FIGURE 1.
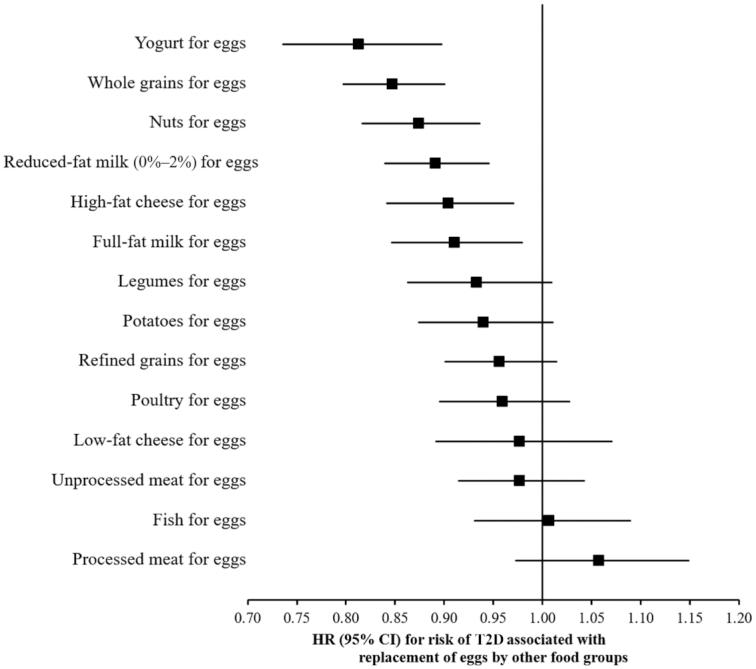
Statistical model–based HRs and 95% CIs for incident T2D associated with replacing 1 egg/d with 1 serving/d of other foods in the NHS, the NHS II, and the HPFS (pooled analysis, n = 213,798). In the substitution analyses, Cox proportional hazards regression models were stratified by calendar time (in 2-y intervals) and cohort, and adjusted for age (mo), race (Caucasian/other), family history of diabetes (yes/no), baseline history of hypercholesterolemia (yes/no), baseline history of hypertension (yes/no), smoking status (never, former, current), BMI (in kg/m2: <21.0, 21.0–22.9, 23.0–24.9, 25.0–26.9, 27.0–29.9, 30.0–34.9, ≥35.0), physical activity (MET-h/wk: <3.0, 3.0–8.9, 9.0–17.9, 18.0–26.9, ≥27.0), oral contraceptive use (never, former, current; in the NHS II only), postmenopausal hormone use (premenopausal, never, former, current; in the NHS and NHS II only), statin use (yes/no), cumulative average alcohol intake (g/d; quintiles), multivitamin use (yes/no), and physical examination during the 2-y cycle (yes/no). The model also included updated cumulative average of daily intake of total calories (kcal/d; in quintiles), bacon (servings/d; in categories), unprocessed red meat (servings/d; in categories), other processed red meats (servings/d; in categories), refined grains (servings/d; in categories), fruits (servings/d; in categories), vegetables (servings/d; in categories), potatoes (servings/d; in categories), full-fat milk (servings/d; in categories), coffee (servings/d; in categories), fruit juices (servings/d; in categories), and sugar-sweetened beverages (servings/d; in categories). All covariates (except race, family history of diabetes, baseline hypercholesterolemia, and basline hypertension) were updated every 2 y. HPFS, Health Professionals’ Follow-up Study; NHS, Nurses’ Health Study; T2D, type 2 diabetes.
