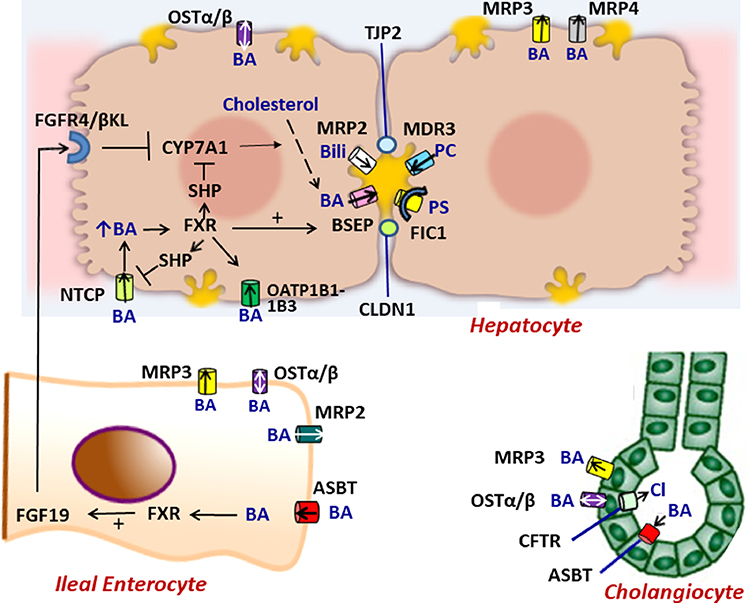
Figure 1.
Molecular regulation of the enterohepatic circulation of bile acids.In hepatocytes, bile acids are taken up by NTCP, OSTα/β or OATP1B1–1B3 on the basolateral membrane or are synthesized from cholesterol by CYP7A1. The ATP-dependent BSEP transports bile acids into bile across the canalicular membrane. FXR, a nuclear hormone receptor, is a master switch that upregulates mRNA expression of BSEP and downregulates NTCP and CYP7A1 (through SHP). MRP2 (conjugated bilirubin transporter), MDR3 (phospholipid transporter) and FIC1 (phosphotidylserine flippase) participate in bile formation across the canalicular membrane. MRP3 and MRP4 transport bile acids from the hepatocyte to the sinusoids. Tight junction proteins (TJP2 and CLDN1) maintain the boundary between canalicular bile and the hepatocyte, preventing the toxicitiy of secreted bile acids. In ileal enterocytes, ASBT promotes absorption of luminal bile acids across the enterocyte brush border which are transported by OSTα/β or MRP3 into portal blood to return to the liver where they interact with FXR to suppress further bile acid synthesis. Within the enterocyte, absorbed bile acids may also activate FXR which upregulates synthesis and secretion of FGF19 into the portal circulation. When it reaches the liver FGF19 binds to the FGFR4/ βKL receptor on the hepatocyte basolateral membrane and triggers suppression of CYP7A1. In cholangiocytes, ASBT in the apical membrane may transport bile acids from bile back into the cell and subsequently into the portal circulation by OSTα/β or MRP3 in the basolateral membrane. CTFR actively secretes chloride into bile. Perturbations of bile formation can result from genetic variants in many of these proteins (FIC1, BSEP, MDR3, MRP2, CFTR, TJP2, CLDN1) and from adaptive changes in transporter expression and function in response to inflammatory, obstructive, or drug-induced insults. . BA = bile acid, PC = phosphatidylcholine, Bili = conjugated bilirubin, Cl = chloride, PS= phosphatidylserine.