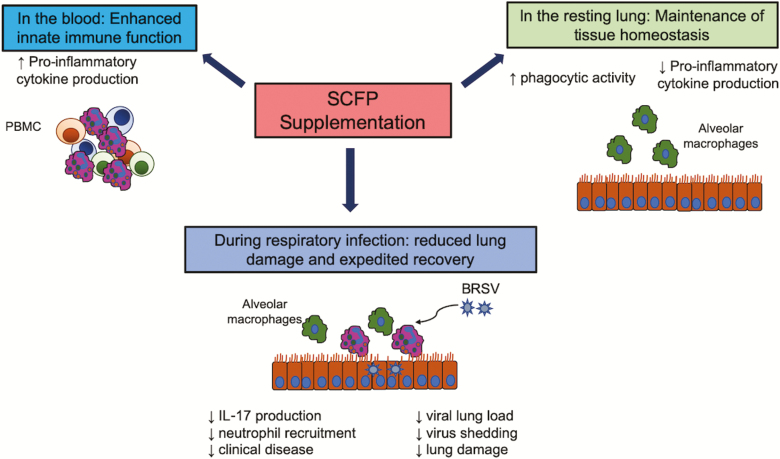
Figure 11.
Our proposed model for the effects of SCFP treatment on immune function in the periphery and lung tissue. The results of our studies suggest that SCFP supplementation differentially modulates immune function in the periphery and lung tissue. In the blood, SCFP treatment results in enhanced innate immune function. Circulating PBMCs have an increased capacity to secrete proinflammatory cytokines, suggesting that they are poised to respond more robustly to an infection or insult. The essential function of the lung is air exchange. Exacerbated inflammation causes tissue damage and interferes with lung function; therefore, immune responses in the mucosa must be carefully controlled. In the current study, SCFP treatment resulted in reduced proinflammatory cytokine secretion following TLR stimulation but increased the capacity of alveolar macrophages to phagocytose particles, suggesting that they may have improved capacity to eliminate invading pathogens or particulates. SCFP treatment during BRSV infection resulted in less clinical disease, less neutrophil recruitment, less lung pathology, and reduced virus shedding.