Abstract
Background
Healthcare professionals (HPs) are the key figures to keep up the healthcare system during the COVID-19 pandemic and thus are one of the most vulnerable groups in this. To this point, the extent of this psychological burden, especially in Europe and Germany, remains unclear. This is the first study investigating German HPs after the COVID-19 outbreak.
Methods
We performed an online-based cross-sectional study after the COVID-19 outbreak in Germany (10–31 March 2020). In total, 2224 HPs (physicians n = 492, nursing staff n = 1511, paramedics n = 221) and 10 639 non-healthcare professionals (nHPs) were assessed including generalized anxiety (Generalized Anxiety Disorder-7), depression (Patient Health Questionnaire-2), current health status (EQ-5D-3L), COVID-19-related fear, subjective level of information regarding COVID-19.
Results
HPs showed less generalized anxiety, depression and COVID-19-related fear and higher health status and subjective level of information regarding COVID-19 than the nHPs. Within the HP groups, nursing staff were the most psychologically burdened. Subjective levels of information regarding COVID-19 correlated negatively with generalized anxiety levels across all groups. Among HPs, nursing staff showed the highest and paramedics the lowest generalized anxiety levels.
Conclusions
In the context of COVID-19, German HPs seem to be less psychological burdened than nHPs, and also less burdened compared with existing international data.
Keywords: COVID-19, generalized anxiety, healthcare professionals, information, psychological burden
Introduction
The COVID 19 pandemic reached Germany in late February 2020. It brought not only objective medical challenges for healthcare professionals (HPs), but also reports and findings from other more affected countries. Due to exponentially increasing case numbers and large numbers of patients requiring intensive care, those more affected countries are facing unexpected challenges. Countries such as China, Italy, Spain, Brasil and the USA were and are currently reaching the limits of their healthcare systems in the context of this pandemic: something that was previously unimaginable in industrialized countries.1 Such a development seems to have been avoided in Germany but is not completely ruled out for the future.
In the face of an ever-renewing European and a further worldwide escalation, there is no shortage of uncertainty and concern among HPs. It is already known from countries other than Germany that HPs are under elevated psychological stress during the COVID-19 pandemic and show increased levels of various psychometric values, including anxiety and depression.2–5 Existing evidence, e.g. from China, already shows the extent of the psychological burden on HPs. Front-line healthcare workers were identified as bearing a particularly heavy psychological burden.2,6 However, these studies were conducted during the extreme stress phase of the COVID-19 epidemic in China. Only few data in the context of other studies suggest that, e.g. in the UK, a heightened psychological burden for the HPs may exist.7 There is, as yet no comparable data, especially from a time when the health system is still mainly coping normally, alongside already population-wide uncertainty, particularly in Europe.
The German situation to this point is 2-fold: Continuing and past restrictions in public life, contact restrictions, empty supermarket shelves and daily updated increasing case numbers are still coupled with a hospital system that is and was largely still able to cope normally. This is combined with mortality rates, which are, for the moment, low when compared internationally.8,9 Though, the German population shows itself already burdened in terms of generalized anxiety, depression and distress, which is in line with evidence from other countries,10,11 customized low-threshold interventions, offline as well as online, are needed and already implemented.12–14 The aim of this study was to close the research gap and provide initial findings on psychological burden of German HPs after the COVID-19 outbreak.
It is hypothesized that the group of HP in Germany will mirror the existing, population-wide elevated psychological burden15 to an even greater extend by being in the ‘front line’, as already could be observed in previous studies in other countries.2,3
Methods
Study design, setting and participants
A nationwide, online-supported cross-sectional survey was conducted. Participants were recruited via online channels and official channels e.g. websites of clinics. The survey period was from the 10–31 March 2020. It was during this period that the first increased numbers of COVID-19 cases in Germany, increasingly restrictive government regulations, the closure of European borders and the restriction of individual freedoms occurred. In total, 12 863 people completed the questionnaire, of which we identified 2224 people in the medical sector as HPs and 10 639 as non-healthcare professionals (nHPs). HPs were from three different groups: physicians, nursing staff and paramedics. The sample description can be seen in Table 1. All participants gave their written consent to participate in the survey and the evaluation of the collected data. The study was conducted in accordance with the ethical guidelines from the Declaration of Helsinki and was approved by the local ethics committee of the faculty of medicine.
Table 1.
Sample description
| Physicians (n = 492) | Nursing staff (n = 1511) | Paramedics (n = 221) | nHPs (n = 10 639) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Gender | Female | 323 | 65.65 | 1312 | 86.83 | 55 | 24.89 | 7474 | 70.25 |
| Male | 168 | 34.15 | 197 | 13.04 | 164 | 74.21 | 3131 | 29.43 | |
| Divers | 1 | 0.20 | 2 | 0.13 | 2 | 0.90 | 34 | 0.32 | |
| Residence | City | 337 | 68.50 | 758 | 50.17 | 79 | 35.75 | 6247 | 58.71 |
| Medium-sized city | 98 | 19.92 | 382 | 25.28 | 67 | 30.32 | 2404 | 22.59 | |
| Small town | 31 | 6.30 | 180 | 11.91 | 42 | 19.00 | 1059 | 9.95 | |
| County | 26 | 5.28 | 191 | 12.64 | 33 | 14.93 | 931 | 8.75 | |
| Risk group | Yes | 84 | 17.07 | 365 | 24.16 | 50 | 22.62 | 2395 | 22.51 |
| No | 408 | 82.93 | 1146 | 75.84 | 171 | 77.38 | 8244 | 77.49 | |
| Mental illness | Yes | 19 | 3.84 | 159 | 10.52 | 14 | 6.33 | 1430 | 13.44 |
| No | 476 | 96.16 | 1352 | 89.48 | 207 | 93.67 | 9209 | 86.56 | |
| Place of work (physician) | Clinic | 312 | 63.41 | ||||||
| Outpatient | 142 | 28.86 | |||||||
| Other | 38 | 7.72 | |||||||
Note: Risk group indicates whether the participant belonged to one of the risk groups for a severe course of COVID-19 (cardiovascular disease, diabetes mellitus, chronic respiratory disease, cancer).
Instruments
Details of general socio-demographic variables were asked. Validated psychometric instruments were used to assess psychological burden. The Generalized Anxiety Disorder-7 (GAD-7) to measure generalized anxiety symptoms over the course of the last 2 weeks (GAD-7, 7 items, 4-point Likert Scale meaning 0 = never to 3 = nearly every day),16 the Patient Health Questionnaire-2 (PHQ-2) to screen for depression symptoms over the course of the last 4 weeks (PHQ-2, 2 items, 4-point Likert Scale meaning 0 = never to 3 = nearly every day)17 and the visual analogous scale of the EuroQol EQ-5D-3L scale to assess current health status (ranging from 0 [worst imaginable health status] to 100 [best imaginable health status]).18 Additionally, based on scientific and media reports, multiple items and item scales were formed in expert consensus with regard to ‘COVID-19-related fear’ (one item, 7-point Likert scale meaning 1 = very low to 7 = extremely high), ‘the subjective level of information regarding COVID-19’ (3 items: I feel informed about COVID-19; I feel informed about measures to avoid an infection with COVID-19; I understand the health authorities’ advice regarding COVID-19. Seven-point Likert scale, meaning 1 = complete disagreement to 7 = complete agreement). Scale reliability for was tested using Cronbach’s α for internal consistency. ‘The subjective level of information regarding COVID-19’ showed high internal consistency (Cronbach’s α = 0.801).
Data analysis
The descriptive and inferential statistics were performed with R3.6.1 (R Core Team, 2019). Sum scores for the GAD-7 and PHQ-2 and mean scores for all other scales were calculated.
To assess the hypotheses, the 95% confidence of the association measures are reported; for each difference between the groups after having assessed the global mean difference in the respective scale. Hence, the assumptions were assessed based on their precision.19–21 Generally, test statistics and P values are not reported given that at this sample size even the slightest deviation from equivalence results in extremely low P values. When the confidence interval (CI) of the effect size covers 0, we assume there is no effect. As soon as this is the case, we use the guidelines by Sawilowsky22 to evaluate the importance of the effect; a Cohen’s d ~0.2 is considered a small, a d ~0.5 is considered medium-sized and d ~0.8 is regarded as large effects.
Due to the large sample size and the intuitive and common interpretation of the effect sizes, parametric methods were also used for violation of the normality assumption.23 For mean comparisons Welch’s t-test with the Cohen’s d association measure was used, for multiple mean comparisons and between-subject analysis of variance with the association measure η2 with subsequent t-tests for post hoc comparisons with Tukey error correction. A complete summary of all post hoc group comparisons after calculation of the variance analyses and post hoc tests can be assessed in the supplementary materials.
To clear the association of subjective level of information regarding COVID-19 and other variables, Spearman correlations between variables were performed. To subsequently test the interdependence of variables a robust linear M-estimator regression was performed (rlm from the R package MASS, 2002). All Spearman correlations including confidence between the measures are provided in the supplemental material.
Following the results of the correlation analyses, prevalence ratios for the amount of participants with moderate generalized anxiety in relation to the subjective level of information regarding COVID-19 were explored. Levels of generalized anxiety were divided by using the GAD-7 sum score of ≥1024 as a split into low levels of generalized anxiety (<10) and moderate to high levels of generalized anxiety (≥10). This was compared with a pre-COVID-19 standard population, where 5.9% of the population scored above ≥10.25 The subjective level of information regarding COVID-19 was split by the median into high (≥median) and low (<median) levels. Prevalence ratios were calculated using unconditional maximum likelihood. CIs were calculated using normal approximation (via the R-packages epitools, 2020).
Results
Concerning generalized anxiety measured by the GAD-7, differences between the different HP groups and between the HPs and the nHPs could be found (η2 = 0.009, CI = [0.006–0.013]) see fig. 1. Physicians show less generalized anxiety than nursing staff and the nHPs (physicians versus nursing staff: d = −0.213, CI = [−0.315 to −0.111] physicians versus nHPs: d = −0.342, CI = [−0.432 to −0.251]). Nursing staff show the highest generalized anxiety of all HPs. They also trend toward lower anxiety scores than the nHPs, effect sizes are relatively small (nursing staff versus nHPs: d = 0.129, CI = [0.075–0.182]). Descriptively paramedics show the lowest generalized anxiety, although they do not differ from physicians in the direct comparison (paramedics versus physicians: d = 0.148, CI = [−0.011 to 0.306]).
Fig. 1.
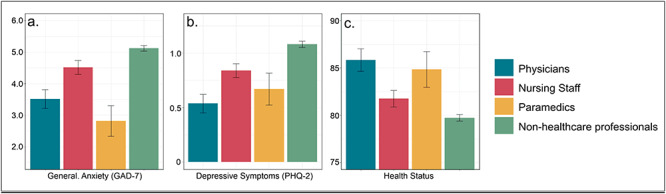
Representation of the different manifestations of generalized anxiety (GAD-7) (a), depression (PHQ-2) (b), health status (c). Bars represent mean individual sum scores for GAD-7 and PHQ-2 and means for health status. Error bars represent 95% CIs. Note: GAD-7: 4-point Likert scale from 0 = never to 3 = nearly every day; PHQ-2: 4-point Likert scale from 0 = never to 3 = nearly every day; health status (EQ-5D-3L): visual analogous scale from 0 (worst imaginable health status) to 100 (best imaginable health status).
Depression, measured by the PHQ-2, also shows differences between the different HP groups and between the HPs and the nHPs (η2 = 0.009, CI = [0.006–0.012]) fig. 1. Physicians show lower depression scores than nursing staff and the nHPs (physicians versus nursing staff: d = −0.21, CI = [−0.312 to −0.108]; physicians versus nHPs: d = −0.377, CI = [−0.468 to −0.287]). Nursing staff and paramedics show lower depression scores than the nHPs, although the paramedics differ in a more pronounced manner (nursing staff versus nHPs: d = 0.167, CI = [0.113–0.221], paramedics versus nHPs: d = 0.285, CI = [0.152–0.418]). There are neither differences between paramedics and physicians, nor between paramedics and nursing staff (all CIs covering 0).
Physicians and paramedics show, comparatively to nursing staff and the nHPs, the best health status. Both differ from the nHPs (η2 = 0.007, CI = [0.00039–0.0094]; physicians versus nHPs: d = 0.345, CI = [0.254–0.435], paramedics versus nHPs: d = −0.289, CI = [−0.423 to −0.156]). Nursing staff slightly differ from paramedics (d = −0.174, CI = [−0.315 to −0.033]), whereas the difference between nursing staff and physicians is relatively more pronounced (d = 0.23, CI = [0.128–0.332]). Physicians do not differ from paramedics (d = 0.056, CI = [−0.103 to 0.214]). Nursing staff, thus, show a lower health status than physicians and paramedics, but the health status of nursing staff is rated hardly better than that of the nHPs (d = −0.115, CI = [−0.169 to −0.061]) fig. 1.
COVID-19-related fear could be found among HPs and the nHPs. HPs show less COVID-19-related fear than the nHPs (all ds > 0.2 with CIs not including 0). Physicians and nursing staff show a similar level (η2 = 0.01, CI = [0.008–0.015]; d = −0.003, CI = [−0.105 to 0.10.]) Paramedics in particular show a lower level of COVID-19-related fear than physicians and nursing staff (paramedics versus physicians: d = 0.414, CI = [0.255–0.573]; paramedics versus nursing staff: d = 0.417, CI = [0.276–0.558]) see fig. 2.
Overall, the participants report a high level of subjective level of information regarding COVID-19, the mean values of all groups (HPs and nHPs) were >5.5. Existing differences between nursing staff and physicians, as well as nursing staff and the nHPs, of which the CIs deviate from 0, remain negligible (nursing staff versus physicians: d = 0.07, CI = [0.011–0.129], nursing staff versus nHPs: d = 0.046, CI = [0.015–0.077]) fig. 2.
Subjective level of information regarding COVID-19 correlates with generalized anxiety. The association of high or low subjective levels of information regarding COVID-19 and low or moderate to high generalized anxiety (cutoff of ≥10) is shown in Table 2. The proportion of moderately anxious participants regardless of level of information is 15.99% in the nHPs, 4.25% in physicians, 11.41% in nursing staff and 4.55% in paramedics.
Table 2.
Generalized anxiety and subjective level of information regarding COVID-19 across the different groups
| Profession | Generalized anxiety below cutoff (GAD-7 < 10) | Generalized anxiety above cutoff (GAD-7 ≥ 10) | % above cutoff | Prevalence ratio | |
|---|---|---|---|---|---|
| Physicians | Low level of information | 170 | 16 | 8.60 | 0.494 |
| High level of information | 293 | 13 | 4.25 | 95% CI [0.243–1.00] | |
| Total | 463 | 29 | 5.89 | ||
| Nursing staff | Low level of information | 569 | 98 | 14.69 | 0.599 |
| High level of information | 767 | 74 | 8.80 | 95% CI [0.451–0.80] | |
| Total | 1336 | 172 | 11.41 | ||
| Paramedics | Low level of information | 95 | 5 | 5.00 | 0.833 |
| High level of information | 115 | 5 | 4.16 | 95% CI [0.238–2.80] | |
| Total | 210 | 10 | 4.55 | ||
| nHPs | Low level of information | 3556 | 771 | 17.82 | 0.835 |
| High level of information | 5373 | 929 | 14.88 | 95% CI [0.766–0.911] | |
| Total | 8929 | 1700 | 15.99 | ||
| In total | Low level of information | 4390 | 891 | 16.87 | 0.807 |
| High level of information | 6550 | 1032 | 13.61 | 95% CI [0.743–0.876] | |
| Total | 10 940 | 1923 | 14.95 |
Note: Prevalence ratio presented for the presence of at least moderate generalized anxiety symptoms (≥10) as a function of the subjective feeling of information regarding COVID-19. Subjective level of information is split across the median in high (≥6) and low (≤6) levels. GAD-7, sum scores of ≥5, ≥10 and ≥15 indicate mild, moderate and severe generalized anxiety symptoms.
Fig. 2.
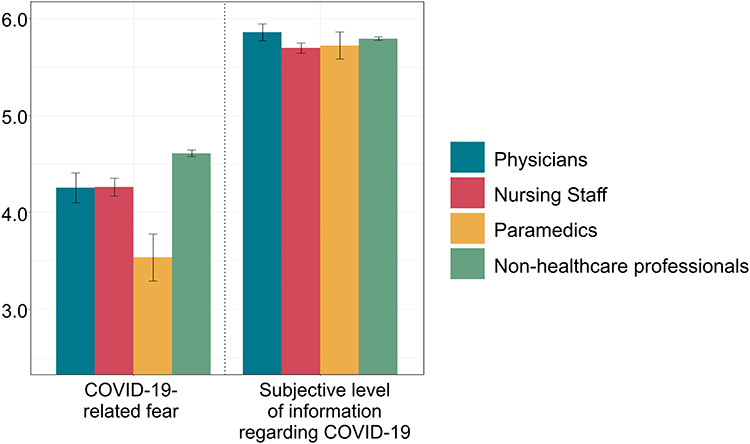
Representation of the different characteristics of COVID-19-related fear and subjective level of information regarding COVID-19. Bars represent mean values of COVID-19-related fear and the means of the individual sum scores of the subjective level of information regarding COVID-19. Error bars represent 95% CIs. Note: COVID-19-related fear: one item, 7-point Likert scale meaning 1 = very low to 7 = extremely high; subjective level of information regarding COVID-19 (three items: I feel informed about COVID-19; I feel informed about measures to avoid an infection with COVID-19; I understand the health authorities' advice regarding COVID-19. Seven-point Likert scale, meaning 1 = complete disagreement to 7 = complete agreement).
The probability of reaching the pathological GAD-7 cutoff score of ≥10 thus diminishes across almost all HP groups and the nHPs with the degree of subjective level of information regarding COVID-19 (Fig. 3). For physicians, nursing staff and others, the prevalence of having generalized anxiety when sufficiently informed is critically reduced (with CIs of the prevalence ratio deviating significantly from 1). However, reduced moderate generalized anxiety in participants with high subjective levels of information can also observed when the sample is analyzed as a whole.
Fig. 3.
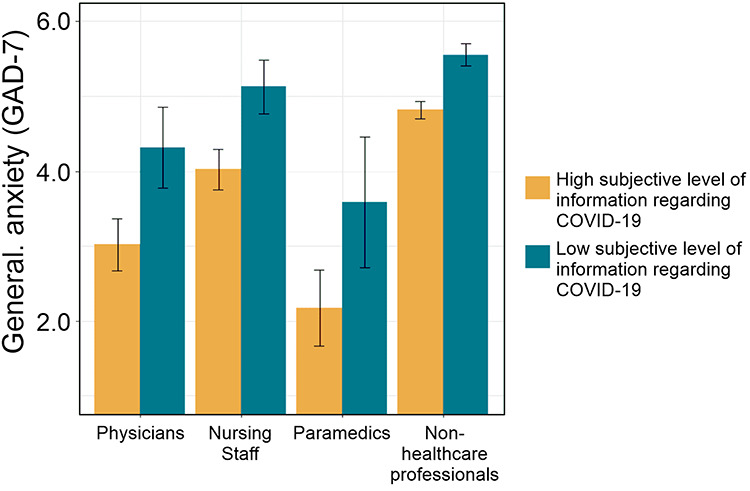
Generalized anxiety (GAD-7) as a function of subjective level information regarding COVID-19 split by the median into high level (≥median ) and low level (< median) of subjective level of information. Bars represent means of the sum scores of the GAD-7. Error bars represent 95% CIs. Note: GAD-7: 4-point Likert scale from 0 = never to 3 = nearly every day; subjective level of information regarding COVID-19 (three items: I feel informed about COVID-19; I feel informed about measures to avoid an infection with COVID-19; I understand the health authorities' advice regarding COVID-19. Seven-point Likert scale, meaning 1 = complete disagreement to 7 = complete agreement).
Discussion
Main findings of the study
Assessing the psychological burden and COVID-19-related concerns of people working in the healthcare system is of high relevance in the light of the COVID-19 pandemic events. To this point, this study is the first to assess those points in the German healthcare system.
In this study, nHPs reported overall higher levels of psychological burden than the HPs, which is particularly pronounced in generalized anxiety and depression scores. Within the HP groups there was, in relative terms, less psychological burden on physicians and paramedics than on nursing staff. Health status was better in the HP groups and within those, physicians reported the best health status, followed by paramedics. HPs also showed less COVID-19-related fear than nHPs, paramedics showing the least fear. Subjective levels information regarding COVID-19 was high overall HPs and nHPs. High levels of subjective levels of information regarding COVID-19 correlated negatively with high levels of generalized anxiety symptoms globally. In the group of individuals with low subjective levels of information regarding COVID-19, 17.88% of the nHPs, 8.60% of the physicians, 14.69% of the nursing staff and 5.00% of the paramedics scored above the cutoff of ≥10, indicating the presence of GAD symptoms. Even without the division in subjective levels of information regarding COVID-19, still 15.99% of the nHPs, 5.89% of the physicians, 11.41% of the nursing staff and 4.55% of the paramedics scored above this cutoff. Especially concerning the nHPs and the nursing staff, this is a massive elevation of prevalence in comparison to a pre-COVID-19 sample, where only 5.9% of the population scored above this cutoff.25
What is already known on this topic
The psychological burden of HPs during the COVID-19 pandemic has already been investigated in the early hotspots of the pandemic, especially in China and Southeast Asia. High psychological burden of front-line workers could be found in China4–6,26 and other countries (e.g. Tan et al.3). In detail, at the height of the crisis in China, 50.7% of healthcare workers showed symptoms of depression, 44.7% those of generalized anxiety and 73.4% showed increased stress symptoms.27 The psychological response of HPs during epidemics has already been investigated during other virus outbreaks, e.g. SARS and H1N1, drawing similar pictures.28,29 A clear picture concerning the HPs in Europe, especially in the beginning of the virus outbreak still does not exist.
What this study adds
In the present study, it was possible to show a rare picture of a healthcare system in the early outbreak stages of a pandemic in the western world. During this phase of the outbreak in Germany, in which uncertainty and anxiety prevailed but COVID-19 cases and death rates were still moderate and low, HPs were less psychologically burdened than the nHPs and less psychologically burdened than comparable HP groups in other countries.3–6,26 This poses the question why the German HPs coped and cope so well in the light of the current pandemic and in comparison to the nHPs. The finding that physicians in the current situation are among the least burdened by generalized anxiety and depression can maybe be understood by the fact that generalized anxiety was most correlated with the subjective level of information regarding COVID-19. This may explain why physicians and HPs show lower overall levels of generalized anxiety and COVID-19-related fear, which also is in line with findings from Tan et al.3 where nonmedical healthcare workers had higher prevalence of anxiety than medical healthcare workers. This, in a second step, points to the inevitable need for the population to be informed transparently and evidence based in order to experience the COVID-19 pandemic with a low level of fear as possible.15,30 The present findings of this study also urge especially western countries to conduct still more research concerning the psychological burden of their HPs. Existing literature is majorly consisting of studies from Southeast Asia and during the early, dramatic scenes of the pandemic. To meet the needs of the HPs, especially as soon as the situation worsens again or a much feared ‘second wave’ hits Europe, the mental health of HPs will have to be given high priority in supporting measures.31
Limitations of this study
Limitations need to be considered. Data were obtained via an anonymous online, self-reported questionnaire in a cross-sectional study design. A potential selection bias may exist. During the short survey period, a series of various governmental restrictions were put into place, which may represent different manifestations of psychological states at different points in time. Data were acquired during a rather early period of the outbreak, which poses the risk of an under- or even overestimation of psychological burden. On the other hand, this exceptional early assessment period might be a major strength of posed study—a thus large sample as the present on the beginning of the current outbreak is scarce and adds a piece to the COVID-19 puzzle in order to gain a clearer picture of the unprecedented COVID-19 pandemic.
Conclusion
In conclusion, HPs in Germany show less psychological burden compared with HPs in other countries and compared with the general population in Germany after the outbreak of COVID-19. In the investigated sample, nursing staff seems to be the most vulnerable group for mental health burden during the COVID-19 pandemic, whereas a high subjective level of information seems to be associated with less psychological burden.
Funding
This study was supported by the Essen University Medicine Foundation. The funder had no role in the design and conduct of the study; management, collection, analysis and interpretation of the data; preparation, review or approval of the manuscript and decision to submit the manuscript for publication.
Declaration of competing interest
The authors declare that they have no competing interests.
Supplementary Material
Eva-Maria Skoda, Head of Research
Martin Teufel, Director
Andreas Stang, Head of Department
Karl-Heinz Jöckel, Deputy Head of Department
Florian Junne, Deputy Head of Department
Benjamin Weismüller, Senior Researcher
Madeleine Hetkamp, Researcher
Venja Musche, Researcher
Hannah Kohler, Researcher
Nora Dörrie, Head of Outpatient Clinic
Adam Schweda, Data Scientist
Alexander Bäuerle, Deputy Head of Research
References
- 1. Saglietto A, D'Ascenzo F, Zoccai GB et al. . COVID-19 in Europe: the Italian lesson. Lancet 2020;395:1110–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lai J, Ma S, Wang Y et al. . Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 2020;3(3):e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tan BYQ, Chew NWS, Lee GKH et al. . Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med 2020. doi: 10.7326/M20-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wang C, Pan R, Wan X et al. . Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 2020;17(5):1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wang C, Pan R, Wan X et al. . A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun 2020;87:40–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kang L, Ma S, Chen M et al. . Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun 2020;87:11–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Moorthy A, Sankar TK. Emerging public health challenge in UK: perception and belief on increased COVID19 death among BAME healthcare workers. J Pub Health (Oxf) 2020; fdaa096 10.1093/pubmed/fdaa096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Koch-Institut Robert. Täglicher Lagebericht des RKI Zur Coronavirus-Krankheit-2019 (COVID-19). Berlin: Robert Koch-Institut; 2020:1–8. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/2020-03-30de.pdf;jsessionid=EF3675948EF9BC39CCAD855DDA838D46.internet061?__blob=publicationFile. (23 June 2020, date last accessed). [Google Scholar]
- 9. Bedford J, Enria D, Giesecke J et al. . COVID-19: towards controlling of a pandemic. Lancet 2020;395(10229):1015–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bäuerle A, Teufel M, Musche V et al. . Increased generalized anxiety, depression, and distress during the COVID-19 pandemic: a cross-sectional study in Germany. J Pub Health 2020. doi: 10.1093/pubmed/fdaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr 2020;52:102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bäuerle A, Skoda E-M, Dörrie N et al. . Psychological support in times of COVID-19: the Essen community-based CoPE concept. J Public Health (Oxf) 2020;fdaa053. doi: 10.1093/pubmed/fdaa053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bäuerle A, Graf J, Jansen C et al. . An e-mental health intervention to support burdened people in times of the COVID-19 pandemic: CoPE It. J Public Health (Oxf) 2020;fdaa058. doi: 10.1093/pubmed/fdaa058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Benecke A, Bäuerle A, Jansen C et al. . Techniques, methods, and dissemination of community based psychological support strategies in times of the COVID-19-pandemic. J Prim Care Community Health 2020. doi: 10.1177/2150132720943328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Teufel M, Schweda A, Dorrie N et al. . Not all world leaders use twitter in response to the COVID-19 pandemic: impact of the way of Angela Merkel on psychological distress, behaviour and risk perception. J Public Health (Oxf). 2020. doi: 10.1093/pubmed/fdaa060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Löwe B, Decker O, Muller S et al. . Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care 2008;46(3):266–74. [DOI] [PubMed] [Google Scholar]
- 17. Löwe B, Kroenke K, Grafe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J Psychosom Res 2005;58(2):163–71. [DOI] [PubMed] [Google Scholar]
- 18. EuroQol G. EuroQol--a new facility for the measurement of health-related quality of life. Health Policy 1990;16(3):199–208. [DOI] [PubMed] [Google Scholar]
- 19. Lash TL. Heuristic thinking and inference from observational epidemiology. Epidemiology 2007;18(1):67–72. [DOI] [PubMed] [Google Scholar]
- 20. Sterne JA, Davey Smith G. Sifting the evidence-what's wrong with significance tests? BMJ 2001;322(7280):226–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wasserstein RL, Schirm AL, Lazar NA. Moving to a world beyond “p < 0.05”. Am Stat 2019;73:1–19. [Google Scholar]
- 22. Sawilowsky SS. New effect size rules of thumb. J Mod Appl Stat Methods 2009;8(2):597–9. [Google Scholar]
- 23. Lumley T, Diehr P, Emerson S et al. . The importance of the normality assumption in large public health data sets. Annu Rev Public Health 2002;23:151–69. [DOI] [PubMed] [Google Scholar]
- 24. Spitzer RL, Kroenke K, Williams JB et al. . A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166(10):1092–7. [DOI] [PubMed] [Google Scholar]
- 25. Hinz A, Klein AM, Brahler E et al. . Psychometric evaluation of the Generalized Anxiety Disorder Screener GAD-7, based on a large German general population sample. J Affect Disord 2017;210:338–44. [DOI] [PubMed] [Google Scholar]
- 26. Kang L, Li Y, Hu S et al. . The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry 2020;7(3):e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Liu S, Yang L, Zhang C et al. . Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry 2020;7(4):e17–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chong MY, Wang WC, Hsieh WC et al. . Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br J Psychiatry 2004;185:127–33. [DOI] [PubMed] [Google Scholar]
- 29. Maunder RG, Lancee WJ, Balderson KE et al. . Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis 2006;12(12):1924–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Jones DS. History in a crisis - lessons for COVID-19. N Engl J Med 2020;382:1681–3. [DOI] [PubMed] [Google Scholar]
- 31. Xiang YT, Yang Y, Li W et al. . Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020;7(3):228–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


