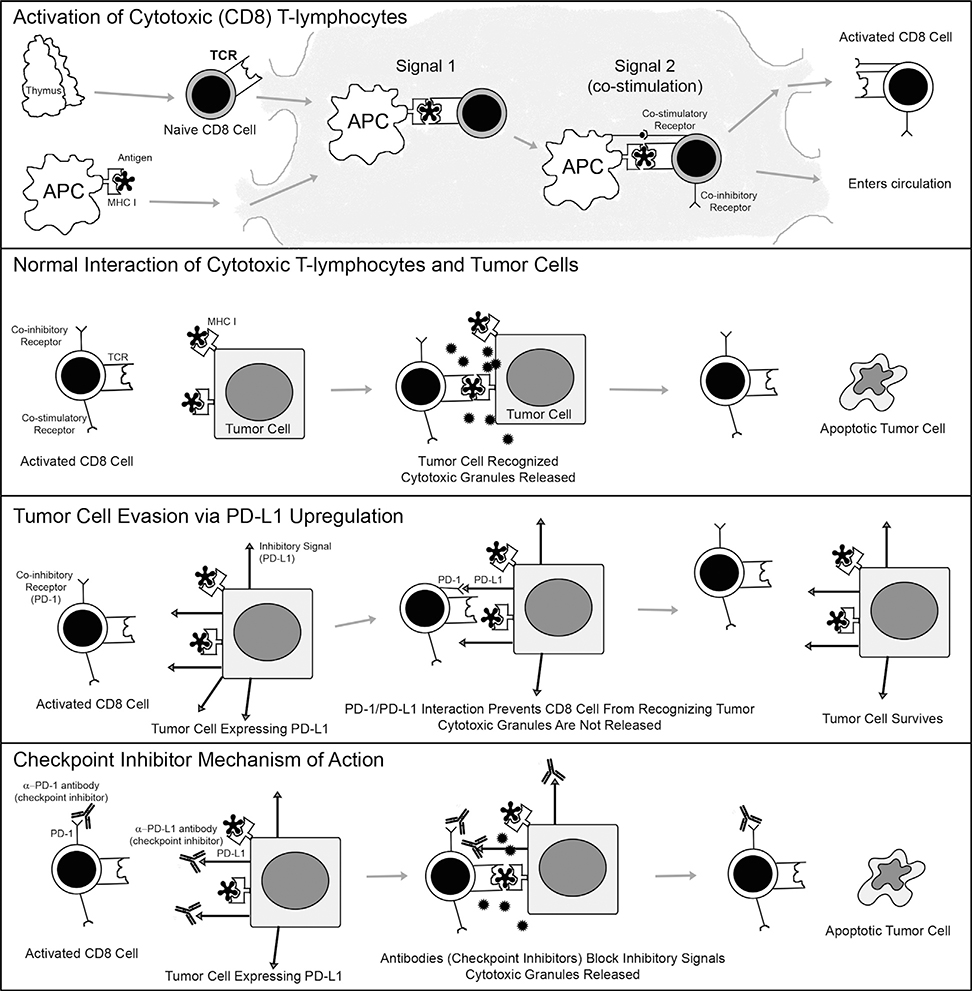
FIGURE 3.
Mechanism of action of the normal PD-1/PD-L1 system, its dysregulation during neoplasia, and its normalization with checkpoint inhibitor drugs. (Top panel) This panel illustrates how normal cytotoxic T lymphocytes become activate. Naïve (unactivated) CD8-positive T lymphocytes expressing T-cell receptors (TCR) on their surfaces exist the thymus and migrate to lymph nodes for activation. Antigen presenting cells (APCs) scavenge antigens throughout the body. They engulf both foreign and endogenous antigens, process them into smaller pieces, and then load them onto major histocompatibility complex class I (MHC I) proteins so that the antigens may be optimally displayed on their surfaces. APCs migrate to lymph nodes. In the lymph nodes, naïve T cells may recognize antigens presented to them by APCs; the TCR interacts with the antigen and MHC I. This type of interaction is known as “signal 1”; a second signal, however, in the form of co-stimulatory signals is needed in order for the naïve T lymphocyte to become activated; without it it will become anergic. Once a co-stimulatory interaction (“signal 2”) is provided, the T lymphocyte is activated. Soon after activation it upregulates co-inhibitory receptors (such as CTLA-4 and PD-1). These co-inhibitory receptors are intended as sites where the activation can be dampened so that autoimmunity is avoided. Activated CD8 lymphocytes, expressing co-inhibitory receptors such as PD-1, then multiply and exit the lymph node into the circulation, in search of cells expressing their target antigens. (Second panel) This panel illustrates the normal action of CD8 T lymphocytes against tumor cells. Activated CD8 T lymphocytes use their TCRs to recognize tumor cells that express MHC I with target antigens on their surfaces. The interaction of the TCR with the MHC I and antigen reads to release of cytotoxic granules from CD8 T lymphocytes, which trigger apoptosis in the tumor cell. The tumor cell is killed, while the CD8 T lymphocyte remains intact and ready to find another target cell. (Third panel) This panel illustrates how tumor cells evade CD8 T lymphocytes by usurping the normal checkpoint PD-1/PD-L1 system. Some tumor cells upregulate inhibitory ligands such as PD-L1 on their surfaces. When an activated T lymphocyte attempts to bind to a tumor cell that expresses the target MHC I and antigen on its surface, PD-L1 interacts with the inhibitory receptor PD-1 on the surface of the T lymphocyte. This PD-1/PD-L1 interaction is called a “checkpoint,” and it prevents the T cells from releasing its cytotoxic granules and from killing the tumor cell. The tumor cell survives, while often the T lymphocyte becomes anergic. (Bottom panel) This panel illustrates how checkpoint inhibitor drugs work to allow CD8 T lymphocytes to find and kill tumor cells, even when they express PD-L1 on their surfaces. Checkpoint inhibitors are monoclonal antibodies that bind to either PD-1 receptors on the surfaces of T lymphocytes, or to PD-L1 on the surfaces of tumor cells. Either drug leads to disruption of the PD-1/PD-L1 interaction, interfering with the inhibitory signal, and thereby allowing the CD8 T lymphocyte to recognize the tumor cell. The CD8 T lymphocyte is able to release cytotoxic granules and once again trigger apoptosis of the targeted tumor cell, as originally intended.