this study (Fig. 1). Uncomplicated appendicitis (n = 10), enterocolitis (n = 5), and colonic diverticulitis (n = 2) were diagnosed based on the combination of blood test, CT findings, and clinical follow-up. Enterocolitis (n = 6), intussusception (n = 3), and penetrating gastric ulcer (n = 1) were diagnosed based on endoscopic findings. Uncomplicated appendicitis (n = 15), complicated appendicitis (n = 10), duodenal perforation (n = 3), colonic perforation (n = 2), and bowel obstruction (n = 2) were based on surgical finding. Meckel diverticulitis (n = 1) was diagnosed based on histopathological findings. The definitive diagnoses are presented in Table 1.
Fig. 1.
Enrolled patients and reading sessions in the present study.
Table 1.
Cases enrolled in this study
| Diagnosis | Cases (n) | Standard reference | Cases (n) |
|---|---|---|---|
| Uncomplicated appendicitis | 25 | Surgery | 15 |
| Blood test, CT, and clinical follow-up | 10 | ||
| Complicated appendicitis | 10 | Surgery | 10 |
| Enteritis or colitis | 11 | Endoscopy | 6 |
| Blood test, CT, and clinical follow-up | 5 | ||
| Intussusception | 3 | Endoscopy | 3 |
| Duodenal perforation | 3 | Surgery | 3 |
| Colonic perforation | 2 | Surgery | 2 |
| Diverticulitis | 2 | Blood test, CT, and clinical follow-up | 2 |
| Bowel obstruction | 2 | Surgery | 2 |
| Penetrating gastric ulcer | 1 | Endoscopy | 1 |
| Meckel diverticulitis | 1 | Histopathology | 1 |
| Total | 60 | 60 |
CT, computed tomography.
MRI examination
A 1.5-T MRI scanner (Magnetom Aera, Siemens Healthineers, Forchheim, Germany) and an 18-channel surface coil (1.5-T Tim Coil, Siemens Healthineers, Forchheim, Germany) were used for all patients. The MRI protocol included axial T1W imaging, axial and coronal T2W imaging, axial and coronal FS-T2W imaging, and axial and coronal True-FISP. Table 2 shows pulse sequences used in the study. The acquisition time of each imaging sequence was in the range of 22–44 s and the total examination time depended on each patient’s condition and was in the range of 15–20 min.
Table 2.
Pulse sequences included in the study.
| Parameter | T2W imaging (HASTE) | FS-T2W imaging (HASTE) | GRE T1W imaging (VIBE) | True-FISP |
|---|---|---|---|---|
| Plane | Axial, coronal | Axial, coronal | Axial | Axial, coronal |
| Breath-hold | Yes | Yes | Yes | Yes |
| Fat saturation | No | SPAIR | No | No |
| FOV (mm) | 320 (axial) | 320 (axial) | 320 (axial) | 320 (axial) |
| 400 (coronal) | 400 (coronal) | 400 (coronal) | 400 (coronal) | |
| Matrix (mm) | 320 × 320 | 320 × 320 | 320 × 320 | 320 × 320 |
| Slice thickness (mm) | 5 | 5 | 5 | 5 |
| Gap (mm) | 1.5, 1 | 1.5, 1 | 0 | 1 |
| Repetition time (ms) | 700 | 700 | 7.35 | 4.26 |
| Echo time (ms) | 70 | 70 | 2.39 | 2.13 |
| Flip angle (°) | 140 | 140 | 10 | 60 |
| Concatenations | 1 | 1 | 1 | 1 |
| Scan time (s) | 18 × 2 (axial) | 18 × 2 (axial) | 22 | 22 × 2 (axial) |
| 18 (coronal) | 18 (coronal) | 22 (coronal) |
FOV, field of view; FS-T2W, fat-suppressed T2-weighted; GRE, gradient echo; HASTE, half-Fourier single-shot turbo spin-echo; SPAIR, spectral attenuated inversion recovery; T1W, T1-weighted; T2W, T2-weighted; True-FISP, true-fast imaging of steady-state precession; VIBE, volumetric interpolated breath-hold examination.
Image analysis
Two radiologists with 10 and 30 years of experience in MRI interpretation, who were informed of the chief complaint, age, and sex of the patients but were blinded to the results of the clinical examination and diagnosis, interpreted the MRI, including all sequences independently to reach a diagnosis. One month later, the readers were informed of the definitive diagnosis and they were asked to assess the MR findings; intraluminal findings included bowel dilatation and fluid collection (Fig. 2); intramural findings included wall thickening, mass, and wall defect (Figs. 3 and 4); extramural findings included fat stranding (Figs. 3 and 4) and lymphadenopathy on the axial plane images of respective sequences. A 5-point score was used: 1 = non-diagnostic; 2 = diagnosis questionable; 3 = moderate diagnostic accuracy but acceptable; 4 = good diagnostic accuracy; 5 = excellent diagnostic accuracy.
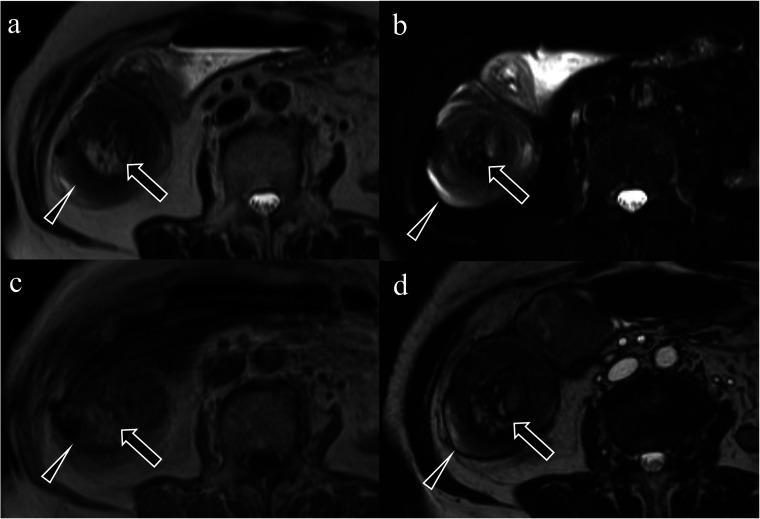
Fig. 2.
An 89-year-old woman who presented with lower abdominal pain was diagnosed with intussusception due to ascending colon cancer. (a) T1-weighted image. (b) T2W image. (c) Fat-suppressed T2W image. (d) True-fast imaging of steady-state precession. Intraluminal findings, including mesenteric fat and swollen lymph nodes in the ascending colon (target sign), indicating intussusception, are observed (a–d, arrows). The thickened wall of the ascending colon is seen (intramural findings) (a–d, arrowheads). T2W, T2-weighted.
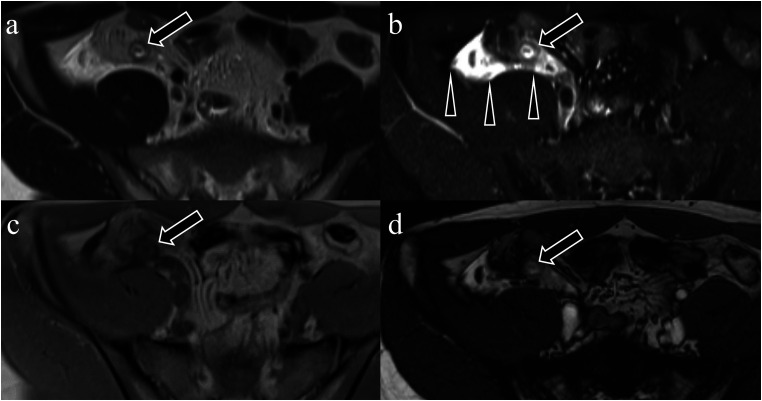
Fig. 3.
An 18-year-old man complaining of right lower abdominal pain diagnosed with acute appendicitis. (a) T1-weighted image. (b) T2W image. (c) FS-T2W image. (d) True-fast imaging of steady-state precession. Thickening of the appendiceal wall (intramural finding) is observed in all sequences (a–d, arrows). Fat stranding surrounding the appendix (extramural findings) is the most obvious on the FS-T2W image (b, arrowheads). FS, fat-suppressed; T2W, T2-weighted.
Fig. 4.
An 80-year-old man who presented with acute abdominal pain after defecation was diagnosed with necrotizing ischemic colitis. (a) T1-weighted image. (b) T2W image. (c) FS-T2W image. (d) True-fast imaging of steady-state precession. Intramural findings, including wall thickening (a–d, arrows) and the partial mucosal defect (intramural findings) (a–d, arrowheads) are observed in the transverse colon in all sequences. Mild fat stranding meaning extramural finding is observed in the transverse mesocolon in the FS-T2W image (extramural findings) (b, circle). FS, fat-suppressed; T2W, T2-weighted.
Statistical analysis
Diagnostic accuracy in the diagnosis of primary lesions was calculated based on the first MRI interpretation in both readers. Next, scores of respective sequences based on the second MRI interpretation were evaluated using Friedman’s one-way analysis of variance (ANOVA) with average values. To determine groups responsible for significant differences by ANOVA, Wilcoxon’s signed rank test was performed. A P value < 0.0083 after Bonferroni correction was considered to indicate a statistically significant difference. All statistical tests were performed using statistical software (R version 3.6.2, R Foundation, Vienna, Austria).
Results
Diagnostic accuracy was 90.0% and 93.3% by readers 1 and 2, respectively. False-negative diagnoses were found in cases with acute appendicitis (n = 3) and Meckel diverticulitis (n = 1), bowel obstruction (n = 1), colonic perforation (n = 1) in reader 1 and acute appendicitis (n = 2), Meckel diverticulitis (n = 1), and colonic perforation (n = 1) in reader 2.
Tables 3–5 show the result of scores for each pulse sequence. For intraluminal findings, the scores were comparable between T2W and FS-T2W imaging for both readers. T2W imaging, FS-T2W imaging, and True-FISP were superior to T1W imaging for both readers (P < 0.0083). In addition, for reader 2, FS-T2W imaging was superior to True-FISP (P < 0.0083) (Table 3). For intramural findings, there was no significant difference for reader 1, whereas T2W imaging, FS-T2W imaging, and True-FISP were superior to T1W imaging (P < 0.0083) for reader 2 (Table 4). For extramural findings, FS-T2W imaging was superior to T2W imaging, T1W imaging, and True-FISP for both readers. T2W imaging and True-FISP were also superior to T1W imaging for reader 2 (P < 0.0083) (Table 5).
Table 3.
Comparison of reader scores among respective pulse sequences for intraluminal findings.
| Score | T2W imaging | FS-T2W imaging | T1W imaging | True-FISP | |
|---|---|---|---|---|---|
| Reader 1 | |||||
| T2W imaging | 3.98 ± 1.03 | – | – | – | – |
| FS-T2W imaging | 4.23 ± 1.14 | 0.0229 | – | – | – |
| T1W imaging | 3.33 ± 0.90 | <0.0001* | <0.0001* | – | – |
| True-FISP | 4.05 ± 1.16 | 0.3674 | 0.2246 | <0.001* | – |
| Reader 2 | |||||
| T2W imaging | 2.83 ± 1.39 | – | – | – | – |
| FS-T2W imaging | 3.35 ± 1.34 | 0.0389 | – | – | – |
| T1W imaging | 1.27 ± 0.73 | <0.0001* | <0.0001* | – | – |
| True-FISP | 2.63 ± 1.52 | 0.3574 | 0.0075* | <0.0001* | – |
Values are given as means ± standard deviation. Scores for primary abnormal findings were assessed by Wilcoxon’s signed rank test with Bonferroni correction.
*P < 0.0083.
T1W, T1-weighted; T2W, T2-weighted; FS-T2W, fat-suppressed T2-weighted; True-FISP, true-fast imaging of steady-state precession.
Table 4.
Comparison of reader scores among respective pulse sequences for intramural findings
| Score | T2W imaging | FS-T2W imaging | T1W imaging | True-FISP | |
|---|---|---|---|---|---|
| Reader 1 | |||||
| T2W imaging | 3.80 ± 0.95 | – | – | – | – |
| FS-T2W imaging | 3.97 ± 1.02 | 0.2004 | – | – | – |
| T1W imaging | 3.68 ± 0.79 | 0.2802 | 0.0139 | – | – |
| True-FISP | 3.68 ± 0.91 | 0.4026 | 0.0347 | 0.8631 | – |
| Reader 2 | |||||
| T2W imaging | 3.98 ± 1.03 | – | – | – | – |
| FS-T2W imaging | 3.82 ±1.21 | 0.5642 | – | – | – |
| T1W imaging | 2.48 ± 1.32 | <0.0001* | <0.0001* | – | – |
| True-FISP | 3.48 ± 1.33 | 0.0443 | 0.1682 | <0.0001* | – |
Values are given as means ± standard deviation. Scores for primary abnormal findings were assessed by Wilcoxon’s signed rank test with Bonferroni correction.
*P < 0.0083.
T1W, T1-weighted; T2W, T2-weighted; FS-T2W, fat-suppressed T2-weighted; True-FISP, true-fast imaging of steady-state precession.
Table 5.
Comparison of reader scores among respective pulse sequences for extramural findings.
| Score | T2W imaging | FS-T2W imaging | T1W imaging | True-FISP | |
|---|---|---|---|---|---|
| Reader 1 | |||||
| T2W imaging | 3.52 ± 1.10 | – | – | – | – |
| FS-T2W imaging | 3.95 ± 1.33 | 0.0043* | – | – | – |
| T1W imaging | 3.07 ± 1.09 | 0.0099 | <0.0001* | – | – |
| True-FISP | 3.45 ± 1.24 | 0.9301 | 0.0056* | 0.0263 | – |
| Reader 2 | |||||
| T2W imaging | 1.61 ± 0.96 | – | – | – | – |
| FS-T2W imaging | 3.03 ± 1.55 | <0.0001* | – | – | – |
| T1W imaging | 1.08 ± 0.38 | <0.0001* | <0.0001* | – | – |
| True-FISP | 1.82 ±1.08 | 0.2741 | <0.0001* | <0.0001* | – |
Values are given as means ± standard deviation. Scores for primary abnormal findings were assessed by Wilcoxon’s signed rank test with Bonferroni correction.
*P < 0.0083.
T1W, T1-weighted; T2W, T2-weighted; FS-T2W, fat-suppressed T2-weighted; True-FISP, true-fast imaging of steady-state precession.
Discussion
We investigated the diagnostic accuracy of MRI as well as the degree of contribution for the detection of intraluminal, intramural, and extramural findings by each pulse sequence using a 5-point score for acute abdominal pain caused by gastrointestinal diseases. The diagnostic accuracy of MRI was 90.0%–93.3%. For intraluminal findings, T2W and FS-T2W imaging were superior to T1W imaging for both readers, and one reader showed True-FISP was also superior to T1W imaging. For intramural findings, one reader demonstrated that T2W imaging, FS-T2W imaging, and True-FISP were superior to T1W imaging. For extramural findings, FS-T2WI was the best sequence for both readers.
Compared with turbo spin-echo T2W imaging, single-shot T2W imaging is obtained in a shorter scan time and is unlikely to be affected by motion artifact; however, it is related to blurring and relative increase in signal intensity of free water (26,27). Currently, single-shot T2W imaging is considered an appropriate sequence for acute abdominal pain. Byott et al. (28) reported that axial and coronal single-shot T2W imaging, which required <2 min for image acquisition, diagnosed acute abdominal pain with a sensitivity of 98% and a specificity of 92%. Mian et al. (29) demonstrated that abbreviated MRI protocols, including axial and coronal single-shot T2W imaging and axial diffusion-weighted imaging (DWI) with short acquisition times, achieved a sensitivity of 100% and a specificity of 75% compared with the standard protocol. Although the present study used T1W, FS-T2W, True-FISP, and T2W imaging, its diagnostic accuracy (90.0%–93.3%) is almost similar to that of previous studies evaluating only T2W or T2W imaging and DWI (28,29). Furthermore, T2W imaging was given a significantly higher score than T1W imaging for intraluminal and intramural findings. Thus, T2W imaging is considered to be a pivotal pulse sequence for the diagnosis of acute abdominal pain caused by gastrointestinal diseases.
Extramural findings, such as fat stranding, were best appreciated by FS-T2W imaging. At the site of inflammation, vascular permeability is increased to induce the migration of immunocytes and cytokines from the peripheral blood into the tissue, including mesenteric fat, which results in increased fluid content at the inflammation site. FS-T2W imaging is the most sensitive sequence for demonstrating edema and inflammation in retroperitoneal and mesenteric fat surrounding the primary site in acute abdominal pain because an obvious contrast between the low-intense fat tissue and high-intense water can be observed on FS-T2W imaging (30). Therefore, FS-T2W imaging has different diagnostic values from T2W imaging and should be obtained for patients with acute abdominal pain.
T1W imaging has the advantage of depicting hemorrhagic conditions (12). Furthermore, a bright appendix on T1W imaging that reflects stool is helpful to exclude acute appendicitis in pregnant women (31). Nevertheless, in the present study, T1W imaging showed inferior scores in detecting intraluminal, intramural, and extramural findings. This could have occurred due to several reasons: no patient with hemorrhagic pathologies, such as gastrointestinal bleeding and intestinal endometriosis, was enrolled in our cohort; however, most cases with acute gastrointestinal bleeding are not suitable for MRI. The second reading session was designated to assess the diagnostic value of each pulse sequence but not to determine whether appendicitis is present or absent; on the other hand, the T1 bright appendix sign aimed to exclude acute appendicitis. We consider the advantage of T1W imaging to be limited to the diagnosis of acute abdominal pain caused by gastrointestinal disease except for hemorrhagic pathology and acute appendicitis.
True-FISP was similar or inferior to T2W and FS-T2W imaging for the assessment of intraluminal and intramural findings and inferior to FS-T2W imaging for the assessment of extramural findings. True-FISP may provide an advantage by avoiding flow void and is beneficial for accessing mucosal lesions without artifacts from movement of the intestinal contents by peristalsis, although it is related to India ink artifact seen as a dark line around the organs (32). In the diagnosis of acute abdominal pain, however, the intestines are not generally filled with fluid, excluding those with bowel obstruction. Given that flow voids in the intestines are not a serious concern in patients with acute abdominal pain, except for those with bowel obstruction, the disadvantage of the India ink artifact obscuring pathology of the bowel wall outweighs the advantage of absent flow void in True-FISP; therefore, True-FISP can be replaced with T2W and FS-T2W imaging.
The present study has several limitations. First, the number of patients was relatively small in this single-center study performed at a general hospital. Second, the study was designed retrospectively and potential selection bias cannot be ruled out. Although the study institution has specific MRI indication criteria for acute abdominal pain, some patients who matched the criteria might not have undergone MRI examination: there is only one magnetic resonance scanner at the study institution, and emergency scanning might not have been possible for some patients due to the packed schedule. The clinicians might have selected alternative modalities instead of MRI for patients with unstable hemodynamics or claustrophobia. Third, the present study focused on gastrointestinal diseases and excluded gynecological, urological, and musculoskeletal diseases that followed different MRI protocols. In fact, physicians should elucidate the affected organ by physical examination although it may be difficult in some cases. Fourth, T2W imaging, FS-T2W imaging, and True-FISP contained axial and coronal images, whereas only axial images were available for T1W imaging. Therefore, only the axial plane was evaluated in the second interpretation session for comparable assessment of all sequences. Fifth, DWI was not included in this study. DWI can indicate acute inflammatory process as high signal intensity (16–19), which is meaningful; however, it does not provide sufficient anatomical and morphological information unlike the other pulse sequences. Therefore, we thought DWI had a different role in diagnosing acute abdominal pain compared to the other pulse sequences and the equal comparison of DWI with them was not appropriate. Finally, a further examination, which proves the non-inferiority of ultrafast MRI protocol compared with the conventional protocol, will be needed to place an ultrafast MRI protocol in clinical routine practices in the future.
In conclusion, MRI was an accurate modality for the diagnosis of acute abdominal pain caused by gastrointestinal diseases. Single-shot T2W and FS-T2W imaging were more informative than T1W imaging and True-FISP. Therefore, T2W and FS-T2W imaging should be performed first and followed by T1W imaging and True-FISP because MRI may have to be terminated at any time due to the patient’s condition, and T1W imaging and True-FISP may be canceled depending on the situation.
Acknowledgements
The authors thank Enago (www.enago.jp) for the English language review.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Akitoshi Inoue https://orcid.org/0000-0002-8610-2571
References
- 1.Stoker J, van Randen A, Laméris W, et al. Imaging patients with acute abdominal pain. Radiology 2009; 253:31–46. [DOI] [PubMed] [Google Scholar]
- 2.Yu HS, Gupta A, Soto JA, et al. Emergency abdominal MRI: current uses and trends. Br J Radiol 2016; 89:20150804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mayumi T, Yoshida M, Tazuma S, et al. The practice guidelines for primary care of acute abdomen 2015. Jpn J Radiol 2016; 34:80–115. [DOI] [PubMed] [Google Scholar]
- 4.Garcia EM, Camacho MA, Karolyi DR, et al. ACR appropriateness criteria® right lower quadrant pain-suspected appendicitis. J Am Coll Radiol 2018; 15:S373–S387. [DOI] [PubMed] [Google Scholar]
- 5.Rosado Ingelmo A, Doña Diaz I, Cabañas Moreno R, et al. Clinical Practice Guidelines for Diagnosis and Management of Hypersensitivity Reactions to Contrast Media. J Investing Allergol Clin Immunol 2016; 26:144–155. [DOI] [PubMed] [Google Scholar]
- 6.Ohno I, Hayashi H, Aonuma K, et al. Guidelines on the use of iodinated contrast media in patients with kidney disease 2012: digest version. JSN, JRS, and JCS Joint Working Group. Jpn J Radiol 2013; 31:546–584. [DOI] [PubMed] [Google Scholar]
- 7.Masselli G, Derchi L, McHugo J, et al. Acute abdominal and pelvic pain in pregnancy: ESUR recommendations. Eur Radiol 2013; 23:3485–3500. [DOI] [PubMed] [Google Scholar]
- 8.Beddy P, Keogan MT, Sala E, et al. Magnetic resonance imaging for the evaluation of acute abdominal pain in pregnancy. Semin Ultrasound CT MR 2010; 31:433–441. [DOI] [PubMed] [Google Scholar]
- 9.Baheti AD, Nicola R, Bennett GL, et al. Magnetic Resonance Imaging of Abdominal and Pelvic Pain in the Pregnant Patient. Magn Reson Imaging Clin N Am 2016; 24:403–417. [DOI] [PubMed] [Google Scholar]
- 10.Zaitsev M, Maclaren J, Herbst M. Motion artifacts in MRI: A complex problem with many partial solutions. J Magn Reson Imaging 2015; 42:887–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee SL, Kim HK, Choi HH, et al. Diagnostic value of magnetic resonance cholangiopancreatography to detect bile duct stones in acute biliary pancreatitis. Pancreatology 2018; 18:22–28. [DOI] [PubMed] [Google Scholar]
- 12.Iraha Y, Okada M, Iraha R, et al. CT and MR imaging of gynecologic emergencies. RadioGraphics 2017; 37:1569–1586. [DOI] [PubMed] [Google Scholar]
- 13.Nitta N, Takahashi M, Furukawa A, et al. MR imaging of the normal appendix and acute appendicitis. J Magn Reson Imaging 2005; 21:156–165. [DOI] [PubMed] [Google Scholar]
- 14.Repplinger MD, Pickhardt PJ, Robbins JB, et al. Prospective comparison of the diagnostic accuracy of MR imaging versus CT for acute appendicitis. Radiology 2018; 288:467–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eng KA, Abadeh A, Ligocki C, et al. Acute appendicitis: a meta-analysis of the diagnostic accuracy of US, CT, and MRI as second-line imaging tests after an initial US. Radiology 2018; 288:712–727. [DOI] [PubMed] [Google Scholar]
- 16.Inci E, Kilickesmez O, Hocaoglu E, et al. Utility of diffusion-weighted imaging in the diagnosis of acute appendicitis. Eur Radiol 2011; 21:768–775. [DOI] [PubMed] [Google Scholar]
- 17.Leeuwenburgh MM, Wiarda BM, Bipat S, et al. Acute appendicitis on abdominal MR images: Training Readers to Improve Diagnostic Accuracy. Radiology 2012; 264:455–463. [DOI] [PubMed] [Google Scholar]
- 18.Avcu S, Çetin FA, Arslan H, et al. The value of diffusion-weighted imaging and apparent diffusion coefficient quantification in the diagnosis of perforated and nonperforated appendicitis. Diagnostic Interv Radiol 2013; 19:106–110. [DOI] [PubMed] [Google Scholar]
- 19.Inoue A, Furukawa A, Nitta N, et al. Accuracy, criteria, and clinical significance of visual assessment on diffusion-weighted imaging and apparent diffusion coefficient quantification for diagnosing acute appendicitis. Abdom Radiol 2019; 44:3235–3245. [DOI] [PubMed] [Google Scholar]
- 20.Kinner S, Pickhardt PJ, Riedesel EL, et al. Diagnostic accuracy of MRI versus CT for the evaluation of acute appendicitis in children and young adults. Am J Roentgenol 2017; 209:911–919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bayraktutan Ü, Oral A, Kantarci M, et al. Diagnostic performance of diffusion-weighted MR imaging in detecting acute appendicitis in children: Comparison with conventional MRI and surgical findings. J Magn Reson Imaging 2014; 39:1518–1524. [DOI] [PubMed] [Google Scholar]
- 22.Pedrosa I, Levine D, Eyvazzadeh A. MR imaging evaluation of acute appendicitis in pregnancy. Radiology. 2006; 238:891–899. [DOI] [PubMed] [Google Scholar]
- 23.Patel D, Fingard J, Winters S, et al. Clinical use of MRI for the evaluation of acute appendicitis during pregnancy. Abdom Radiol 2017; 42:1857–1863. [DOI] [PubMed] [Google Scholar]
- 24.Chang PT, Schooler GR, Lee EY. Diagnostic errors of right lower quadrant pain in children: beyond appendicitis. Abdom Imaging 2015; 40:2071–2090. [DOI] [PubMed] [Google Scholar]
- 25.Petkovska I, Martin DR, Covington MF, et al. Accuracy of unenhanced MR imaging in the detection of acute appendicitis: single-institution clinical performance review. Radiology 2016; 279:451–460. [DOI] [PubMed] [Google Scholar]
- 26.Chung HW, Chen CY, Zimmerman RA, et al. T2-Weighted fast MR imaging with true FISP versus HASTE: comparative efficacy in the evaluation of normal fetal brain maturation. AJR Am J Roentgenol 2000; 175:1375–1380. [DOI] [PubMed] [Google Scholar]
- 27.Zhang L, Kholmovski EG, Guo J, et al. HASTE sequence with parallel acquisition and T2 decay compensation: application to carotid artery imaging. Magn Reson Imaging 2009; 27:13–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Byott S, Harris I. Rapid acquisition axial and coronal T2 HASTE MR in the evaluation of acute abdominal pain. Eur J Radiol 2016; 85:286–290. [DOI] [PubMed] [Google Scholar]
- 29.Mian M, Khosa F, Ali IT, et al. Faster magnetic resonance imaging in emergency room patients with right lower quadrant pain and suspected acute appendicitis. Pol J Radiol 2018; 83:e340–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Singh A, Danrad R, Hahn PF, et al. MR imaging of the acute abdomen and pelvis: Acute appendicitis and beyond. Radiographics 2007; 27:1419–1431. [DOI] [PubMed] [Google Scholar]
- 31.Shin I, An C, Lim JS, et al. T1 bright appendix sign to exclude acute appendicitis in pregnant women. Eur Radiol 2017; 27:3310–3316. [DOI] [PubMed] [Google Scholar]
- 32.Gourtsoyiannis N, Papanikolaou N, Grammatikakis J, et al. MR imaging of the small bowel with a true-FISP sequence after enteroclysis with water solution. Invest Radiol 2000; 35:707–711. [DOI] [PubMed] [Google Scholar]