Figure 2.
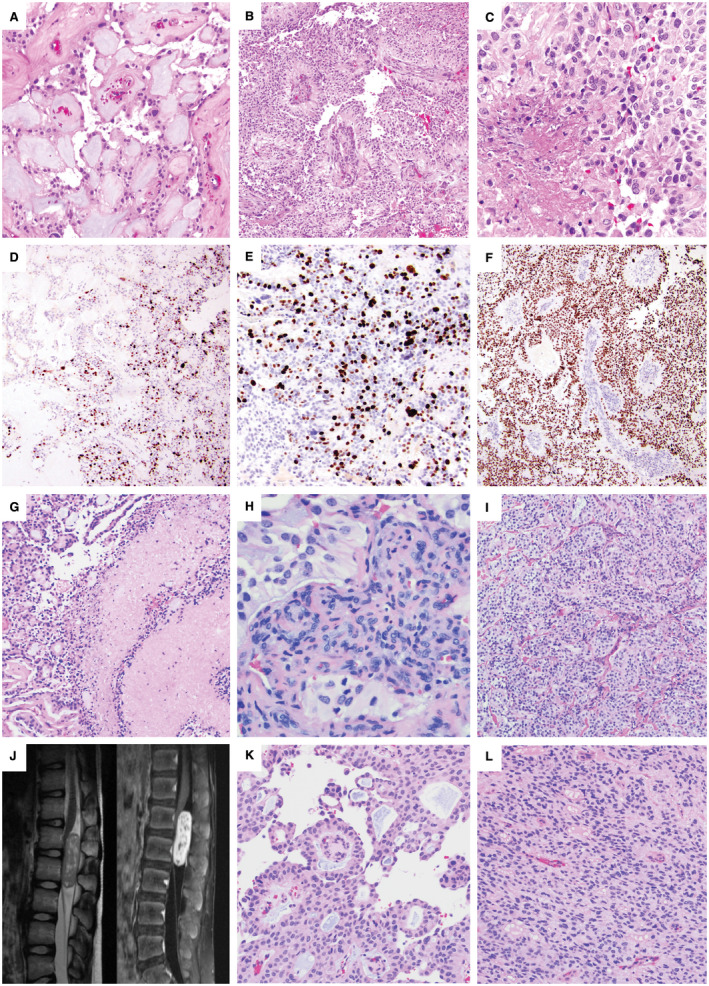
Adult and pediatric intradural anaplastic myxopapillary ependymomas. A–F. Case #14: A 55‐year‐old woman with a 2.7‐cm L1‐L2 mass and CSF dissemination with masses involving the cauda equina at the time of diagnosis underwent gross total resection and radiation therapy. The initial resection included areas of classic MPE (A) intermixed with anaplastic areas demonstrating hypercellularity and reduced mucin (B). The mitotic index reached 7 mitoses per 10 HPF, and there was both non‐palisading necrosis (C) and microvascular proliferation (MVP). A sharp transition between the classic and anaplastic components was present, reflected both by the histology and the variation in Ki‐67 (D), which was 20% in the anaplastic component (E) and <1% in conventional areas (D); left side). There was diffuse nuclear p53 positivity within the areas of anaplastic transformation (F). Recurrence 18 months later as a 2.3‐cm L2 mass also showed anaplastic features. G–I. Case #9: A 31‐year‐old man with an intradural sacral mass and smaller thoracic tumor deposits underwent subtotal resection, chemotherapy and a partial course of radiation. Re‐resection of the sacral MPE 9 months later showed both palisading and non‐palisading necrosis (G), which was not considered an anaplastic feature because of prior chemoradiation therapy. Anaplastic features included a Ki‐67 LI of 10%, a mitotic index of 7/10 HPF and MVP (H). Many areas of the tumor showed hypercellularity with decreased mucin (I). The patient was lost to clinical follow‐up and died at 36 years of age; no autopsy was performed. J–L. Case #4: A 10‐year‐old boy presented with an intradural extramedullary L1‐L2 enhancing mass centered at the conus medullaris by spinal MRI (J). Portions of the tumor showed classic MPE histology with papillary architecture and a myxoid stroma (K), while anaplastic regions were hypercellular with reduced mucin (L). Anaplastic features included a Ki‐67 LI of up to 15%, 6 mitoses per 10 high power fields and small foci of MVP.
