Abstract
Short segment fixation aims to restore spinal stability and alignment in thoracolumbar spine injuries while preserving spinal motion by decreasing the levels of spine involved in fixation. In its simplest form it applies to fixation one level above and one level below the fractured vertebra. It has proven effective with good clinical, functional and radiological results in well selected cases. However not insignificant rates of sagittal collapse and recurrence of kyphosis with or without clinical implications have also been reported. Most of the failures were attributed to lack of anterior column integrity and relatively inferior robustness of earlier posterior short segment constructs. With better understanding of fracture biomechanics, better implant designs and evolution of strategies to increase the biomechanical strengths of posterior constructs, the rates of kyphosis recurrence and implant failure have been significantly reduced. Although there is lack of robust evidence to guide a surgeon to the best approach for a particular fracture, adhering to basic biomechanical principals increases the efficacy and reliability of short segment fixation. This narrative review highlights the status of short segment fixation in dorsolumbar spine injuries with emphasis on patient selection and strategies to increase effectiveness and reduce failures of short segment fixation.
Keywords: Spine injuries, Thoracolumbar, Short segment fixation
1. Introduction
The goal of operative treatment of thoracolumbar spinal fractures is to protect neurological function and to restore spinal stability and alignment. The surgical strategy chosen should correct segmental kyphotic deformity and prevent late instability and pain while permitting early ambulation and return to function. To this end, different surgical techniques such as posterior pedicle screw fixation; anterior decompression, arthrodesis and instrumentation; and combined anterior and posterior approaches have been described.1, 2, 3, 4, 5, 6 Due to concerns regarding disc degeneration and adjacent segment disease in a predominantly young trauma population, minimising the number of spinal levels to be involved in fixation/fusion is one of the avowed goal of any instrumentation for spine injury.7 This is achieved by short segment fixation i.e. fixation at levels adjacent to the fractured vertebra. While short segment fixation has demonstrated good results in thoracolumbar injuries,6, 7, 8 it can be accompanied by not insignificant rates of hardware failures and recurrence of kyphosis with or without clinical implications.9, 10, 11 This has been attributed to insufficient anterior support and less robust instrumentation leading to a biomechanical failure.10,12 Modifications in short segment fixation have helped to reduce failure rates.13, 14, 15, 16 Despite the reported failures, short segment instrumentation remains the preferred choice of most surgeons for majority of thoracolumbar injuries because of it being patient friendly, easy to perform and with acceptable clinical results. This narrative review will discuss the current status of short segment fixation in management of thoracolumbar injuries. The strategies to decrease the failure rates and increase the effectiveness of short segment instrumentation will also be discussed.
2. Classification of thoracolumbar injuries
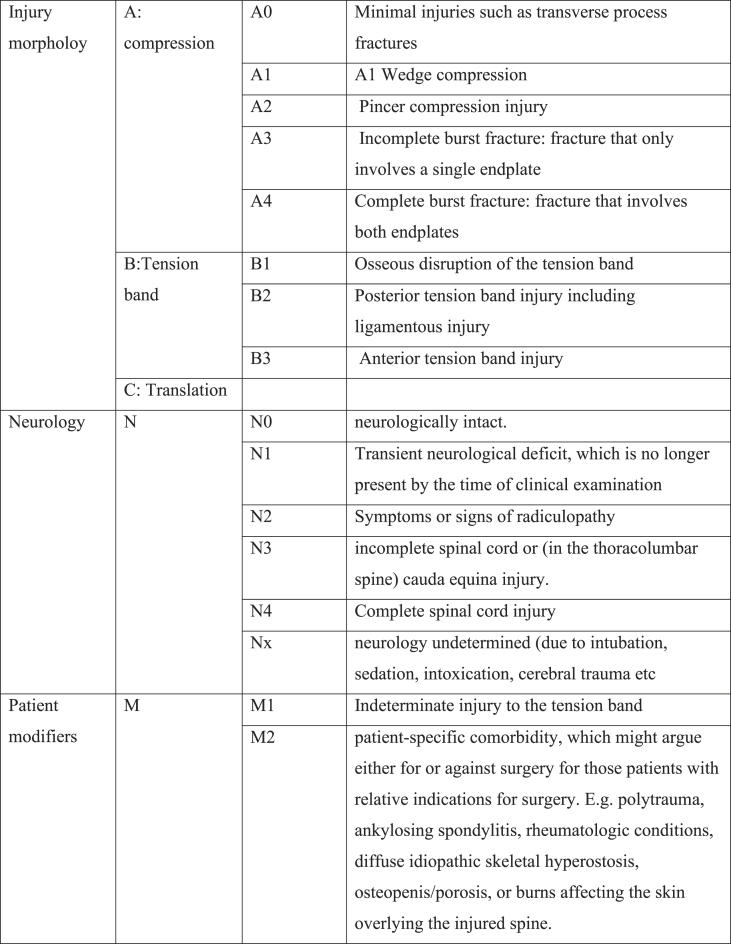
As the understanding of the biomechanics of spine and the imaging modalities have improved, various classification systems of thoracolumbar injuries have been described.17, 18, 19 This has led to lot of confusion in classifying fractures as well the treatment based on each of the classification system. For ease of understanding and because it incorporates most of the current knowledge and practice on thoracolumbar injuries, AOSpine Thoracolumbar Spine Injury Classification20 has been used in this review (Fig. 1). This system classifies a spine injury based on injury morphology, neurological status and two patient specific modifiers (M1 and M2). Injury morphology is divided into three main groups: type A—compression; type B—tension band injury; and type C—translation injuries with a total of 9 subgroups. Of these morphological patterns, there is a general consensus that type B and type C injuries need surgical treatment while A0 to A2 can be managed conservatively. Most of the controversy has been on treatment of burst fractures i.e. A3 and A4 injuries.
Fig. 1.
AO classification20(developed by AO Spine Knowledge Forum Trauma).
3. Indications for short segment fixation
Short segment fixation is typically reserved for unstable burst fractures. Multiple studies have shown good results of short segment fixation in well selected cases.6, 7, 8,11,13 The issue of stability in burst fractures is a vexed one and still unresolved. Vaccaro et al. introduced the concept of PLC or posterior ligamentous complex19 to indicate instability but the interobserver agreement in determining the status of the posterior longitudinal ligament is very low and hence it cannot be the sole determinant of instability in burst fractures.21 Loss of more than 50% anterior vertebral height reduction, local kyphosis greater than 20°, or canal encroachment more than 50% have also been used as markers of instability in burst fractures.22, 23, 24 Presence of neurological injury has been independently thought to be indicating instability irrespective of vertebral deformity.22, 23, 24 However good robust evidence to support any of the above criteria is lacking. It should be remembered that besides radiological parameters, patient specific factors like polytrauma, ankylosing spondylitis, rheumatoid arthritis, overlying skin condition, fitness for bracing etc may further influence the decision to manage a burst fracture operatively or conservatively.25
Most of the studies of conservative treatment of burst fractures do not involve patients with neurological deficit and a burst fracture with neurological deficit is managed by surgical methods by most surgeons.26 However, presence of neurological deficit is not an absolute indication for short segment instrumentation. Dai et al. did not experience neurological deterioration in any of the cases in a subset of 22 patients with neurological involvement out of a total of 127 burst fractures treated conservatively.27 However the reasons for choosing conservative treatment in this subset of patients were not mentioned in their study.
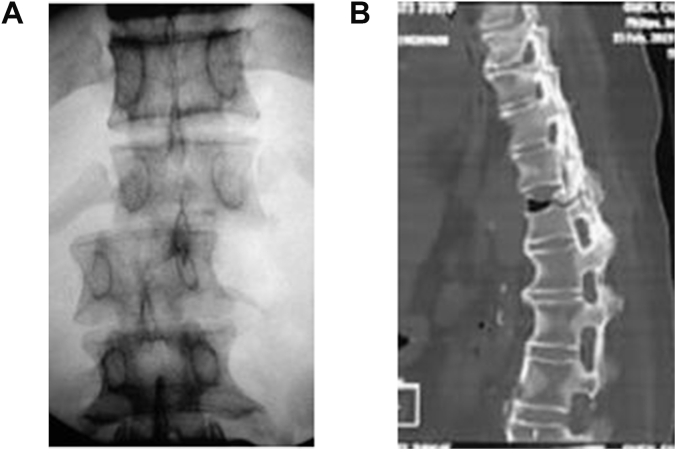
Short segment fixation can also be reliably used in flexion distraction injuries or type B injuries in non ankylosed spines.28,29 Long constructs are commonly used in highly unstable Type C rotational and translational thoracolumbar injuries(Fig. 2a) to counteract the high deforming forces, though there have been reports of successful use of short segment fixation in thoracolumbar fracture dislocations.30 Another scenario in which short segment instrumentation cannot be reliably used is for thoracolumbar injuries in ankylosed spines(Fig. 2b). Spinal fractures are subject to high torques because of long lever arms in ankylosed spines. This increases the stress at the implant bone interface. Osteoporosis is also very common in ankylosing disorders further increasing the risk of implant failure. Long segment constructs with more points of fixation are needed to reduce the risk of implant failure.31,32
Fig. 2.
Injuries not amenable to short segment fixation. 2a. Fracture dislocations of spine. 2b. Injuries in ankylosed spine.
4. Strategies for reduction and canal clearance with posterior short segment fixation
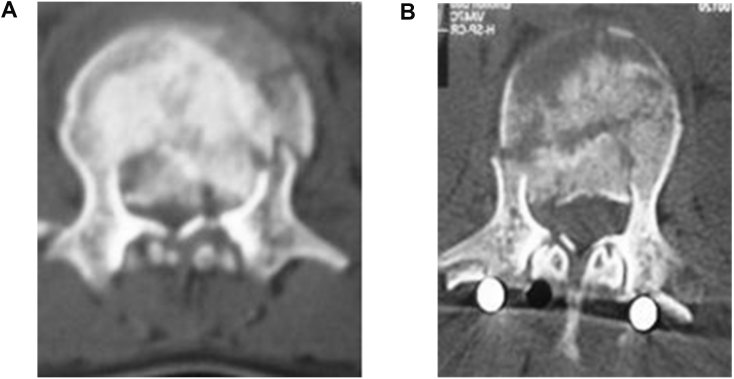
In short segment fixation, fracture reduction can be achieved by a combination of postural reduction, pre-contouring of rods and cantilever correction.7, 33 Pedicle screws with their 3 column purchase can provide distraction to all the 3 columns the spine. Distraction should be done carefully based on the damaged endplate.34 Excessive distraction will lead to differential increase in distraction across posterior column exacerbating kyphotic angulation and stressing the screw-bone interface.7, 33 Thus, careful attention also must be directed toward generating concomitant lordosis and re-establishing sagittal balance.33 Lordosing manoeuvres, either by pre-contoured rods or by approximating distal ends of Schanz screws, must be performed first before applying controlled distraction. Monoaxial screws are favoured as they deliver greater forces for deformity correction.33 A common technique used to increase the effectiveness of short segment instrumentation is use of screw in the fractured vertebra. In this technique, the screw in fractured vertebra is inserted with a slightly increased vertical offset. This acts as a push point increasing the forward force and provides a lordosing force at the time of reduction of appropriately precontoured rod onto the screws at lower end vertebra.13 The fulcrum of this forward thrust is the screw head of the pedicle screw in the fractured vertebra and this causes the compression to occur posterior to the screw head and distraction at the structures that are anterior to it. Tensioning of the annulus and posterior longitudinal ligament, indirectly reduces the retropulsed fragments thus helping to achieve canal clearance.33 Indirect reduction thus achieved helps to improve local kyphosis, restore vertebral height and decrease canal encroachment (Fig. 3, Fig. 4).
Fig. 3.
Canal clearance achieved by posterior short segment instrumentation and indirect reduction. 3a. Preoperative axial view. 3b. Immediate postoperative axial CT.
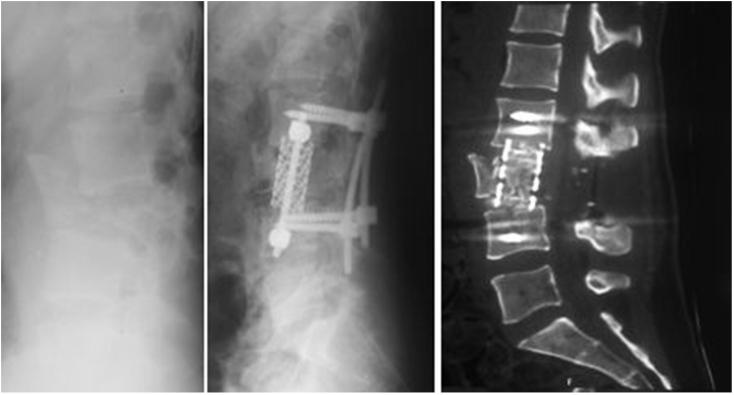
Fig. 4.
Effective restoration of vertebral body height and segmental lordosis by short segment fixation.
5. Efficacy of short segment fixation
A review of published studies showed that an immediate correction of kyphosis angle ranging from 6.2⁰ to 21.4 ⁰ is achieved after short segment instrumentation.35 Significant improvements in anterior vertebral height ranging from 50 to 100% and vertebral wedge angle are also achieved.36,37 Sjostrom et al. showed that after indirect reduction of burst fractures, canal encroachment decreased from a mean of 40%(range 8–70%) to 20%(range 7–62%).38 Gertzbein et al. demonstrated a residual encroachment of 40% after an initial average encroachment of 54%. The canal clearance was best when the initial encroachment was between 34% and 66% and if done within first 4 days.39 Indirect reduction techniques may not be as effective in achieving canal clearance in burst fractures with a suspicion of ruptured annular ligaments or when a reverse cortical sign is present.39,40 All the clinical studies report very good clinical results with mean VAS typically less than 2, ODI less than 20 and significant improvement in other functional scores and capacity to return to work.40,41
6. Posterolateral fusion with short segment fixation
The use of posterolateral fusion along with short segment instrumentation is questionable. It is not associated with improved clinical outcomes and it does not prevent kyphosis recurrence or implant failure(Table 1). Moreover, it is accompanied by longer operative times, increased blood loss and donor site morbidity.6,11,34,42 Posterolateral fusion does not provide the spine with the sufficient strength to resist predominantly anterior axial loads leading to recurrence of kyphosis.36 Inferior results in fusion groups in some studies may be due to use of spinous processes as graft. This reduces the tension band effect of the posterior column leading to recurrence of kyphosis. The improvement in clinical parameters and health related quality of life was uniformly good in both fusion and non fusion groups across all studies. Multiple uncontrolled studies also show similar outcomes as regards to clinical and radiological parameters in patients treated with or without fusion.6,11
Table 1.
Studies comparing posterior short segment fixation with or without posterolateral fusion.
| Study | No. Of cases | Kyphosis recurrence | Decrease in vertebral body height | Implant failure | Blood loss | Operative time | |
|---|---|---|---|---|---|---|---|
| Wang34 | fusion | 30 | 4.80 | 8.3% | 16.6% | 572 | 224 |
| non fusion | 28 | 1.00 | 3.6% | 10.7% | 303 | 162 | |
| Jindal11 | fusion | 23 | 5.50 | – | 8.7% | 486 | 142 |
| non fusion | 24 | 3.6° | – | 4.2% | 378 | 107 | |
| Lin dai42 | fusion | 37 | 1.40 | – | Nil | 423 | 152 |
| non fusion | 36 | 1.70 | – | Nil | 310 | 102 |
7. Implant failure with short segment instrumentation
There have been reports of significant rates of implant failure ranging from 9 to 54% with short segment instrumentation. The mean loss of correction ranged from 0.30 to 15.40 35. McLain et al. were among the first to describe the failures of short segment instrumentation in their series of 19 patients with thoracolumbar fractures of which 11 were treated by short segment fixation. 5(45%) out of these 11 patients experienced failure from bending or breakage of screws with all the failures occurring within the first 6 months. In situ bending of the rods and pre-stressing of the screws through compression/distraction manoeuvres was attributed to the failure of instrumentation.9 McCormack et al. analysed cases with failure of short segment instrumentation and they felt that the degree of vertebral comminution was the cause of failure. They came up with a load sharing classification (LSC) to quantify this comminution and predict failure of posterior fixation. Three separate characteristics of the fracture i.e. the amount of vertebral body comminution as seen in sagittal CT reconstructions, apposition of fracture fragments as seen in axial CT cuts through the fracture site and the amount of corrected kyphotic deformity as measured by comparing preoperative and postoperative lateral plain films, were graded. Each of these factors was subdivided into three grades of severity and was scored on a point system from 1 to 3. In their series all 10 (out of 28) patients with implant failure had a LSC score more than 7 and out of these 5 had a score of 9, the maximal possible in their scheme.10 Dai et al. found that LSC scores were more predictive of late kyphosis in conservatively treated burst fractures as well.27 Altay et al. observed that radiological outcomes of short segment fixation are dependent on fracture location, type of fracture and LSC score of the fracture. More correction loss was observed in L1 fractures treated by short segment fixation having higher LSC score.35 On the contrary Scholl et al. concluded that LSC was not predictive of short segment instrumentation failure in a retrospective review of 22 patients with thoracolumbar fractures.43
Disc integrity is also thought to be a contributing factors to recurrence of kyphosis besides the vertebral body comminution.36 In studies where the implants were routinely removed, progression of kyphosis even when vertebral body height is maintained would implicate disc as the cause.36 The mechanism of disc collapse remains a matter of controversy. Disruption of vascularity of the endplates, stress shielding effect of posterior fixation and herniation of the disc into the central depression of the endplate are some of the proposed mechanisms.36,37
Other postulated reasons for failure have been poor implant or construct design such as a small diameter junction between screw head and shaft, in situ bending of the rod, damage to the posterior structures and stressing the screws with excessive distraction.6,7,9,11
8. Strategies to counter short segment instrumentation failures
The strategies to counter short instrumentation failure have focussed either on anterior augmentation or augmenting the biomechanical strengths of posterior construct.
8.1. Augmenting the posterior short segment construct
The strategies for increasing the biomechanical strength of posterior constructs include the use of crosslinks, addition of a supplemental hook fixation at the levels of the screws, and additional fixation with pedicle screws in the fractured vertebra.13 Intermediate or index level screws (a screw into the fractured vertebra) have proven to be very effective in maintenance of sagittal alignment and minimising implant failure. Dick et al. reported the first instance of use of an intermediate screw to increase the biomechanical strength of short-segment construct. In a cadaveric model, they proved that axial stiffness and flexion stiffness increased 160% and 84% respectively with the addition of intermediate screw as opposed to cross links.14 Mahar et al. termed this fixation as segmental construct and concluded that a segmental construct increased construct stiffness for axial torsion stiffness and it protected the anterior column during flexion-extension loading.15 In a cadaveric biomechanical model, Bartanusz et al. found that short segment fracture screw fixation with intermediate level screws was biomechanically equivalent to combined anterior–posterior constructs.16
8.1.1. Clinical effectiveness of augmentation with index/intermediate level screws
Clinical studies have also attested to the effectiveness of short segment instrumentation with screws at the intermediate or index level.7,8,13,28,45,46 In a study on 72 thoracolumbar burst fractures with unstable burst fractures, Guven et al. observed that fractured vertebra fixation resulted in lowered rates of kyphosis correction failure and that this fixation was equivalent to a construct with fixation 2 levels above and below the fracture.44 Gelb et al. concluded that pedicle screw placement into the fractured vertebra seemed to protect against correction loss as 57% of the cohort with no intermediate screw had >10° loss of kyphosis correction as compared to none in intermediate screw group. There was no relation between loss of kyphosis correction and load sharing classification, Magerl type, or level of injury.7 Farrokhi et al. compared short segment instrumentation with or without fracture level fixation in a group of 80 patients with thoracolumbar fractures. Higher rate of impant failure were found in the group with no screw in the fractured vertebra. This group showed a mean worsening of 29% in kyphosis, whereas the group with fixation in fractured vertebra had a significant improvement by a mean of 6%. The effectiveness of intermediate level fixation in reduction of kyphotic deformity and maintenance of sagittal alignment was most marked in Magerl type C fractures.28 Kose et al. used a thinner and shorter screw in fractured vertebra due to the fear of distracting fracture fragments. The mean sagittal index was corrected to −1.8° (−5°–3°) from 19.6° (12°–28°). At final follow up, the mean sagittal index was 2.4° (0°–8°). None of the patients in their series required revision for loss of correction or failure of instrumentation. The load sharing classification did not influence the results.45 Kanna et al. used fixation at the fractured level in 32 burst fractures with LSC >7 in a retrospective, uncontrolled series of patients. There were no implant failures and mean loss of kyphosis correction was 1–2°. It was concluded that there was no need for anterior fixation even in injuries with LSC>713. In a comparative study on 60 patients, Dobran et al. concluded that inclusion of fracture level in a short-segment fixatiotn was as effective as long segment fixation in kyphosis correction and maintenance of sagittal alignment for unstable burst fracture at thoracolumbar junction. At final follow up, local kyphosis angle(LKA) was 15.97° ± 5.62° for short segment fixation and 17.76° ± 11.22° for long segment fixation.46 Common to all the studies was emphasis on achieving lordosis by contouring and no overdistraction.
8.1.2. Contraindications to index level screw fixation
Presence of a break in the pedicular wall is a contraindication to index level fixation. It is recommended to use the intermediate screw on only one side if the other side is fractured.13,15 Insertion of unilateral pedicle screw instead of bilateral screws has been shown to have equivalent clinical and radiological results. Sun et al. showed that there was no difference in corrected vertebral wedge angle, local kyphosis angle and anterior vertebral body height in patients treated with either unilateral or bilateral fixation in the fractured vertebra at a mean follow-up of 18.3 months in a well matched cohort of thoracolumbar burst fractures with LSC>7.47
8.2. Anterior column support
Based on preceding discussion it would appear intuitive that anterior column support would address the issue of implant failure and recurrent kyphosis. Strategies to augment anterior column have utilised 3 approaches:
-
i)
Augmentation through transpedicular route
-
ii)
Anterior approach and reconstruction
-
iii)
Anterior reconstruction through all posterior approach.
8.2.1. Augmentation through transpedicular route
Intracorporeal bone grafting by morselized autograft, vertebroplasty and kyphoplasty with hydroxyapatite, calcium sulphate, or calcium phosphate, balloon assisted endplate reduction(BAER) are some of the techniques that have been used through transpedicular routes in addition to short segment fixation.48,49 Intracorporeal grafting has not proven to be successful in majority of studies despite initial promising results.48 One reason mentioned is the resorption of graft before its incorporation.48 There have been reports of good results with the use of hydroxyapatite, calcium sulphate and calcium phosphate.49 However concerns around cement leakage, displacement of fracture fragments, radiation exposure, additional costs and long term fate of synthetic graft/cement in a predominantly young trauma population need to be answered, especially in light of near universal good results with index level fixation.
8.2.2. Anterior approach and reconstruction
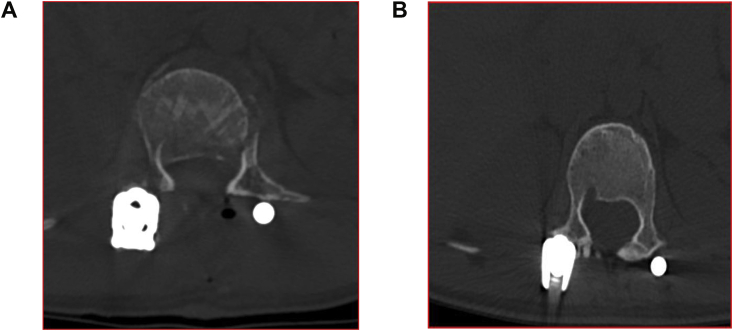
Direct spinal cord decompression and potential for complete kyphosis correction are important advantages of anterior approach. Combined anterior posterior approaches give the best immediate and long term kyphosis correction.3,23 However anterior approach is relatively morbid and might be impractical in a polytrauma situation. It must also be kept in mind that some degree of kyphosis recurrence does not always impact on the clinical outcome.13,37 Further the degree of canal compromise may not actually correlate to neurological dysfunction and a formal anterior clearance might not be needed.11,13 The retropulsed fragment may further remodel obviating the need for canal clearance11(Fig. 5).Sjostrom et al. observed that canal encroachment decreased to a mean of 2% at one year as compared to preoperative 38%(range 10–70%) in burst fractures treated by posterior instrumentation.38 The choice of anterior approach might be impacted by surgeon choice, definition of successful treatment, training and regional variations with European (particularly German surgeons) favouring anterior approaches.50
Fig. 5.
Remodelling at 2 years in a case of burst fracture managed by short segment fixation. 5a. Postoperative axial view. 5b. Axial view at 2 years at same level.
Anterior column support might actually serve to keep the posterior instrumentation as a short segment, particularly in the lumbar spine where it is extremely important to save motion segments(Fig. 6). Korvossis et al. compared short segment fixation with index level screws and a combined ant posterior approach in a well matched cohorts of lumbar fracture. They concluded that short segment transpedicular fixation(SSTF) offered similar significant short term correction of posttraumatic deformities and better immediate clinical results. However, it did not significantly maintain the achieved kyphosis correction at the final evaluation done at 4 years as compared to a combined anterior and posterior approach. They did not recommend SSTF alone for operative stabilization of fractures with this severity although they did report that the anterior group had significantly more postoperative complications.51
Fig. 6.
Anterior reconstruction was used to reconstruct a severely comminuted L3 fracture and keep the instrumentation short segment and save mobile lumbar levels; Follow up CT scan shows maintenance of lumbar lordosis and incorporation of graft.
8.2.3. Anterior reconstruction through all posterior approach
The all posterior/extracavitory approach for anterior reconstruction4 sacrifices important posterior stabilising structures and requires multilevel fixation and should not be recommended with short segment fixation.
9. Modifications of short segment fixation
Short segment fixation using adjacent vertebra as fixation anchor points has been further modified to mono segment fixation or same segment short fixation.52, 53, 54 Originally described by Goetzen, this type of fixation incorporates fixation in one adjacent vertebra besides the fractured vertebra and is meant to save motion segments and possibly limit implant failure while reducing operating times and blood loss.52, 53, 54, 55 This fixation while suitable for purely ligamentous injuries in non ankylosed spines, should be used with caution in burst fractures.52 Finite element analysis have proven that displacements are increased in fractured vertebra under all loading conditions in monosegmental fixation as compared to short segment fixation.56 Fractures with greater comminution, involvement of both superior and inferior endplates and fractures with cortical breach in pedicles are unsuitable for this type of fixation.23,51, 52, 53, 54, 55
10. Conclusion
Posterior short segment instrumentation is sufficient for almost all Type A fractures and type B fractures in a non ankylosed spine. There might be a slight recurrence of kyphosis but the clinical impact is minimal. Index level screws (screw in the fractured vertebra) increases the effectiveness of short segment instrumentation and substantially decreases the implant failure rate. Anterior reconstruction is rarely indicated and if chosen a separate anterior approach helps to save levels and limit instrumentation to short segment.
The future research should focus on identifying the clinical and radiological variables that impact the outcomes in management of thoracolumbar fractures. In particular the definition of instability in relation to radiological parameters need to be well defined to better identify factures needing operative treatment. There is a distinct lack of high quality evidence which would guide surgeons to decide between operative or non operative treatment particularly in burst fractures(AO type A3,A4) with neurological deficit.
Author statement
Rohit Jindal: Literature review, conceptualisation of article, clinical photographs, preliminary and final draft. Vinay Jasani: Literature review, conceptualisation of article , writing of final draft. Dinesh Sandal: Literature review, preliminary draft. Sudhir Kumar Garg: Editing of preliminary and final draft
Declaration of competing interest
None.
References
- 1.McAfee P.C., Bohlman H.H., Yuan H.A. Anterior decompression of traumatic thoracolumbar fractures with incomplete neurological deficits using a retroperitoneal approach. J Bone Joint Surg Am. 1985;67(1):89–104. [PubMed] [Google Scholar]
- 2.Kostuik J.P. Anterior fixation for burst fractures of the thoracic and lumbar spine with or without neurological involvement. Spine. 1988;13(3):286–293. doi: 10.1097/00007632-198803000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Sasso R.C., Renkens K., Hanson D. Unstable thoracolumbar burst fractures: anterior-only versus short-segment posterior fixation. J Spinal Disord Tech. 2006;19(4):242–248. doi: 10.1097/01.bsd.0000211298.59884.24. [DOI] [PubMed] [Google Scholar]
- 4.Haiyun Y., Rui G., Shucai D. Three-column reconstruction through single posterior approach for the treatment of unstable thoracolumbar fracture. Spine. 2010;35(8):E295–E302. doi: 10.1097/BRS.0b013e3181c392b9. [DOI] [PubMed] [Google Scholar]
- 5.Defino H.L., Rodriguez-Fuentes A.E. Treatment of fractures of the thoracolumbar spine by combined anteroposterior fixation using the Harms method. Eur Spine J. 1998;7:187–194. doi: 10.1007/s005860050054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sanderson P.L., Fraser R.D., Hall D.J. Short segment fixation of thoracolumbar burst fractures without fusion. Eur Spine J. 1999;8:495–500. doi: 10.1007/s005860050212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gelb D., Ludwig S., Karp J.E. Successful treatment of thoracolumbar fractures with short-segment pedicle instrumentation. J Spinal Disord Tech. 2010;23(5):293–301. doi: 10.1097/BSD.0b013e3181af20b6. [DOI] [PubMed] [Google Scholar]
- 8.Shen W.J., Liu T.J., Shen Y.S. Non-operative treatment versus posterior fixation for thoracolumbar junction burst fractures without neurologic deficit. Spine. 2001;26(9):1038–1045. doi: 10.1097/00007632-200105010-00010. [DOI] [PubMed] [Google Scholar]
- 9.McLain R.F., Sparling E., Benson D.R. Early failure of short-segment pedicle instrumentation for thoracolumbar fractures. J Bone Joint Surg Am. 1993;75(2):162–167. doi: 10.2106/00004623-199302000-00002. [DOI] [PubMed] [Google Scholar]
- 10.McCormack T., Karaikovic E., Gaines R.W. The load-sharing classification of spine fractures. Spine. 1994;19(15):1741–1744. doi: 10.1097/00007632-199408000-00014. [DOI] [PubMed] [Google Scholar]
- 11.Jindal N., Sankhala S., Bachhal V. The role of fusion in the management of burst fractures of the thoracolumbar spine treated by short segment pedicle screw fixation : a prospective randomised trial. J. Bone Joint Surg. Br. 2012;94(8):1101–1106. doi: 10.1302/0301-620X.94B8.28311. [DOI] [PubMed] [Google Scholar]
- 12.Lazaro B.C., Deniz F.E., Brasiliense L.B. Biomechanics of thoracic short versus long fixation after 3-column injury. J Neurosurg Spine. 2011;14(2):226–234. doi: 10.3171/2010.10.SPINE09785. [DOI] [PubMed] [Google Scholar]
- 13.Kanna R.M., Shetty A.P., Rajashekhran S. Posterior fixation including the fractured vertebra for severe unstable thoracolumbar fractures. Spine J. 2015;15:256–264. doi: 10.1016/j.spinee.2014.09.004. [DOI] [PubMed] [Google Scholar]
- 14.Dick J.C., JonesMP ZdeblickTA., Kunz D.N., Horton W.C. A biomechanical comparison evaluating the use of intermediate screws and crosslinkage in lumbar pedicle fixation. J Spinal Disord. 1994;7(5):402–407. [PubMed] [Google Scholar]
- 15.Mahar A., Kim C., Wedemeyer M. Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fracture. Spine. 2007;32(14):1503–1507. doi: 10.1097/BRS.0b013e318067dd24. [DOI] [PubMed] [Google Scholar]
- 16.Bartanusz V., Harris J., Moldavsky M., Yiwei C., Bucklen B. Vertebra pedicle screw placement for pathologies involving the anterior and middle vertebral column is as effective as long segment stabilization with cage reconstruction: a biomechanical study. Spine. 2015;40(22):1729–1736. doi: 10.1097/BRS.0000000000001130. [DOI] [PubMed] [Google Scholar]
- 17.Denis F. The three-column spine and its significance in the classification of acute thoracolumbar spine injuries. Spine. 1983;8(8):817–831. doi: 10.1097/00007632-198311000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Magerl F., Aebi M., Gertzbein S.D., Harms J., Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3:184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 19.Vaccaro A.R., Lehman R.A., Jr., Hurlbert R.J. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine. 2005;30(20):2325–2333. doi: 10.1097/01.brs.0000182986.43345.cb. [DOI] [PubMed] [Google Scholar]
- 20.Vaccaro A.R., Oner C., Kepler C.K. AOSpine Spinal Cord Injury & Trauma Knowledge Forum. AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine. 2013;38(23):2028–2037. doi: 10.1097/BRS.0b013e3182a8a381. [DOI] [PubMed] [Google Scholar]
- 21.Schroeder G.D., Kepler C.K., Koerner J.D. A worldwide analysis of the reliability and perceived importance of an injury to the posterior ligamentous complex in AO A type fractures. Global Spine J. 2015;5(5):378–382. doi: 10.1055/s-0035-1549034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mclain R.F. The biomechanics of long versus short fixation for thoracolumbar spine fractures. Spine. 2006;31(11S):S70–S79. doi: 10.1097/01.brs.0000218221.47230.dd. [DOI] [PubMed] [Google Scholar]
- 23.Rajasekaran S., Kanna R.M., Shetty A.P. Management of thoracolumbar spine trauma an overview. Indian J Orthop. 2015;49(1):72–82. doi: 10.4103/0019-5413.143914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Verheyden A.P., Spiegl U.J., Ekkerlein H. Treatment of fractures of the thoracolumbar spine: recommendations of the spine section of the German society for orthopaedics and trauma (DGOU) Global Spine J. 2018;8(2 S):34S–45S. doi: 10.1177/2192568218771668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schnake K.J., Schroeder G.D., Vaccaro A.R., andOner C. AOSpine classification systems (subaxial, thoracolumbar) J Orthop Trauma. 2017;31(4S):S14–S23. doi: 10.1097/BOT.0000000000000947. [DOI] [PubMed] [Google Scholar]
- 26.Vaccaro A.R., Lim M.R., Hurlbert R.J. Surgical decision making for unstable thoracolumbar spine injuries: results of a consensus panel review by the Spine Trauma Study Group. J Spinal Disord Tech. 2006;19(1):1–10. doi: 10.1097/01.bsd.0000180080.59559.45. [DOI] [PubMed] [Google Scholar]
- 27.Dai L.Y., Jiang L.S., Jiang S.D. Conservative treatment of thoracolumbar burst fractures: a long-term follow-up results with special reference to the load sharing classification. Spine. 2008;33(23):2536–2544. doi: 10.1097/BRS.0b013e3181851bc2. [DOI] [PubMed] [Google Scholar]
- 28.Farrokhi M.R., Razmkon A., Maghami Z., Nikoo Z. Inclusion of the fracture level in short segment fixation of thoracolumbar fractures. Eur Spine J. 2010;19(10):1651–1656. doi: 10.1007/s00586-010-1449-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu Y.J., Chang M.C., Wang S.T., Yu W.K., Liu C.L., Chen T.H. Flexion–distraction injury of the thoracolumbar spine. Injury. 2003;34(12):920–922. doi: 10.1016/s0020-1383(02)00396-0. [DOI] [PubMed] [Google Scholar]
- 30.Chokshi J.J., Shah M. Outcomes of including fracture level in short- segment fixation for thoracolumbar fracture dislocation. Asian Spine J. 2019;13(1):56–60. doi: 10.31616/asj.2018.0064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reinhold M., Knop C., Kneitz C., Disch A. Spine fractures in ankylosing diseases: recommendations of the spine section of the German society for orthopaedics and trauma (DGOU) Global Spine J. 2018;8(2S):56S–68S. doi: 10.1177/2192568217736268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lindtner R.A., Kammerlander C., Goetzen M. Fracture reduction by postoperative mobilisation for the treatment of hyperextension injuries of the thoracolumbar spine in patients with ankylosing spinal disorders. Arch Orthop Trauma Surg. 2017;137(4):531–541. doi: 10.1007/s00402-017-2653-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Whang P.G., Vaccaro A.R. Thoracolumbar fracture: posterior instrumentation using distraction and ligamentotaxis reduction. J Am Acad Orthop Surg. 2007;15(11):695–701. doi: 10.5435/00124635-200711000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Wang S.T., Ma H.L., Liu C.L., Yu W.K., Chang M.C., Chen T.H. Is fusion necessary for surgically treated burst fractures of the thoracolumbar and lumbar spine?: a prospective, randomized study. Spine. 2006;31(23):2646–2652. doi: 10.1097/01.brs.0000244555.28310.40. [DOI] [PubMed] [Google Scholar]
- 35.Altay M., Ozkurt B., Aktekin C.N. Treatment of unstable thoracolumbar junction burst fractures with short- or long-segment posterior fixation in Magerl type a fractures. Eur Spine J. 2007;16(8):1145–1155. doi: 10.1007/s00586-007-0310-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang X.Y., Dai L.Y., Xu H.Z., Chi Y.L. Kyphosis recurrence after posterior short-segment fixation in thoracolumbar burst fractures. J Neurosurg Spine. 2008;(8):246–254. doi: 10.3171/SPI/2008/8/3/246. [DOI] [PubMed] [Google Scholar]
- 37.Lakshmanan P., Jones A., Mehta J., Ahuja S., Davies P.R., Howes J.P. Recurrence of kyphosis and its functional implications after surgical stabilization of dorsolumbar unstable burst fractures. Spine J. 2009;9(12):1003–1009. doi: 10.1016/j.spinee.2009.08.457. [DOI] [PubMed] [Google Scholar]
- 38.Sjostrom L., Karlstrom G., Pech P., Rauschning W. Indirect spinal canal decompression in burst fractures treated with pedicle screw instrumentation. Spine. 1996;21(1):113–123. doi: 10.1097/00007632-199601010-00026. [DOI] [PubMed] [Google Scholar]
- 39.Gertzbein S.D., Crowe P.J., Fazl M., Schwartz M., Rowed D. Canal clearance in burst fractures using the AO internal fixator. Spine. 1992;17(5):558–560. doi: 10.1097/00007632-199205000-00013. [DOI] [PubMed] [Google Scholar]
- 40.Arlet V., Orndorff D.G., Jagannathan J., Dumont A. Reverse and pseudoreverse cortical sign in thoracolumbar burst fracture: radiologic description and distinction–a propos of three cases. Eur Spine J. 2009;18(2):282–287. doi: 10.1007/s00586-008-0848-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Siebenga J., Leferink V.J., Segers M.J. Treatment of traumatic thoracolumbar spine fractures: a multicenter prospective randomized study of operative versus nonsurgical treatment. Spine. 2006;31(25):2881–2890. doi: 10.1097/01.brs.0000247804.91869.1e. [DOI] [PubMed] [Google Scholar]
- 42.Dai L.Y., Jiang L.S., Jiang S.D. Posterior short-segment fixation with or without fusion for thoracolumbar burst fractures: a five to seven-year prospective randomized study. J Bone Joint Surg Am. 2009;91(5):1033–1104. doi: 10.2106/JBJS.H.00510. [DOI] [PubMed] [Google Scholar]
- 43.Scholl B.M., Theiss S.M., Kirkpatrick J.S. Short segment fixation of thoracolumbar burst fractures. Orthopedics. 2006;29(8):703–708. doi: 10.3928/01477447-20060801-14. [DOI] [PubMed] [Google Scholar]
- 44.Guven O., Kocaoglu B., Bezer M., Aydin N., Nalbantoglu U. The use of screw at the fracture level in the treatment of thoracolumbar burst fractures. J Spinal Disord Tech. 2009;22(6):417–421. doi: 10.1097/BSD.0b013e3181870385. [DOI] [PubMed] [Google Scholar]
- 45.Kose K.C., Inanmaz M.E., Isik C., Basar H., Caliskan I. Short segment pedicle screw instrumentation with an index level screw and cantilevered hyperlordotic reduction in the treatment of type-A fractures of the thoracolumbar spine. Bone Joint Lett J. 2014;96-B(4):541–547. doi: 10.1302/0301-620X.96B4.33249. [DOI] [PubMed] [Google Scholar]
- 46.Dobran M., Nasi D., Brunozzi D. Treatment of unstable thoracolumbar junction burst fractures: short-segment pedicle fixation with inclusion of fracture level versus long-term instrumentation. Acta Neurochir. 2016;158(10):1883–1889. doi: 10.1007/s00701-016-2907-0. [DOI] [PubMed] [Google Scholar]
- 47.Sun C., Liu X., Tian J., Guan G., Zhang H. Comparison of unilateral versus bilateral pedicle screw fixation at the level of fracture using posterior short-segment pedicle instrumentation in the treatment of severe thoracolumbar burst fractures. Int J Surg. 2017;41:50–55. doi: 10.1016/j.ijsu.2017.03.055. [DOI] [PubMed] [Google Scholar]
- 48.Alanay A., Acaroglu E., Yazici M., Oznur A., Surat A. Short-segment pedicle instrumentation of thoracolumbar burst fractures: does transpedicular intracorporeal grafting prevent early failure? Spine. 2001;26(2):213–217. doi: 10.1097/00007632-200101150-00017. [DOI] [PubMed] [Google Scholar]
- 49.Toyone T., Ozawa T., Inada K. short-Segment fixation without fusion for thoracolumbar burst fractures with neurological deficit can preserve thoracolumbar motion without resulting in post-traumatic disc degeneration. Spine. 2013;38(17):1482–1490. doi: 10.1097/BRS.0b013e318297bdb7. [DOI] [PubMed] [Google Scholar]
- 50.Pishnamaz M., Curfs I., Balosu S. Two-Nation comparison of classification and treatment of thoracolumbar fractures:an internet-based multicenter study among spine surgeons. Spine. 2015;40(22):1749–1756. doi: 10.1097/BRS.0000000000001143. [DOI] [PubMed] [Google Scholar]
- 51.Korovessis P., Baikousis A., Zacharatos S., Petsinis G., Koureas G., Iliopoulos P. Combined anterior plus posterior stabilization versus posterior short-segment instrumentation and fusion for mid-lumbar (l2–l4) burst fractures. Spine. 2006;31(8):859–868. doi: 10.1097/01.brs.0000209251.65417.16. [DOI] [PubMed] [Google Scholar]
- 52.Defino H.L.A., Scarparo P. Fractures of thoracolumbar spine;monosegmental fixation. Inj Int J Care Inj . 2005;36 doi: 10.1016/j.injury.2005.06.019. S-B90—S-B97. [DOI] [PubMed] [Google Scholar]
- 53.Gotzen L., Puplat D., Junge A. Indications, technique and results of monosegmental dorsal spondylodesis in wedge compression fractures (grade II) of the thoracolumbar spine] Unfallchirurg. 1992;95(9):445-454. [PubMed] [Google Scholar]
- 54.Li X., Ma Y., Dong J. Retrospective analysis of treatment of thoracolumbar burst fracture using mono-segment pedicle instrumentation compared with short-segment pedicle instrumentation. Eur Spine J. 2012;21:2034–2042. doi: 10.1007/s00586-012-2214-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wei F.X., Liu S.Y., Liang C.X., Li H.M. Transpedicular fixation in management of thoracolumbar burst fractures. Spine. 2010;35(15):E714–E720. doi: 10.1097/BRS.0b013e3181d7ad1d. [DOI] [PubMed] [Google Scholar]
- 56.Wang D.M., Shi D.F., Li X.L., Dong J., Wang C.H., Chen S.G. Biomechanical comparison of different pedicle screw fixations for thoracolumbar burst fractures using finite element method. Appl Mech Mater. 2011;117–119:699–702. [Google Scholar]