Fig 2.
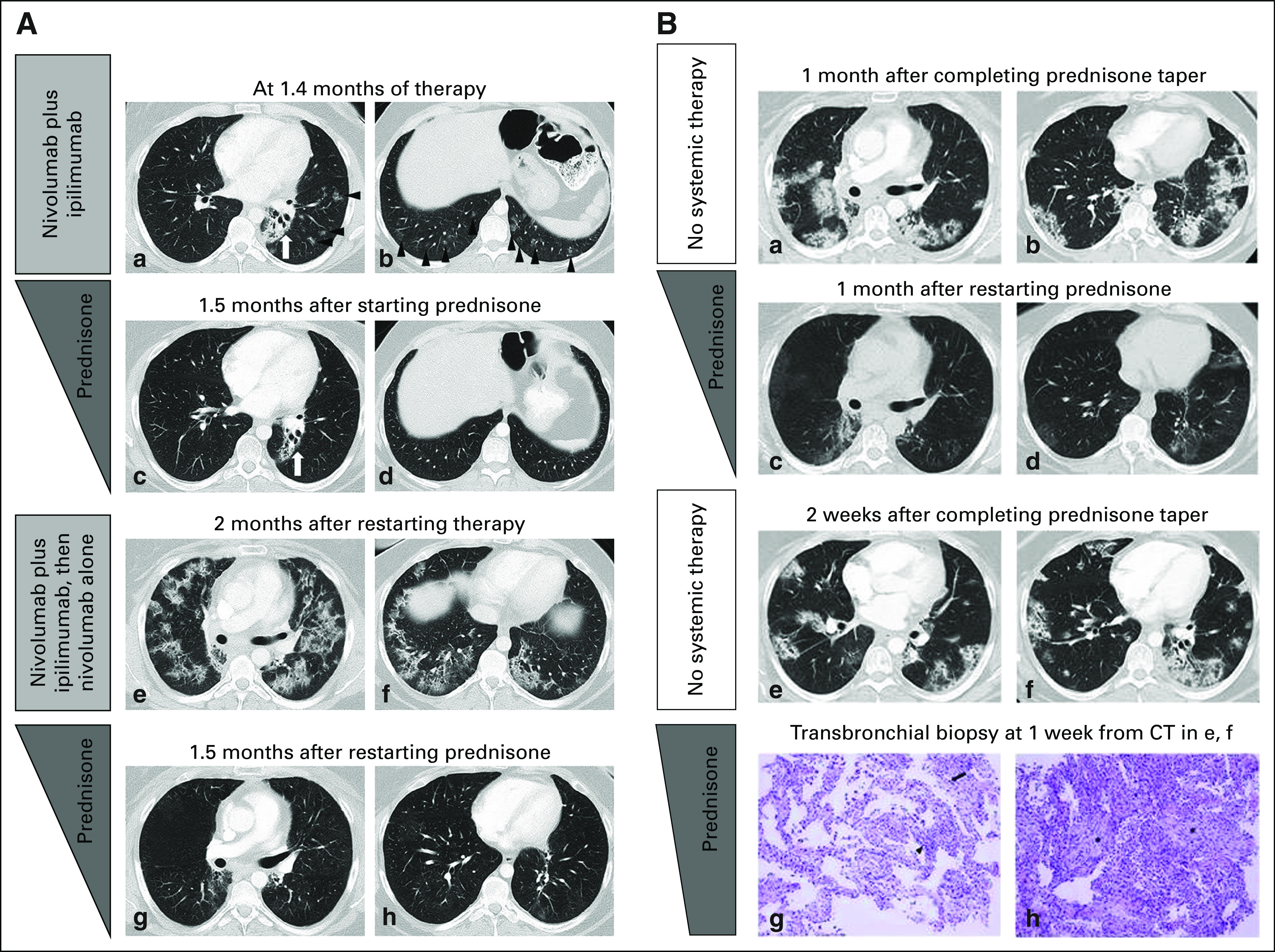
Pneumonitis with a cryptogenic organizing pneumonia (COP) pattern in a 33-year-old female with Hodgkin lymphoma who was treated with nivolumab and ipilimumab combination therapy, with a recurrence during retreatment (2A; a–h) and two episodes of pneumonitis flare after completion of corticosteroid taper (2B; a–h). Reprinted with permission from Nishino et al.5 2A: (a and b) Computed tomography (CT) scan of the chest at 1.4 months of therapy demonstrated ground-glass and reticular opacities and consolidations with multifocal distribution, which are indicative of a COP pattern of pneumonitis (arrowheads). Left perihilar opacity and traction bronchiectasis are a result of prior radiation therapy (arrows). (2A: c and d) The patient was treated with oral prednisone taper, and the findings have resolved on the follow-up scan performed 1.5 month later. (2A: e and f). The patient restarted therapy and received two doses of nivolumab and ipilimumab and two doses of nivolmab monotherapy, then developed recurrent pneumonitis 2 months after restarting therapy. The scan at the time of recurrent pneumonitis demonstrated similar findings with multifocal ground-glass and reticular opacities and consolidations, which again represented a COP pattern. The findings were more extensive than the first episode. (2A: g and h) Nivolumab was held and the patient was treated again with prednisone taper for pneumonitis, with subsequent improvement. (2B: a and b) The patient completed 2 months of corticosteroid taper, and after 1 month, experienced another episode of pneumonitis with a similar radiographic pattern, without nivolumab retreatment or other systemic therapy, which indicated a pneumonitis flare. (2B: c and d) Another course of corticosteroid taper was administered, with subsequent improvement. (2B: e and f) The 2.7-month course of corticosteroid taper was completed, and after 2 weeks, the patient again developed a pneumonitis flare with a similar radiographic pattern as prior episodes. (2B: g and h) The sampled fragments of lung that were obtained by transbronchial biopsies showed interstitial pneumonitis that evolved to organizing pneumonia. Findings included lymphocyte-predominant interstitial pneumonitis (arrowhead, 2B[g], hematoxylin and eosin stain, ×200) with rare eosinophils (arrow, 2B [g]), and areas of organizing pneumonia with fibroblast plugs and foamy macrophages filling the airspaces (asterisks, 2B [h], hematoxylin and eosin stain, ×200). No tumor cells, microorganisms, or viral cytopathic changes were identified. The patient started another course of prednisone taper with subsequent clinical improvement and is schedule for a follow-up CT scan.
