Abstract
Patient: Male, 84-year-old
Final Diagnosis: Acute bronchitis • chronic multiple pain with spondylosis with radiculopathy: lumbar region • chronic renal failure CKD 4 • derailed type 2 diabetes mellitus • diabetes mellitus type 2 • eart failure • hyperuricaemia • progressive aortic stenosis • pulmonary hypertension • SARS-CoV2
Symptoms: Appetite loss • fever • pain • sore throat
Medication: —
Clinical Procedure: —
Specialty: General and Internal Medicine
Objective:
Unusual clinical course
Background:
When treating patients with comorbidities who are infected with severe acute respiratory syndrome as a result of SARS-CoV-2, it is crucial to offer multidisciplinary treatment that takes into consideration all of the health conditions with which they have been diagnosed. In particular, clinicians should not lose sight of the patient experience, which we can be assessed with the help of patient-reported outcomes (PROs).
Case Report:
An 84-year-old man infected with SARS-CoV-2 was already suffering from multiple health conditions, including Type 2 diabetes mellitus. He most likely was receiving cortisone therapy and had chronic pain with spondylosis with radiculopathy, bilateral gonarthrosis following total knee replacement, malaise, and fatigue.
The patient received acute inpatient care in a hospital that provides complementary medical therapies. We collected clinical and patient-reported data on quality of life, physical functions, the sensation of pain, psychological well-being, and symptoms while taking into account the degree of chronicity of the conditions, the level of the patient’s pain, and his hospitalization in an isolation ward. We stabilized clinical parameters related to the patient’s main underlying health conditions (blood glucose and pain levels and oxygen saturation). The PROs we collected demonstrated a significant improvement on discharge.
Conclusions:
Applying PROs can be helpful in obtaining a more comprehensive picture of a patient with COVID-19, in which “the patient is given a voice,” in addition to being assessed by others. The knowledge gained can then be made available to the interdisciplinary treatment team to be incorporated into the treatment plan.
MeSH Keywords: Chronic Disease, Comorbidity, COVID-19, Patient Care, Quality of Life
Background
SARS-CoV-2 is rapidly spreading worldwide, causing COVID-19. Groups at higher risk for complications and death due to COVID-19 include older people and patients with pre-existing conditions, such as cardiovascular disease, diabetes mellitus (DM), and hypertension [1–4]. The fact that care for patients with multiple chronic conditions is still insufficient, as was pointed out several years ago, further aggravates the situation [5]. Moreover, the diagnosis-related groups (payment) system does not yet fully reflect the importance of considering comorbidities, which are defined as conditions linked to the index condition and/or typically coexisting conditions [6], although the creation of complex treatment groups alleviates this problem [7]. However, the evidence varies as to how to treat patients with comorbidities and/or multiple morbidities who have more than 1 chronic condition [6].
Many patients with comorbidities who are infected with SARSCoV-2 require treatment in an isolation unit. To date, only a few studies have focused on the experience of these individuals. A recent study by Liu et al. examined the mental well-being of patients with COVID-19 following treatment [8]. However, further research is needed because little information about the state of health has come directly from patients. Our objective here was to obtain data on COVID-19 patients with multiple health conditions who did not require invasive mechanical ventilation.
We wanted to collect PROs when a patient was admitted to an isolation unit for acute inpatient care and then was discharged from the hospital. PROs reflect the patient’s health status as reported directly by that individual, rather than by the clinician [9]. These outcomes include physical function, mental and physical well-being, pain intensity, and symptoms associated with pain. Our aim also was to collect information on pain chronicity and quality of life (QoL), as well as to assess key clinical parameters in the context of the infection.
This was a retrospective analysis of the reported PROs at admission and discharge of an 84-year-old patient with comorbidities who was infected with SARS-CoV-2. His diagnoses were verified by specialists and coded according to the International Classification of Diseases (ICD). The patient was treated in Germany in a general acute care hospital that offers complementary medical therapies. He gave his written consent to participate in this study and had the right to withdraw consent for collection of his data at any time. He was treated by specialists in general internal medicine who had additional qualifications in nephrology and with a focus on alternative medicine; other ward physicians; physiotherapists; and very broadly-trained nursing staff with many years of experience in alternative medicine. The patient refused intensive medical care. His written advance directives are available.
Case Report
The patient was admitted for acute inpatient treatment after experiencing fever as high as 38°C, cough, sore throat, poor appetite, and uncontrolled blood glucose levels up to 500 mg/dL to 600 mg/dL for several days. The patient had dyspnea on light exertion when performing day-to-day tasks at home. He had a history of New York Heart Association (NYHA) Class 2 chronic heart failure. In addition, he had Type 2 DM (T2DM), most likely was receiving cortisone therapy, and had chronic pain with spondylosis with radiculopathy; bilateral gonarthrosis, which had occurred after total knee replacement; malaise; and fatigue. The patient’s general condition had steadily deteriorated and he complained of pronounced weakness and excessive sleepiness. Moreover, he had pain in his knees that was immobilizing and a chronic pain syndrome with back and joint pain. Figure 1 lists the patient’s confirmed diagnoses.
Figure 1.
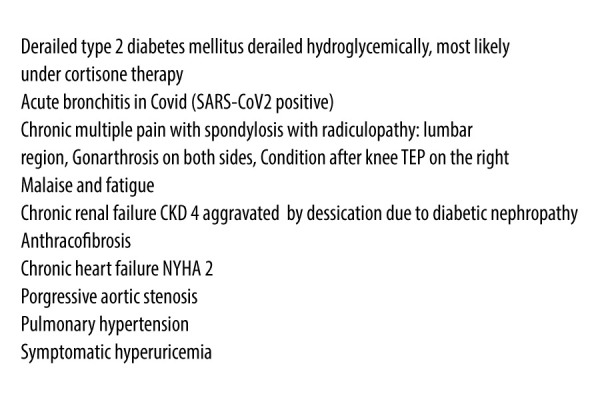
Confirmed diagnoses.
Because of the patient’s general condition and his self-reported medical history, a SARS-CoV-2 reverse transcription polymerase chain reaction test was administered, following World Health Organization protocols (WHO 13.03.20). The results were positive and the patient was admitted to the isolation ward. Because the patient was dehydrated, he was treated with infusions of Sterofundin and Cernevit. Both Sterofundin and Cernevit are injected intravenously. Sterofundin is a liquid containing electrolytes and Cernevit is used for parenteral nutrition. This treatment was followed by prompt mobilization, physiotherapy, and massage sessions with Vibrax to stimulate breathing and inhalation, as well as Tri-Flow therapy. With Vibrax therapy, a device generates vibrations in the chest that relax the muscles of the respiratory system, loosen mucus, improve breathing, and assist expectoration. Tri-Flow is a training device designed to strengthen the muscles responsible for breathing and the lungs, and to improve breathing capacity. These treatments were administered at close intervals during his inpatient hospitalization.
We stimulated the patient’s breathing by rubbing his back. We also administered oxygen therapy because his spontaneous oxygen saturation was reduced to 88% on admission. With time, the collective therapeutic interventions stabilized his respiratory function, reduced his cough, and eased his breathing. His dyspnea on light exertion regressed and the elevation in his inflammatory markers decreased over time.
The patient’s dominant clinical symptom was uncontrolled hyperglycemia with blood glucose levels of 550 mg/dL to 600 mg/dL. Specialists in internal medicine monitored the levels 7 to 10 times a day to optimize intensified conventional insulin therapy and they prescribed a diabetic diet for him. The patient’s pharmacological pain treatment also required optimization because he reported experiencing itchy hives and angioedema when he was at home. The cause of the symptoms was prior inadequate pain treatment.
Following an 8-day hospitalization and frequent application of the measures previously described, the patient was discharged to quarantine at home. To assess PROs related to his treatment, we used the depression module of the Patient Health Questionnaire (PHQ-9) to screen for the presence and severity of depression [10]. The questionnaire has 9 items and is based on the Diagnostic and Statistical Manual of Mental Disorders. This tool can be used for treatment and follow-up of patients and it is recommended by the American Psychiatric Association working group [11,12]. PHQ-9 has been used in patients with Middle East Respiratory Syndrome (MERS-CoV) [13], including individuals with MERS-CoV who were hospitalized in isolation wards [14]. It also has been used to assess psychological stress in healthcare workers who provide care to patients with COVID-19 [15]. We administered the PHQ-9 questionnaire to the patient on admission and discharge.
The patient’s functional restrictions were assessed with the Hannover Functional Ability Questionnaire (FFbH), which was applicable to this case because it has been used in patients with rheumatic diseases and other chronic joint diseases. The FFbH consists of 18 items and reflects functional restrictions in everyday activities. Function is reported as a percentage of the maximum number of points achieved. A score of 100% corresponds to unrestricted ability to perform everyday activities, whereas 0% indicates maximum limitation [16].
We also used the Nottingham Health Profile (NHP), which provides information about how a given disease affects a patient’s QoL [17,18]. The questionnaire consists of 38 statements on 6 dimensions of QoL: loss of energy, emotional reactions, physical mobility, sleep, social isolation, and pain. Individuals surveyed indicate whether these statements currently apply to them by answering “yes” or “no”. A weighting factor is allocated to each affirmative answer and the values are totalled. The higher the score, the stronger the subjective impairment in the specific area.
To check for pain, we used the Mainz Pain Staging System (MPSS), a diagnosis-independent classification model. It grades chronic pain according to 3 stages based on anamnestic data and information on the persistence of pain over time, dimensional spread of pain, use of medication, and utilization of healthcare facilities [19]. In addition, we used the graded classification of chronic pain severity according to von Korff, which describes pain intensity and activity limitations [20]. The questionnaire assesses pain severity and impairment in 3 areas of life: everyday life, recreational activities, and ability to work, including housework. Moreover, we decided to use a Visual Analogue Scale (VAS) because it can measure various outcomes [21,22]. In the present study, VAS was used to measure pain, mood (well-being), and physical condition.
To record impairment, the patient assesses the extent of subjectively experienced impairment in activities of daily living that is caused by pain. In the present study, this was done with the help of the Pain Disability Index (PDI). The PDI reflects a total of 7 separate items: family and home commitments, recreation, social activities, work, sex life, self-care, and essential activities [23].
The tables show detailed answers from the patient on admission to the hospital. Table 1 lists his answers to general questions.
Table 1.
General questions on admission.
| Have you taken anti-inflammatory drugs in the last 2 months before hospitalization? Please note that some painkillers also contain anti-inflammatory substances | Yes |
| Which food supplements (vitamin tablets etc.) have you taken in the last 2 months before hospitalization? | No |
| How good was your mental health on average in the 2 months before hospitalization? Please rate on a scale from 0 (very bad) to 10 (very good) | 8 |
| Have you done competitive sports in your life? If yes: a) from when to when? b) which sport? | Yes, athletics (12–25) |
| Have you ever had illnesses in your life that were caused by COVID-19 virus-like pathogens? | I don’t know |
| Which vaccinations do you have that not everyone has (e.g. vaccinations needed for certain trips, flu vaccinations,…)? | Flu vaccinations, measles vaccination, chickenpox vaccination |
To determine the degree of chronicity and level of pain that the patient experienced, we performed MPSS and graded his pain severity on admission according to von Korff (Table 2). The degree of chronicity at the time of admission corresponded to stage 3 (MPSS) (Table 3), the highest degree of chronicity. The von Korff pain grading yielded 6 impairment points (severe impairment, high-grade limitation), which is also the highest degree of severity.
Table 2.
Results of von Korff Pain Grading on admission.
| Question | Answer |
|---|---|
| Were you unable to perform your usual activities because of your pain? (last 3 months) | Yes, all the time |
| To what extent has pain in the last 3 months impaired your activities of everyday life (dressing, washing, eating, shopping)? | 6.5 |
| To what extent has pain in the last 3 months impaired free-time activities or activities with family or friends? | 8.8 |
| To what extent has pain in the last 3 months impaired your capacity to do work (including housework)? | 8.2 |
Table 3.
Results of Mainz Pain Staging System (MPSS) on admission.
| Question | Answer |
|---|---|
| How often has your (main) pain occurred in the last 4 weeks, in general (average)? | Persistent pain |
| How long has your (main) pain lasted in the past 4 weeks, in general? | Longer than a week, or permanent |
| Rate your pain in the past 4 weeks in general fluctuations in strength, i.e., has the pain changed between mild, moderate, and severe pain? | Constant pain intensity |
| How many pain pictures can you distinguish? | More than 2 pain pictures |
| In past 4 weeks, have you taken any medication for your pain? | More than 2 drugs |
| Have you ever attempted to stop taking or significantly reduce the dose of a medication that you take because of pain? | No |
| Have you changed your doctor because you pain treatment was unsuccessful? | No change |
| Have you ever been hospitalized because of your pain? | Only 1 time |
| Have you ever had surgery for your pain? | No |
| Have you had inpatient rehabilitation? | No |
The patient’s physical function improved from 8% on admission to 44% at time of discharge
When assessing QoL (Table 4), we could not evaluate the NHP items for pain and emotion due to insufficient information. We collected the necessary information required to assess the sensation of pain with the help of the VAS. All dimensions of the patient’s QoL improved during his hospital stay.
Table 4.
Results of Nottingham Health Profile (NHP) on admission.
| Yes | No | Don‘t know | |
|---|---|---|---|
| I am constantly tired | x | ||
| I have pain at night | x | ||
| I feel depressed | x | ||
| I have excruciating pain | x | ||
| I take pills to sleep | x | ||
| I forgot what it‘s like to feel joy | x | ||
| I feel irritated | x | ||
| I find it painful to change my body position | x | ||
| I feel lonely | x | ||
| I can only move around the house | x | ||
| It is difficult for me to bend down | x | ||
| Everything strains me | x | ||
| I wake up early in the morning | x | ||
| I can‘t go out at all | x | ||
| I find it difficult to make contact with other people | x | ||
| The days drag on | x | ||
| I have difficulty climbing stairs or going down stairs | x | ||
| It is difficult for me to stretch and to grab objects | x | ||
| I have pain when I walk | x | ||
| I have often lost my patience lately | x | ||
| I feel that I am not close to anyone | x | ||
| I lie awake most of the time | x | ||
| I feel like I‘m losing control | x | ||
| I am in pain when I stand | x | ||
| I find it difficult to get dressed myself | x | ||
| My energy fades quickly | x | ||
| It is difficult for me to stand for a long time (e.g., at the sink or the bus stop) | x | ||
| I am in constant pain | x | ||
| I take a long time to fall asleep | x | ||
| I feel like a burden to other people | x | ||
| Worries keep me awake at night | x | ||
| I feel that life is not worth living | x | ||
| I sleep badly at night | x | ||
| I find it difficult to get along with other people | x | ||
| I need help if I want to leave the house (e.g. a stick or someone to support me) | x | ||
| I am in pain when I climb stairs or go down the steps | x | ||
| I wake up depressed | x | ||
| I am in pain when I sit | x |
The patient’s 14-point PHQ-9 score suggests that he might have had a severe depressive disorder (moderate severity) on admission. However, during his hospital stay, his mental well-being score changed from 14 points to 10 points on the PHQ-9 scale.
The intensity of the patient’s pain decreased from a VAS of 6.0 on admission to 2.1 (Table 5) on the day of discharge. On discharge, the patient’s oxygen saturation was 95%, and his blood glucose levels were within normal range. He had no treatment complications.
Table 5.
Visual Analogue Scale (VAS) condition descriptions on admission.
| Question | Answer |
|---|---|
| Have you had pain in the past 4 weeks? | Yes |
| How would you rate your pain right now? | 6.0 |
| What was the most pain you have had in the past 4 weeks? | 7.0 |
| How severe has the pain been in the past 4 weeks on average? | 5.1 |
| Is your pain tolerable? | 4.6 |
| Indicate on the scale how much pain affects your sleep | 5.4 |
| Indicate on the scale how much pain affects how well you feel | 6.3 |
| Indicate on the scale how much pain affects your physical well-being | 6.9 |
Discussion
Elderly patients with multiple comorbid conditions that require treatment are often more susceptible to SARS-CoV-2 infection [24]. In this study, the patient’s main risk factor was DM with complications. DM is one of the leading causes of morbidity worldwide [25] and there is evidence that patients with the condition are more susceptible to infectious diseases [26]. If patients with SARS-CoV-2 require hospitalization, they face the added difficulty of isolation, which can affect their mental well-being, level of pain, QoL, or physical function. In patients with comorbidities who are infected with SARS-CoV-2, the course of treatment is also likely to be more unfavorable due to their high-risk profile [27], which means that they often require intensive care.
In addition, patients with MPSS stage III (the highest stage of chronicity) typically experience smaller changes in average pain intensity and more significant psychological impairment than do patients with stage MPSS stage I or II [28]. Complex interventions, which are called for in patients with comorbidities and/or multiple morbidities, do not always produce clinical results, just as PROs might not improve in each case [6]. The patient in our study had positive tendencies. Despite his highest chronicity grade and comorbidities, he believes that the acute care he received as an inpatient produced positive results. His mental well-being improved despite the isolation. In the context of patient-centered treatment, communication between nurses, medical staff, therapists, and a patient is accorded a high priority. This fact may explain, among other things, the positive effect on the patient’s mental well-being.
The immediate start of mobilization and physiotherapy, which were performed at close intervals in this case, is aimed at maintaining and supporting a patient’s ability to move independently. The immediate therapeutic application of mobilization also aims to prevent secondary diseases such as pneumonia, pressure ulcers, or joint contractures. Moreover, mobilization improves pulmonary perfusion and breathing and may reduce hospitalization time [29]. Movement therapy, which the patient in this case received during his entire inpatient stay, supports metabolic processes and blood circulation. It may also help maintain and improve joint mobility and coordination.
Thanks to the extensive use of PROs, the treatment team acquired a comprehensive picture of the patient’s state of health based on clinical data and the patient’s own assessment. PROs are used because clinical parameters alone often cannot provide information about a patient’s well-being in everyday life [30]. PROs should be collected immediately after a patient has been admitted to the hospital so that baseline data are available for use. PROs can influence communication flow between doctors, nurses, therapists, and patients, which can have a positive impact on treatment process and outcomes [31]. Obviously, a patient has to be able to assess his or her condition, which may limit the applicability of PROs.
Conclusions
By collecting PROs, a more comprehensive picture of a patient with COVID-19 can be developed. “The patient is given voice”, in addition to being assessed by others. The knowledge gained can be made available to the interdisciplinary treatment team to be incorporated into the treatment plan. If a patient has several comorbidities, all his or her diagnoses should be included in the treatment concept, in keeping with multidisciplinary treatment. Currently, this is not done automatically because clinical parameters dominate in acute in-patient care and they often push PROs into the background. Moreover, the importance of PROs is not yet acknowledged in the diagnosis-related groups (payment) system.
Acknowledgments
We thank the patient for participating in this study.
References:
- 1.Yang W, Cao Q, Qin L, et al. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19): A multi-center study in Wenzhou city, Zhejiang, China. J Infect. 2020;80(4):388–93. doi: 10.1016/j.jinf.2020.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sun P, Lu X, Xu C, et al. Understanding of COVID-19 based on current evidence. J Med Virol. 2020;92(6):548–51. doi: 10.1002/jmv.25722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020;323(18):1775–76. doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 4.Wang W, Tang J, Wei F. Updated understanding of the outbreak of 2019 novel coronavirus (2019-nCoV) in Wuhan, China. J Med Virol. 2020;92(4):441–47. doi: 10.1002/jmv.25689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wagner EH, Austin BT, Davis C, et al. Improving chronic illness care: Translating evidence into action. Health Affairs. 2001;20(6):64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- 6.Smith SM, Wallace E, O’Dowd T, Fortin M. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev. 2016;3(3):CD006560. doi: 10.1002/14651858.CD006560.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Romekye T, Noehammer E, Stummer H. Patient-report-outcome-measure and incentives for inpatient chronic care in Germany. Global J Health Sci. 2020;12(8):127–43. [Google Scholar]
- 8.Liu K, Chen Y, Wu D, et al. Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID-19. Complement Ther Clin Pract. 2020;39:101132. doi: 10.1016/j.ctcp.2020.101132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Snyder CF, Aaronson NK, Choucair AK, et al. Implementing patient-reported outcomes assessment in clinical practice: A review of the options and considerations. Qual Life Res. 2012;21:1305–14. doi: 10.1007/s11136-011-0054-x. [DOI] [PubMed] [Google Scholar]
- 10.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.U.S. Preventive Services Task Force Screening for depression: Recommendations and rationale. Ann Intern Med. 2002;136(10):760–64. doi: 10.7326/0003-4819-136-10-200205210-00012. [DOI] [PubMed] [Google Scholar]
- 12.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) Washington DC: American Psychiatric Association; 2000. [Google Scholar]
- 13.Lee SH, Shin HS, Park HY, et al. Depression as a mediator of chronic fatigue and post-traumatic stress symptoms in middle east respiratory syndrome survivors. Psychiatry Investig. 2019;16(1):59–64. doi: 10.30773/pi.2018.10.22.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim H, Yoo HC, Lee SY, et al. Psychiatric findings in suspected and confirmed middle east respiratory syndrome patients quarantined in hospital: A retrospective chart analysis. Psychiatry Investig. 2018;15(4):355–60. doi: 10.30773/pi.2017.10.25.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kohlmann T, Raspe HH. Der Funktionsfragebogen Hannover zur alltagsnahen Diagnostik der Funktionsbeeinträchtigungen durch Rückenschmerzen (FFbH-R) Rehabilitation. 1996;35(1996):I–VIII. [in German] [PubMed] [Google Scholar]
- 17.Hunt SM, McKenna SP, McEwen J, et al. The Nottingham Health Profile: Sbjective health status and medical consultations. Soc Sci Med. Part A. 1981;15:221–29. doi: 10.1016/0271-7123(81)90005-5. [DOI] [PubMed] [Google Scholar]
- 18.Kohlmann T, Bullinger M, Kirchberger-Blumstein I. Die deutsche Version des Nottingham health profile (NHP): Übersetzungsmethodik und psychometrische Validierung. Soz Praventivmed. 1997;42(3):175–85. doi: 10.1007/BF01300568. [in German] [DOI] [PubMed] [Google Scholar]
- 19.Gerbershagen HU. Das Mainzer Stadienkonzept des Schmerzes: Eine Standortbestimmung. In: Klingler D, Morawetz R, Thoden U, et al., editors. Antidepressiva als Analgetika. Aktueller Wissensstand und Therapeutische Praxis. Wien: Aarachne; 1996. pp. 71–95. [in German] [Google Scholar]
- 20.von Korff M, Ormel J, Keefe FJ, Dworkin SF. Grading the severity of chronic pain. Pain. 1992;50(2):133–49. doi: 10.1016/0304-3959(92)90154-4. [DOI] [PubMed] [Google Scholar]
- 21.Lee KA, Kieckhefer GM. Measuring human responses using visual analogue scales. Western J Nurs Res. 1989;1(1):128–32. doi: 10.1177/019394598901100111. [DOI] [PubMed] [Google Scholar]
- 22.Pfennings L, Cohen L, van der Ploeg H. Preconditions for sensitivity in measuring change: Visual analogue scales compared to rating scales in a Likert format. Psychol Rep. 1995;77(2):475–80. doi: 10.2466/pr0.1995.77.2.475. [DOI] [PubMed] [Google Scholar]
- 23.Dillmann U, Nilges P, Saile H, et al. Behinderungseinschätzung bei chronischen Schmerzpatienten. Schmerz. 1994;8(2):100–10. doi: 10.1007/BF02530415. [DOI] [PubMed] [Google Scholar]
- 24.Zhang JJ, Dong X, Cao YY, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020;75(7):1730–41. doi: 10.1111/all.14238. [DOI] [PubMed] [Google Scholar]
- 25.Knapp S. Diabetes and infection: Is there a link? – A mini-review. Gerontology. 2013;59(2):99–104. doi: 10.1159/000345107. [DOI] [PubMed] [Google Scholar]
- 26.Joshi N, Caputo GM, Weitekamp M. Infections in patients with diabetes mellitus. N Engl J Med. 1999;341(25):1906–12. doi: 10.1056/NEJM199912163412507. [DOI] [PubMed] [Google Scholar]
- 27.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus – infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–69. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Frettlöh J, Maier C, Gockel H, Hüppe M. Validität des Mainzer Stadienmodells der Schmerzchronifizierung bei unterschiedlichen Schmerzdiagnosen. Der Schmerz. 2003;17(4):240–51. doi: 10.1007/s00482-003-0227-9. [in German] [DOI] [PubMed] [Google Scholar]
- 29.Mundy LM, Leet TL, Darst K, et al. Early mobilization of patients hospitalized with community-acquired pneumonia. Chest. 2003;124:883–89. doi: 10.1378/chest.124.3.883. [DOI] [PubMed] [Google Scholar]
- 30.Hostettler S, Kraft E, Bosshard C. Patient-reported outcome measures: Die Patientensicht zählt. Schweiz Ärzteztg. 2018;99(40):1348–52. [in German] [Google Scholar]
- 31.Nelson EC, Eftimovska E, Lind C, et al. Patient reported outcome measures in practice. BMJ. 2015;350:g7818. doi: 10.1136/bmj.g7818. [DOI] [PubMed] [Google Scholar]


