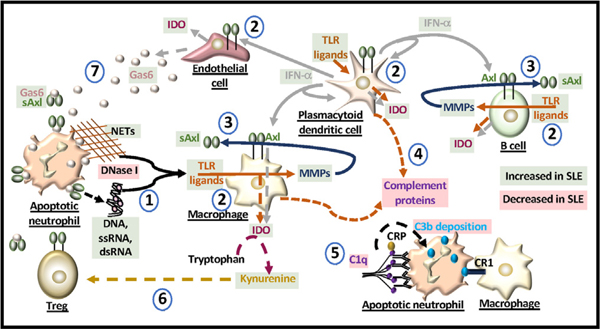
Fig. 2. Molecules dysregulated in SLE.
(1) Mutations in DNase I can limit the degradation of DNA from apoptotic cells and/or from neutrophil extracellular traps (NETs) and induce the release of nucleic acids that can act as TLR ligands. (2) IFN-α and IDO production are elevated in SLE. TLR ligands induce the production of IFN-α and IDO from antigen presenting cells and endothelial cells. IFN-α also induces the production of IDO and cell surface expression of Axl. (3) TLRs can generate matrix metalloproteinases (MMPs) that cleave Axl from the cell surface. In SLE, soluble Axl (sAxl) is elevated and generated mainly from macrophages and B cells. (4) The production of complement proteins is modulated by TLR ligands. (5) C1q binds antibodies that opsonize the apoptotic cell. C reactive protein (CRP) binds to C1q in activating the complement cascade involving C3b deposition which binds to macrophage complement receptor 1 (CR1). Reduced levels of C1q alter macrophage uptake of apoptotic cells. (6) IDO generates kynurenine from tryptophan that can enhance the formation of Tregs. Kynurenine production is elevated in SLE but the levels of Tregs do not increase. Ligation of Treg Axl with Gas6 enhances their suppressor activity which may be blocked by sAxl. (7) Gas6 sourced from activated endothelial cells is elevated in SLE and binds apoptotic cells and Axl. In SLE, the levels of sAxl may block immune cell recognition of apoptotic cells and alter the function of immune and non-immune cells in the microenvironment.