Abstract
Although high-protein diets continue to be popular for weight loss and type 2 diabetes, evidence suggests that worsening renal function may occur in individuals with—and perhaps without—impaired kidney function. High dietary protein intake can cause intraglomerular hypertension, which may result in kidney hyperfiltration, glomerular injury, and proteinuria. It is possible that long-term high protein intake may lead to de novo CKD. The quality of dietary protein may also play a role in kidney health. Compared with protein from plant sources, animal protein has been associated with an increased risk of ESKD in several observational studies, including the Singapore Chinese Health Study. Potential mediators of kidney damage from animal protein include dietary acid load, phosphate content, gut microbiome dysbiosis, and resultant inflammation. In light of such findings, adopting current dietary approaches that include a high proportion of protein for weight reduction or glycemic control should be considered with care in those at high risk for kidney disease. Given the possibility of residual confounding within some observational studies and the conflicting evidence from previous trials, long-term studies including those with large sample sizes are warranted to better ascertain the effects of high protein intake on kidney health.
Keywords: nutrition, chronic kidney disease, high protein diet, glomerular hyperfiltration, proteinuria
In the United States, >60% of the population meets the criteria for being obese or overweight. In this context, growing interest in low-carbohydrate, high-protein diets has emerged over recent decades. The revived popularity of low-carbohydrate, high-protein diets may be partly fueled by their promotion across social media as an effective means for rapid weight loss and better glycemic control. For patients with CKD or at risk of CKD, high intake of dietary protein, including animal protein, may have detrimental effects on kidney function and long-term kidney health. This review focuses on the potential consequences of high dietary protein intake on kidney health and its relevance in the primary and secondary prevention of CKD.
The Rise in Popularity of High-Protein Diets
The estimated average requirement for protein intake is 0.6 g of protein per kilogram of ideal body weight per day, which corresponds to the amount of protein required to avoid negative nitrogen balance and to meet half of a population’s requirements. The recommended daily allowance for protein intake is 0.83 g/kg per day and is calculated to meet the requirements of 97%–98% of the population (two SD above the estimated average requirement).1 Although there is a lack of consensus regarding the formal definition of a high-protein diet, most definitions set a threshold between 1.2 and 2.0 g/kg per day. Within this range, protein consumption >1.5 g/kg per day is generally considered to be a high-protein diet. Data from the National Health and Nutrition Examination Survey (NHANES) show that the current average consumption of protein in the United States is estimated to be approximately 1.2–1.4 g/kg per day,2 which is higher than the recommended amount. Popular weight-loss diets encourage higher amounts of protein while restricting the amount of carbohydrates, based on the assumption that all carbohydrates are undesirable—an assumption that has been refuted in the literature.3 Although such diets vary, these weight-loss strategies typically recommend that 25%–35% of calories consumed should be from protein and <45% of calories should be from carbohydrates (Supplemental Table 1). In extreme cases, such as the ketogenic diet, <5%–10% of calories are from carbohydrates.
Hyperfiltration from High-Protein Diets and Effects on Kidney Health
In 1928, it was first noted in a frog model that amino acids and peptides could increase blood flow to the kidneys.4 Subsequent studies in rats and dogs had similar findings.5–7 In one study of dogs eating meat, the increase in the GFR (a marker of hyperfiltration) was dose dependent, with a maximal GFR increase of nearly 80%.8
Human data have also shown hyperfiltration with high protein consumption.7 The largest short-term (<6 months) trial showed that a high-protein diet (protein comprising 25% of calories) increased eGFR by 3.8 ml/min per 1.73 m2 after 6 weeks compared with a lower protein diet (protein comprising 15% of calories).9,10 In the early stages, glomerular hyperfiltration occurs as a rise in GFR, in proteinuria, or both, but may result in a loss of kidney function over time, particularly in those with underlying CKD, risk factors for CKD, or both.11
Several long-term observational studies in humans have shown an association between the consumption of high-protein diets and kidney function decline in individuals with preexisting CKD, including the Nurses’ Health Study and the Gubbio Population Study.10,12 In the Nurses’ Health Study, an 11-year observational study of women experiencing mild renal insufficiency (defined as eGFR >55 ml/min per 1.73 m2 and <80 ml/min per 1.73 m2), every 10-g increase in protein intake was significantly associated with a change in eGFR of −1.69 ml/min per 1.73 m2 (95% confidence interval [95% CI], −2.93 to −0.45 ml/min per 1.73 m2), which was not observed in the population with normal renal function.12
In the Gubbio study, a population-based study of 1522 participants aged 45–64 years, a higher protein intake was associated with a lower eGFR after 12 years, including among participants with or without CKD (with CKD defined as an eGFR <90 ml/min per 1.73 m2). Overall, in a multivariable regression analysis, 1 g/d higher protein intake was related to a −4.1 (95% CI, −5.1 to −3.1) ml/min per 1.73 m2 more negative eGFR change and to a significantly increased risk for incident eGFR <60 ml/min per 1.73 m2 (odds ratio, 1.78; 95% CI, 1.15 to 2.78).10
Additional long-term observational studies have also described the association of high protein intake with a decline in kidney function, whereas others have not (Table 1). Most recently, a study of nearly 1800 Iranians followed for an average of 6 years showed that those consuming excess protein in the form of a low-carbohydrate, high-protein diet also had a higher risk of CKD (odds ratio, 1.48; 95% CI, 1.03 to −2.15).13
Table 1.
Summary of observational studies of high dietary protein intake and kidney health across large populations (>1000 participants)
| Study Reference | Study or Location | Type | N (BMI, kg/m2) | Mean Age (yr) | Mean eGFR (ml/min per 1.73 m2) | DM/HTN HTx (%) | Sex (% male) | Protein Intake in the Highest Group (g/kg per d, g/d, or % of total calorie intake) | Duration (yr) | Variable and Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| Knight et al.12 | Nurses’ Health Study | Prospective cohort | 1624 (N/D) | 55 | 90 | 4/40 | 0 | 93 g/d | 11 | HP was not associated with eGFR decline in normal renal function. However, it was associated with accelerated eGFR decline in mild CKD |
| Huang et al.74 | Taiwan | Cross-sectional | 599 (24.3) | 60 | 22 | N/D | 54 | N/D | N/A | HP was also associated with worsening eGFR at increments of −3.50 ml/min per 1.73 m2, compared with moderate and low protein intake (P<0.001) |
| Halbesma et al.75 | Prevention of Renal and Vascular ENd-stage Disease (PREVEND) | Prospective cohort | 8461 (26.1) | 50 | 81 | N/D | N/D | 1.4 g/kg per d | 7.0 | No association between baseline protein intake and rate of renal function decline |
| Cirillo et al. 10 | Gubbio Study | Prospective cohort | 1522 (28) | 54 | 84 | 5/41 | 44 | 2.1 g/kg per d | 12 | 1 g/d higher protein intake was related to −4.1 ml/min per 1.73 m2 more negative eGFR change and 1.78 risk for incidence of eGFR <60 ml/min per 1.73 m2 |
| Beasley et al.76 | Cardiovascular Health Study | Prospective cohort | 3623 (26.5) | 72 | 73 | 14/55 | 39 | 1.63 g/kg per d;24% of total calories | 6.4 | Protein intake was not associated with change in eGFR (P>0.05 for all comparisons) |
| Lew et al.51 | Singapore Chinese Health Study | Prospective cohort | 63,257 (23) | 57 | N/D | 9/23 | 43 | 65.3 g/d | 15.5 | Total protein intake was positively associated with incidence of ESKD in a model that adjusted for basic demographic characteristics (i.e., age, gender, dialect, educational level, and year of interview: HR, 1.55; 95% CI, 1.28 to 1.87) when comparing the highest quartile with the lowest quartile intake. However, the HR was attenuated to 1.19 (95% CI, 0.98 to 1.44) after adjusting for other lifestyle and comorbidity factors |
| Haring et al.50 | Atherosclerosis Risk in Communities (ARIC) Study | Prospective cohort | 11,952 (27) | 54 | 103 | 11/31 | 56 | 109.5 g/d;19.5% | 23 | Total protein consumption itself was not associated with increasing risk of incident CKD (HR of the highest quintile, 0.89; 95% CI, 0.76 to 1.05) |
| Malhotra et al.77 | Jackson Heart Study | Observational cohort | 3165 (31.8) | 55 | 97 | 19/57 | 36 | 1.0 g/kg per d;19.4% | 8 | Consumption of protein as percentage of energy intake in lowest and highest quintiles was associated with decline in eGFR among subjects who were diabetic |
| Esmeijer et al.78 | Alpha Omega Cohort | Prospective cohort | 2255 (27.6) | 69 | 82 | 18/57 | 80 | 92 g/d17% | 3.5 | Patients with a daily total protein intake of ≥1.20 compared with <0.80 g/kg ideal body weight had a twofold faster annual eGFR cysC decline (−1.60 versus −0.84 ml/min per 1.73 m2) in patients post-MI |
| Jhee et al.79 | Korean Genome and Epidemiology Study | Prospective cohort | 9226 (24.5) | 52 | 94 | 7/14 | 48 | 1.7 g/kg per d | 11.5 | The highest quartile was associated with 1.32-fold increased risk of rapid eGFR decline (95% CI, 1.02 to 1.73) |
| Farhadnejad et al.13 | Tehran Lipid and Glucose Study | Prospective cohort | 1797 (26.7) | 38 | 76 | 12/18 | 46 | 16% | 6.1 | The highest tertile of LCHP diet had greater risk of incident CKD (OR, 1.48; 95% CI, 1.03 to 2.15) in comparison to those in the lowest one (P for trend=0.027) |
BMI, body mass index; DM, diabetes mellitus; HTN, hypertension; HTx, heart transplant; N/D, not described; HP, high-protein diet; N/A, not applicable; HR, hazard ratio; cysC, cystatin C; MI, myocardial infarction; LCHP, low-carbohydrate, high-protein diet; OR, odds ratio.
However, some observational studies have not observed an association between a high-protein diet and kidney function. Also, randomized clinical trials with a relatively long observation period (>6 months) have generally demonstrated little to no effect on renal function, which may be limited by the use of creatinine-based measurements of kidney function, a sizable attrition in study participants, and the limited duration of these studies (a maximum of 24 months) (Table 2). In one meta-analysis of 30 trials that included short- and long-term trials, a high-protein diet did cause hyperfiltration (as measured by a change in GFR) but caused no change in plasma creatinine.14 Another meta-analysis of low-carbohydrate diets showed a small increase in eGFR (0.13 ml/min per 1.73 m2; 95% CI, 0.00 to 0.26 ml/min per 1.73 m2).15
Table 2.
Summary of long-term (>6 mo) randomized controlled trials of high dietary protein intake and kidney health
| Study Reference | Location | Population Characteristics | Size (LP/HP) | Duration | Protein Intake | Outcome (HP versus LP) |
|---|---|---|---|---|---|---|
| Flechtner-Mors et al.80 | Germany | Obese | 110 (55/55) | 12 mo | HP, 1.34 g/kg;LP, 0.8 g/kg | Dietary protein was not associated with change of renal function (BUN and creatinine) |
| Li et al.27 | United States | Obese | 85 (41/44) | 12 mo | HP, 2.2 g/kg;SP, 1.1 g/kg | CC changes were NS, but hyperfiltration was shown in HP. Albuminuria was not different |
| Yancy et al.81 | United States | Obese | 146 (74/72) | 48 wk | HP, 112.2±46.8 g/d;LP, 78.0±35.5 g/d | Creatinine and albuminuria were not different between groups |
| Larsen et al.26 | Australia | Type 2 DM, obese | 99 (46/53) | 12 mo | HP, 30%LP, 15% | eGFR and albuminuria were not different between groups, although protein intake measured by urea nitrogen was not significantly different between groups |
| Wycherley et al.82 | Australia | Obese | 68 (35/33) | 12 mo | HP, 35%, 1.2 g/kg;LP, 17%, 0.8 g/kg | CC changes were NS, but hyperfiltration was shown in HP |
| Krebs et al.25 | New Zealand | Type 2 DM, obese | 294 (150/144) | 24 mo | HP, 30%;LP, 15% | Creatinine and albuminuria was not changed, but protein intake was not regulated well, and it was not different between groups |
| Friedman et al.16 | United States | Obese | 307 (154/153) | 24 mo | HP, >15%;LP, 15% | CC was higher in HP group at 12 mo (P<0.05), and the change was attenuated at 24 mo. Albumin excretion was not different between groups |
| Tirosh et al.83 | Israel | Obese | 318 | 24 mo | HP/LC, unlimited protein intake–finally 22%;NP/LP, 18.8%–19.1% | Dietary protein was not associated with increase of eGFR and albuminuria after adjustment. But protein intake of two groups was not different |
| Tay et al.24 | Australia | Type 2 DM, obese | 115 (57/58) | 12 mo | HP, 28%;LP, 17% | eGFR and albuminuria were not different |
| Møller et al.17 | Europe and New Zealand | Prediabetes | 309 (206/103) | 12 mo | HP, 25%;NP/LP, 15% | There were no associations between increased protein intake and creatinine clearance |
LP, low protein intake; HP, high protein intake; CC, creatinine clearance; DM, diabetes mellitus.
The negligible effects seen in long-term studies also may be attributed to the counterbalancing effects of hyperfiltration (an increase in renal function) and kidney damage from hyperfiltration (a decrease in renal function). For example, a randomized clinical trial of participants who were prescribed the Atkins diet (protein content around 30% of total energy intake) versus a control diet (protein content around 15% of total energy intake) for 12 months reported a rise in creatinine clearance among participants in the Atkins diet arm, suggesting hyperfiltration.16 However, the differences in creatinine clearance between the Atkins versus control diet groups were attenuated after 24 months of observation,16 which may indicate that the short-term rise in GFR with high protein intake may be followed by a decline in GFR over time, possibly as a result of renal injury.
Hyperfiltration may also lead to an increased risk of proteinuria. Several studies have shown a link between high protein intake and increased albuminuria or proteinuria as an early indicator of kidney damage. Several observational studies have also demonstrated an increased risk of albuminuria with high dietary protein intake versus standard dietary protein intake, even after accounting for differences in sociodemographics, comorbidities, body anthropometry, health behaviors (e.g., physical activity, energy intake, and smoking status), and medication use.17–20 However, in another study, the researchers did not consistently observe an association of high protein consumption with albuminuria for the whole population, finding it only among individuals with hypertension and diabetes.21 In short-term trials with 4–12 weeks of follow-up, in patients with a single kidney or type 2 diabetes, those assigned to high-protein diet interventions (defined as 1.6 g/kg per day or 30% of energy content derived from protein) resulted in a slight increase in urinary albumin excretion compared with participants assigned to a standard diet.22,23
However, several long-term (>6 months) trials have not observed an increase in proteinuria with high protein intake,16,24–27 particularly among participants with normal kidney function. In one trial, the albumin excretion rate did not change between baseline and 12 months, regardless of whether participants were assigned to a high-protein diet (protein comprising 28% of total energy content) or a high-carbohydrate diet (protein comprising 17% of total energy content).24 Some of these studies were carried out with a small number of participants (<100) and over a relatively short duration of observation (<12 months),26,27 and the effect of a high-protein diet on proteinuria merits further examination in large-scale, long-term trials. Randomized clinical trials for hyperfiltration of kidney and albuminuria are summarized in Table 2.
Proposed Pathways Linking High-Protein Diets and CKD
Mechanistically, high protein intake may lead to increases in kidney volume and weight in humans,28 which was demonstrated in a mouse model as mesangial matrix expansion with tubulointerstitial fibrosis.29 Although research has not fully elucidated the exact mechanisms of protein-induced glomerular hyperfiltration, it is thought to occur as an evolutionary feedback mechanism facilitating the excretion of increased amounts of protein-derived nitrogenous waste. Other factors proposed as underlying mechanisms to facilitate the increased excretion of nitrogenous waste include changes in endocrine mediators (e.g., glucagon and IGF-1), leading to vasodilation, and changes in neurohormonal responses (i.e., tubuloglomerular feedback) within the kidney.30
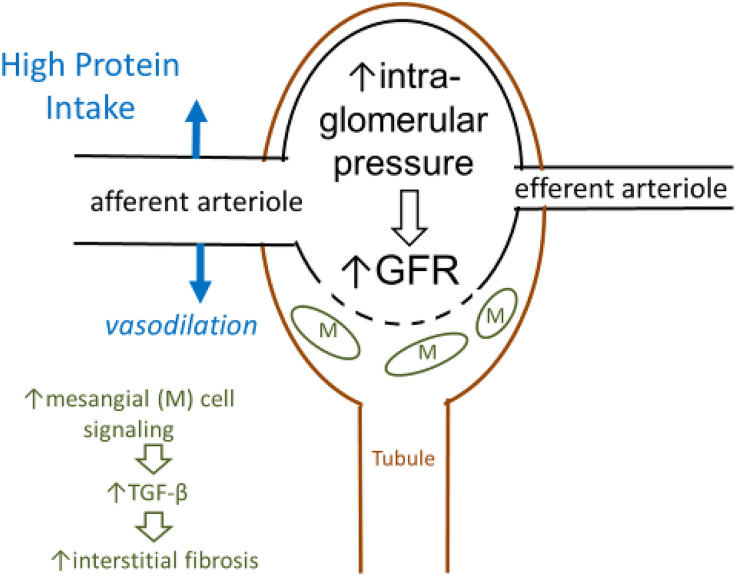
Although some instances of short-term glomerular hyperfiltration, such as that which occurs during pregnancy, may not be associated with a decrease in kidney function, it is possible that prolonged, recurrent glomerular hyperfiltration induced by consumption of a high-protein diet may lead to kidney damage through multiple pathways over time (Figure 1).31 Experimental data demonstrated that, in a rat model, incrementally higher levels of protein intake (i.e., 20%, 30%, and 45% of total energy content) caused an increase in proinflammatory gene expression in a dose-dependent manner,32 and that, in pig models, long-term exposure to a high-protein diet (i.e., 35% of energy intake) led to 55% greater renal fibrosis and 30% greater glomerulosclerosis.33
Figure 1.
High dietary protein intake leads to the dilation of the afferent arteriole and increased GFR, which may lead to damage to kidney structures over time due to glomerular hyperfiltration.
Harmful Metabolic Consequences of High-Protein Diets
In addition to having potential implications of kidney function and structure, high-protein diets may also lead to other metabolic complications.
High dietary intake of protein may lead to higher levels of urea and other nitrogenous waste products. Indeed, several studies have shown that high versus standard dietary protein intake is associated with higher BUN concentrations.16,34 For example, in a crossover study of 24 healthy young men who consumed a diet with a high level of protein (2.4 g/kg per day) or a diet with a normal level of protein (1.2 g/kg per day) over a 7-day period for each diet (total 14 days), BUN concentrations were significantly higher during the period of higher protein intake than during the period of normal protein intake.34 Conversely, other studies have shown a proportional reduction in urea generation with dietary protein restriction.35 One theory holds that high circulating BUN levels, by enhancing protein carbamylation and generating reactive oxygen species, lead to increased oxidative stress, inflammation, endothelial dysfunction, and cardiovascular disease.30
A diet with high protein intake might also lead to metabolic acidosis among patients with advanced CKD who have impaired acid excretion and generation of bicarbonate, particularly in the context of protein sourced from animal-based foods. Furthermore, dietary acid might also be a risk factor for CKD through intrarenal mechanisms promoting kidney injury and progressive GFR decline.36 In an animal model of CKD, chronic metabolic acidosis can stimulate the production of angiotensin II, aldosterone, and endothelin-1, as well as ammoniagenesis, all of which can promote inflammation and fibrosis.36 The standard American diet, in which protein comprises approximately 15% of energy, is estimated to produce a dietary acid load of approximately 1 mEq/kg per day, the bulk of which is derived from animal sources such as meats, eggs, and cheeses.37
In contrast, by including a higher proportion of foods with natural alkali, such as fruits and vegetables, a vegan diet is nearly acid neutral. Plant-based foods can be used to reduce both the dietary acid load and the severity of metabolic acidosis.38 Similarly, a low protein intake in patients with advanced nondialysis CKD has also been shown to attenuate the severity of metabolic acidosis. NHANES III data have shown that, among 1486 adult participants with CKD, higher dietary acid load ascertained by 24-hour dietary recall was strongly associated with development of ESKD over a median follow-up of 14.2 years.39 Compared with participants whose dietary acid consumption was in the lowest tertile, those with dietary acid consumption in the highest tertile had triple the risk of incident ESKD, even after accounting for differences in sociodemographics, nutritional factors, clinical factors, baseline eGFR, proteinuria, and serum bicarbonate levels.39
Dietary protein intake, which is also strongly correlated with phosphorus intake,40 may account for 84% of the variance in dietary phosphorus intake.41 Hyperphosphatemia is a critical factor for morbidity or mortality in patients with CKD.42 Several large epidemiologic studies have found higher phosphorus levels (even those within the normal range) to be associated with an increased risk of cardiovascular disease morbidity and mortality, even in individuals with normal kidney function.43,44 Dietary phosphate loading increases expression of fibroblast growth factor 23 (FGF-23), which is a phosphaturic hormone.45 Elevated FGF-23 levels are associated with vascular calcifications among patients with CKD46 and left ventricular hypertrophy in experimental animals with uremia.47 In a long-term observational study over 10 years among an elderly community population, FGF-23 independently associated with all-cause mortality and incidence of heart failure.48 In addition, in the Ramipril Efficacy In Nephropathy trial, participants with higher serum phosphate levels had faster progression of kidney disease compared with those who had lower levels.49
Protein Source (Plant versus Animal Protein)
Several observational studies have noted the source of dietary protein intake in relation to CKD incidence (Table 3), finding a strong association between intake of animal protein, especially processed red meat consumption, and incidence and progression of CKD. The Atherosclerosis Risk in Communities Study showed an increased risk of incident CKD among participants consuming the highest quintile of red/processed meat compared with those consuming the least.50 Similarly, in the Singapore Chinese Health Study, consuming red meat strongly associated with ESKD risk in a dose-dependent manner.51 Data from these studies also demonstrated that red meat, processed meat, or both associated with an increased risk of albuminuria, rapid eGFR decline, or both.19,51 Substituting one serving of red meat with a plant-based protein such as legumes was associated with a 31%–62.4% reduced risk of CKD.50,51
Table 3.
Summary of observational studies of protein source (plant versus animal) and kidney health
| Study Reference | Study or Location | Type | Size | Age (yr) | Follow-up Period (yr) | Variable and Outcome |
|---|---|---|---|---|---|---|
| Knight et al.12 | Nurses’ Health Study | Prospective cohort study | 1624 | 42–68 | 11 | Consumption of nondairy protein was associated with rapid decline of eGFR among participants with mild CKD |
| Lin et al.19 | Nurses’ Health Study | Prospective cohort study | 3121 | 67 | 11 | HP usually found in Western dietary pattern (red and processed meat, saturated fat, sweets) was associated with albuminuria (OR, 2.17; 95% CI, 1.18 to 3.66) and rapid eGFR decline (OR, 1.77; 95% CI, 1.03 to 3.03). On the other hand, DASH diet (fruits, vegetables, whole grains) had a lower risk of rapid eGFR decline (OR, 0.55; 95% CI, 0.38 to 0.80) |
| Lin et al.20 | Nurses’ Health Study | Prospective cohort study | 3348 | 67 | 11 | Highest quartile of animal fat was associated with higher odds of microalbuminuria (OR, 1.72; 95% CI, 1.12 to 2.64). Consuming two or more servings of red meat/wk was associated with higher odds of microalbuminuria (OR, 1.51; 95% CI, 1.01 to 2.26) |
| Beasley et al.76 | Cardiovascular Health Study | Prospective cohort study | 3623 | >65 | 6.4 | There were also no significant associations when protein intake was separated by source (animal versus vegetable) |
| Lew et al.51 | Singapore Chinese Health Study | Prospective cohort study | 63,257 | 45–74 | 15.5 | Highest quartile of protein intake (from red meat) had 40% increased HR of ESKD (dose dependent). Replacing one serving of red meat with other protein sources was associated with a max relative risk reduction of 62.4% |
| Haring et al.50 | Atherosclerosis Risk in Communities (ARIC) Study | Prospective cohort study | 11,952 | 44–66 | 23 | Highest quintile of red/processed meat intake had 23% increased HR of incident CKD. On the other hand, highest quintile of vegetable protein intake had 24% reduced HR of incident CKD |
| Oosterwijk et al.84 | DIAbetes and LifEstyle Cohort Twente-1 Study (DIALECT-1) | Cross-sectional | 420 | 63±9 | N/A | The prevalence ratio for the incidence of CKD (<60ml/min per 1.73 m2) in the fully adjusted model was 0.47 (95% CI, 0.23 to 0.98; P=0.04) in the highest tertile of vegetable protein intake |
HP, high-protein diet; OR, odds ratio; DASH, Dietary Attempt to Stop Hypertension; HR, hazard ratio; N/A, not applicable.
The pathophysiology of the association of animal protein with CKD remains unclear. One proposed mechanism is the link between animal protein consumption and hypertension, which observational studies and controlled trials have repeatedly demonstrated.52 Conversely, plant-based foods have been shown to have the opposite effect,53,54 so much so that emphasizing plant-based foods over animal-based foods is one of the principles of the Dietary Attempt to Stop Hypertension (DASH) diet.55 Animal protein consumption also may lead to weight gain, which might be another predisposing factor for kidney disease. Additionally, studies have demonstrated that, compared with intake of plant protein, intake of animal protein causes an imbalance in the composition of the gut microbiome by producing more ammonia and sulfur-based materials and having a proinflammatory profile, which may result in reduced kidney function and an increased risk of cardiovascular disease.56–59 Finally, high red meat intake has been associated with an increase in inflammation and oxidative stress, including upregulated inflammatory mediators such as NF-κB and inflammatory cytokines.60,61
These differences between the effects of animal-based protein versus plant-based protein may favor the use of the latter in both CKD and ESKD. Plant-based proteins have been previously described as being more than adequate for nutrition in these populations.62
The Newest High-Protein Diet: the Ketogenic Diet
Although the ketogenic diet has recently received a disproportionate amount of attention because it is purported to help treat obesity and type 2 diabetes, evidence that it actually offers such benefits is limited. Long-term randomized trials have failed to show a clinically significant benefit over comparator diets.3 Worse, the diet is not without consequence: it may produce adverse effects in the average dieter, such as hyperlipidemia,3 vitamin and mineral deficiencies, and fatigue. For patients with or at high risk for kidney disease, the ketogenic diet may further tilt the risk/benefit ratio unfavorably by producing kidney-specific risks.
In brief, the ketogenic diet restricts the intake of carbohydrates as an energy source and instead emphasizes the use of (both ingested and stored) fat, resulting in the production of ketones (and giving the diet its name). The diet emphasizes an intake of 1.2–2.0 g/kg of protein per day, which is within the range of a diet with moderately high to high levels of protein.63 For patients with existing kidney disease, the diet’s high protein intake may accelerate the progression of their kidney disease.64 For individuals without kidney disease, there is limited evidence suggesting that these diets pose danger. However, data from several prospective studies show that animal protein—an integral part of many ketogenic diets—may increase the risk of developing CKD.19,20,50,51
Of equal concern for those without CKD is the high amount of fat in the ketogenic diet. Lin et al.19 showed a higher risk of albuminuria among study participants in the highest quartile of animal fat consumption compared with those in the lowest quartile. In another study, Lin et al.20 demonstrated that a dietary pattern that included higher saturated fat intake is also associated with an increased risk of albuminuria and eGFR decline. In addition, studies have demonstrated a protective effect of many foods that are often excluded from the ketogenic diet, including fruits, vegetables, legumes, and whole grains.65 Exclusion of these foods from the diet may represent an opportunity cost of potential health benefits for the kidney.
Excess consumption of animal protein with the ketogenic diet has also been implicated in the formation of kidney stones.66,67 This may be one reason why, in the pediatric epilepsy community (where the ketogenic diet is used to treat refractory epilepsy in children), nephrolithiasis has been recurrently listed as an adverse effect of the diet.68,69
The acid load consumed and generated among those following a ketogenic diet could also lead to metabolic acidosis and related complications. Case reports exist of ketoacidosis70 among individuals without kidney disease who consume a low-carbohydrate diet. More modest acidosis is caused by both the dietary acid load in individual foods (especially those from animal-based sources) and ketoacids associated with ketone production, combined with the absence of alkali naturally found in many fruits and vegetables that are partially or totally excluded from the ketogenic diet. Several studies within the pediatric epilepsy literature have documented metabolic acidosis in individuals without CKD.68,69 For those with CKD, consuming a high dietary acid load has been associated with a higher risk of ESKD.39 In comparison, consumption of dietary sources of alkali has been shown to delay progression of CKD in a randomized clinical trial.71 Finally, chronic metabolic acidosis in CKD exacerbated by a high dietary acid load may lead to worsened bone health.69,72
High-Protein Diets and Solitary Kidney
Persons with a congenital or acquired solitary kidney—including those who have had a unilateral nephrectomy resulting from living kidney donation, kidney malignancy such as renal cell carcinoma, or trauma—have decreased renal mass. This may lead to glomerular hypertrophy in the setting of increased intraglomerular pressure and glomerular hyperfiltration. These physiologic adaptations of the solitary kidney may lead to unfavorable clinical and renal outcomes over time. Hence, high-protein diets should be avoided, if possible, and plant-based proteins may be recommended. In general, people with one kidney should avoid excessively high dietary protein intake (>1.2 g/kg per day) and high dietary sodium intake; they should also consume adequate dietary fiber and avoid obesity, maintaining a body mass index of <30 kg/m2. Future studies should help us better understand the optimal target protein intake for persons with a congenital or acquired solitary kidney.73
Future Directions
There are substantial gaps in our knowledge about the effects of high-protein diets on kidney health, which may result from difficulties in implementing methodologically rigorous research in this area. For example, challenges in maintaining dietary adherence over a protracted period may partly explain the paucity of randomized clinical trials examining the long-term effects of a high-protein diet on kidney health. Indeed, a number of hypotheses regarding long-term effects of a high-protein diet have been extrapolated from short-term interventional studies.
In addition, the lack of a uniform definition of a high-protein diet (including the total quantity of protein intake), as well as variation in sources of protein across studies, may have contributed to mixed findings. Although there have been numerous observational studies examining associations of long-term high protein intake exposure with kidney function, interpretation of these data are limited by residual confounding as well as challenges in the accurate measurement of protein intake consumption over a prolonged period. For example, although food frequency questionnaires are the preferred method for ascertaining dietary intake in epidemiologic studies, these tools are known to underestimate nutrient consumption, particularly in CKD. Measurement of urinary nitrogen excretion may provide a more accurate assessment of dietary protein intake, but it may be difficult to implement this tool in long-term studies.
Conclusion
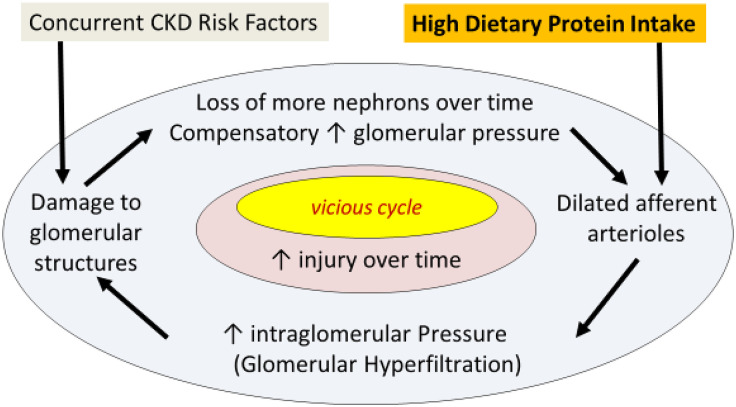
Although there has not been a full elucidation of the underlying mechanisms by which high protein intake may adversely affect kidney function, particularly in the context of CKD, existing data suggest that glomerular hyperfiltration caused by a high-protein diet may lead to an increase in albuminuria and an initial rise and subsequent decline in GFR (Figure 2). Furthermore, growing evidence suggests that high-protein diets may be associated with a number of metabolic complications that may be detrimental to kidney health. Given the rise in popularity of high-protein diets and the high prevalence of CKD in the United States population—including many individuals who may be unaware of their CKD status, further studies are needed to investigate how differences in dietary protein quantity and quality affect short- and long-term outcomes in patients with or without CKD.
Figure 2.
High dietary protein may lead to dilation of afferent arterioles, which results in intraglomerular pressure and glomerular hyperfiltration. It could damage glomerular structure causing compensatory increase of glomerular pressure in remaining glomerulus over time.
Disclosures
K. Kalantar-Zadeh has received honoraria from Abbott, AbbVie, Alexion, Amgen, AstraZeneca, AVEO, Chugai, DaVita, Fresenius, Genentech, Haymarket Media, Hospira, Kabi, Keryx, Novartis, Pfizer, Relypsa, Resverlogix, Sandoz, SanofiAventis, Shire, Vifor, UpToDate and ZS Pharma. All remaining authors have nothing to disclose.
Funding
None.
Supplementary Material
Acknowledgments
Dr. Gang Jee Ko, Dr. Shivam Joshi, and Dr. Kamyar Kalantar-Zadeh reviewed the literature; and all authors were responsible for study concept and design, providing supervision or mentorship, drafting the manuscript, and providing critical revision of the manuscript for important intellectual content. Dr. Kamyar Kalantar-Zadeh is supported by research grants from the National Institutes of Health (NIH)/National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), including R01-DK95668, K24-DK091419, and R01-DK078106, all outside the submitted work. Dr. Kamyar Kalantar-Zadeh is supported by philanthropic grants from Mr. Harold Simmons, Mr. Louis Chang, Dr. Joseph Lee, and AVEO, all outside the submitted work. Dr. Connie M. Rhee is supported by research grants from the NIH/NIDDK including K23-DK102903, R03-DK114642, and R01-DK122767, and philanthropic grants from Dr. Joseph Lee. Dr. Gang Jee Ko was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2019R1F1A1062663), all outside the submitted work.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
Supplemental Material
This article contains the following supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2020010028/-/DCSupplemental.
Supplemental Table 1. Comparison of macronutrient contents of selected popular diets.
References
- 1.World Health Organization : Protein and Amino Acid Requirements in Human Nutrition: Report of a Joint WHO/FAO/UNU Expert Consultation, Geneva, Switzerland, World Health Organization, 2007 [PubMed] [Google Scholar]
- 2.Moore LW, Byham-Gray LD, Scott Parrott J, Rigassio-Radler D, Mandayam S, Jones SL, >.;/>.: The mean dietary protein intake at different stages of chronic kidney disease is higher than current guidelines. Kidney Int 83: 724–732, 2013. [DOI] [PubMed] [Google Scholar]
- 3.Joshi S, Ostfeld RJ, McMacken M: The ketogenic diet for obesity and diabetes-enthusiasm outpaces evidence [published online ahead of print July 15, 2019]. JAMA Intern Med doi:10.1001/jamainternmed.2019.2633 [DOI] [PubMed] [Google Scholar]
- 4.Watzadse G: Über die Harnbildung in der Froschniere. Pflügers Arch 219: 694–705, 1928 [Google Scholar]
- 5.O’Connor WJ, Summerill RA: The effect of a meal of meat on glomerular filtration rate in dogs at normal urine flows. J Physiol 256: 81–91, 1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hostetter TH, Meyer TW, Rennke HG, Brenner BM: Chronic effects of dietary protein in the rat with intact and reduced renal mass. Kidney Int 30: 509–517, 1986. [DOI] [PubMed] [Google Scholar]
- 7.Kamper AL, Strandgaard S: Long-term effects of high-protein diets on renal function. Annu Rev Nutr 37: 347–369, 2017. [DOI] [PubMed] [Google Scholar]
- 8.Moustgaard J: Variation of the renal function in normal and unilaterally nephrectomized dogs. Am J Vet Res 8: 301–306, 1947. [PubMed] [Google Scholar]
- 9.Juraschek SP, Appel LJ, Anderson CA, Miller ER 3rd: Effect of a high-protein diet on kidney function in healthy adults: Results from the OmniHeart trial. Am J Kidney Dis 61: 547–554, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cirillo M, Lombardi C, Chiricone D, De Santo NG, Zanchetti A, Bilancio G: Protein intake and kidney function in the middle-age population: contrast between cross-sectional and longitudinal data. Nephrol Dial Transplant 29: 1733–1740, 2014. [DOI] [PubMed] [Google Scholar]
- 11.Kalantar-Zadeh K, Kramer HM, Fouque D: High-protein diet is bad for kidney health: unleashing the taboo. Nephrol Dial Transplant 35: 1–4, 2020. [DOI] [PubMed] [Google Scholar]
- 12.Knight EL, Stampfer MJ, Hankinson SE, Spiegelman D, Curhan GC: The impact of protein intake on renal function decline in women with normal renal function or mild renal insufficiency. Ann Intern Med 138: 460–467, 2003. [DOI] [PubMed] [Google Scholar]
- 13.Farhadnejad H, Asghari G, Emamat H, Mirmiran P, Azizi F: Low-carbohydrate high-protein diet is associated with increased risk of incident chronic kidney diseases among Tehranian adults. J Ren Nutr 29: 343–349, 2019 [DOI] [PubMed] [Google Scholar]
- 14.Schwingshackl L, Hoffmann G: Comparison of high vs. normal/low protein diets on renal function in subjects without chronic kidney disease: A systematic review and meta-analysis. PLoS One 9: e97656, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oyabu C, Hashimoto Y, Fukuda T, Tanaka M, Asano M, Yamazaki M, >.;/>.: Impact of low-carbohydrate diet on renal function: A meta-analysis of over 1000 individuals from nine randomised controlled trials. Br J Nutr 116: 632–638, 2016. [DOI] [PubMed] [Google Scholar]
- 16.Friedman AN, Ogden LG, Foster GD, Klein S, Stein R, Miller B, >.;/>.: Comparative effects of low-carbohydrate high-protein versus low-fat diets on the kidney. Clin J Am Soc Nephrol 7: 1103–1111, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Møller G, Rikardt Andersen J, Ritz C, Silvestre MP, Navas-Carretero S, Jalo E, >.;/>.: Higher protein intake is not associated with decreased kidney function in pre-diabetic older adults following a one-year intervention-A preview sub-study. Nutrients 10: 54, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Almeida JC, Zelmanovitz T, Vaz JS, Steemburgo T, Perassolo MS, Gross JL, >.;/>.: Sources of protein and polyunsaturated fatty acids of the diet and microalbuminuria in type 2 diabetes mellitus. J Am Coll Nutr 27: 528–537, 2008. [DOI] [PubMed] [Google Scholar]
- 19.Lin J, Fung TT, Hu FB, Curhan GC: Association of dietary patterns with albuminuria and kidney function decline in older white women: A subgroup analysis from the Nurses’ health study. Am J Kidney Dis 57: 245–254, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin J, Hu FB, Curhan GC: Associations of diet with albuminuria and kidney function decline. Clin J Am Soc Nephrol 5: 836–843, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wrone EM, Carnethon MR, Palaniappan L, Fortmann SP; Third National Health and Nutrition Examination Survey : Association of dietary protein intake and microalbuminuria in healthy adults: Third national health and nutrition examination survey. Am J Kidney Dis 41: 580–587, 2003. [DOI] [PubMed] [Google Scholar]
- 22.Coppo R, Amore A, Roccatello D, Martina G, Rollino C, Basolo B, >.;/>.: Microalbuminuria in single kidney patients: relationship with protein intake. Clin Nephrol 29: 219–228, 1988. [PubMed] [Google Scholar]
- 23.Luger M, Holstein B, Schindler K, Kruschitz R, Ludvik B: Feasibility and efficacy of an isocaloric high-protein vs. standard diet on insulin requirement, body weight and metabolic parameters in patients with type 2 diabetes on insulin therapy. Exp Clin Endocrinol Diabetes 121: 286–294, 2013 [DOI] [PubMed] [Google Scholar]
- 24.Tay J, Thompson CH, Luscombe-Marsh ND, Noakes M, Buckley JD, Wittert GA, >.;/>.: Long-term effects of a very low carbohydrate compared with a high carbohydrate diet on renal function in individuals with type 2 diabetes: a randomized trial. Medicine (Baltimore) 94: e2181, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krebs JD, Elley CR, Parry-Strong A, Lunt H, Drury PL, Bell DA, >.;/>.: The diabetes excess weight loss (DEWL) trial: a randomised controlled trial of high-protein versus high-carbohydrate diets over 2 years in type 2 diabetes. Diabetologia 55: 905–914, 2012. [DOI] [PubMed] [Google Scholar]
- 26.Larsen RN, Mann NJ, Maclean E, Shaw JE: The effect of high-protein, low-carbohydrate diets in the treatment of type 2 diabetes: a 12 month randomised controlled trial. Diabetologia 54: 731–740, 2011. [DOI] [PubMed] [Google Scholar]
- 27.Li Z, Treyzon L, Chen S, Yan E, Thames G, Carpenter CL: Protein-enriched meal replacements do not adversely affect liver, kidney or bone density: an outpatient randomized controlled trial. Nutr J 9: 72, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Skov AR, Toubro S, Bülow J, Krabbe K, Parving HH, Astrup A: Changes in renal function during weight loss induced by high vs low-protein low-fat diets in overweight subjects. Int J Obes Relat Metab Disord 23: 1170–1177, 1999 [DOI] [PubMed] [Google Scholar]
- 29.Björnson Granqvist A, Ericsson A, Sanchez J, Tonelius P, William-Olsson L, Dahlqvist U, >.;/>.: High-protein diet accelerates diabetes and kidney disease in the BTBRob/ob mouse. Am J Physiol Renal Physiol 318: F763–F771, 2020. [DOI] [PubMed] [Google Scholar]
- 30.Kalantar-Zadeh K, Fouque D: Nutritional management of chronic kidney disease. N Engl J Med 377: 1765–1776, 2017. [DOI] [PubMed] [Google Scholar]
- 31.Brenner BM, Lawler EV, Mackenzie HS: The hyperfiltration theory: a paradigm shift in nephrology. Kidney Int 49: 1774–1777, 1996. [DOI] [PubMed] [Google Scholar]
- 32.Tovar-Palacio C, Tovar AR, Torres N, Cruz C, Hernández-Pando R, Salas-Garrido G, >.;/>.: Proinflammatory gene expression and renal lipogenesis are modulated by dietary protein content in obese Zucker fa/fa rats. Am J Physiol Renal Physiol 300: F263–F271, 2011. [DOI] [PubMed] [Google Scholar]
- 33.Jia Y, Hwang SY, House JD, Ogborn MR, Weiler HA, O K, >.;/>.: Long-term high intake of whole proteins results in renal damage in pigs. J Nutr 140: 1646–1652, 2010. [DOI] [PubMed] [Google Scholar]
- 34.Frank H, Graf J, Amann-Gassner U, Bratke R, Daniel H, Heemann U, >.;/>.: Effect of short-term high-protein compared with normal-protein diets on renal hemodynamics and associated variables in healthy young men [published correction appears in Am J Clin Nutr 91: 494, 2010]. Am J Clin Nutr 90: 1509–1516, 2009. [DOI] [PubMed] [Google Scholar]
- 35.Weiner ID, Mitch WE, Sands JM: Urea and ammonia metabolism and the control of renal nitrogen excretion. Clin J Am Soc Nephrol 10: 1444–1458, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wesson DE, Buysse JM, Bushinsky DA: Mechanisms of metabolic acidosis-induced kidney injury in chronic kidney disease. J Am Soc Nephrol 31: 469–482, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lennon EJ, Lemann J Jr., Litzow JR: The effects of diet and stool composition on the net external acid balance of normal subjects. J Clin Invest 45: 1601–1607, 1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scialla JJ, Anderson CA: Dietary acid load: a novel nutritional target in chronic kidney disease? Adv Chronic Kidney Dis 20: 141–149, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Banerjee T, Crews DC, Wesson DE, Tilea AM, Saran R, Ríos-Burrows N, >.;/>.: Centers for Disease Control and Prevention Chronic Kidney Disease Surveillance Team : High dietary acid load predicts ESRD among adults with CKD. J Am Soc Nephrol 26: 1693–1700, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Karavetian M, Rizk R: Patient education for hyperphosphatemia management: improving outcomes while decreasing costs? Kidney Res Clin Pract 37: 4–7, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kalantar-Zadeh K, Gutekunst L, Mehrotra R, Kovesdy CP, Bross R, Shinaberger CS, >.;/>.: Understanding sources of dietary phosphorus in the treatment of patients with chronic kidney disease. Clin J Am Soc Nephrol 5: 519–530, 2010. [DOI] [PubMed] [Google Scholar]
- 42.Fouque D, Roth H, Pelletier S, London GM, Hannedouche T, Jean G, >.;/>.: Control of mineral metabolism and bone disease in haemodialysis patients: which optimal targets? Nephrol Dial Transplant 28: 360–367, 2013. [DOI] [PubMed] [Google Scholar]
- 43.de Boer IH, Rue TC, Kestenbaum B: Serum phosphorus concentrations in the third national health and nutrition examination survey (NHANES III). Am J Kidney Dis 53: 399–407, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chang AR, Lazo M, Appel LJ, Gutiérrez OM, Grams ME: High dietary phosphorus intake is associated with all-cause mortality: results from NHANES III. Am J Clin Nutr 99: 320–327, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Burnett S-AM, Gunawardene SC, Bringhurst FR, Jüppner H, Lee H, Finkelstein JS: Regulation of C-terminal and intact FGF-23 by dietary phosphate in men and women. J Bone Miner Res 21: 1187–1196, 2006 [DOI] [PubMed] [Google Scholar]
- 46.Nasrallah MM, El-Shehaby AR, Salem MM, Osman NA, El Sheikh E, Sharaf El Din UA: Fibroblast growth factor-23 (FGF-23) is independently correlated to aortic calcification in haemodialysis patients. Nephrol Dial Transplant 25: 2679–2685, 2010. [DOI] [PubMed] [Google Scholar]
- 47.Faul C, Amaral AP, Oskouei B, Hu MC, Sloan A, Isakova T, et al.: FGF23 induces left ventricular hypertrophy. J Clin Invest 121: 4393–4408, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ix JH, Katz R, Kestenbaum BR, de Boer IH, Chonchol M, Mukamal KJ, et al.: Fibroblast growth factor-23 and death, heart failure, and cardiovascular events in community-living individuals: CHS (cardiovascular health study). J Am Coll Cardiol 60: 200–207, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zoccali C, Ruggenenti P, Perna A, Leonardis D, Tripepi R, Tripepi G, et al.: REIN Study Group : Phosphate may promote CKD progression and attenuate renoprotective effect of ACE inhibition. J Am Soc Nephrol 22: 1923–1930, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Haring B, Selvin E, Liang M, Coresh J, Grams ME, Petruski-Ivleva N, et al.: Dietary protein sources and risk for incident chronic kidney disease: Results from the atherosclerosis risk in communities (ARIC) study. J Ren Nutr 27: 233–242, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lew QJ, Jafar TH, Koh HW, Jin A, Chow KY, Yuan JM, et al.: Red meat intake and risk of ESRD. J Am Soc Nephrol 28: 304–312, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Joshi S, Ettinger L, Liebman SE: Plant-based diets and hypertension [published online ahead of print September 24, 2019]. Am J Lifestyle Med doi:10.1177/1559827619875411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chauveau P, Koppe L, Combe C, Lasseur C, Trolonge S, Aparicio M: Vegetarian diets and chronic kidney disease. Nephrol Dial Transplant 34: 199–207, 2019. [DOI] [PubMed] [Google Scholar]
- 54.Kalantar-Zadeh K, Moore LW: Does kidney longevity mean healthy vegan food and less meat or is any low-protein diet good enough? J Ren Nutr 29: 79–81, 2019 [DOI] [PubMed] [Google Scholar]
- 55.Karanja NM, Obarzanek E, Lin PH, McCullough ML, Phillips KM, Swain JF, et al.: Descriptive characteristics of the dietary patterns used in the dietary approaches to stop hypertension trial. DASH Collaborative Research Group. J Am Diet Assoc 99[Suppl]: S19–S27, 1999. [DOI] [PubMed] [Google Scholar]
- 56.Tomova A, Bukovsky I, Rembert E, Yonas W, Alwarith J, Barnard ND, et al.: The effects of vegetarian and vegan diets on gut microbiota. Front Nutr 6: 47, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mafra D, Borges NA, Cardozo LFMF, Anjos JS, Black AP, Moraes C, et al.: Red meat intake in chronic kidney disease patients: two sides of the coin. Nutrition 46: 26–32, 2018. [DOI] [PubMed] [Google Scholar]
- 58.Barros AF, Borges NA, Ferreira DC, Carmo FL, Rosado AS, Fouque D, et al.: Is there interaction between gut microbial profile and cardiovascular risk in chronic kidney disease patients? Future Microbiol 10: 517–526, 2015. [DOI] [PubMed] [Google Scholar]
- 59.Black AP, Anjos JS, Cardozo L, Carmo FL, Dolenga CJ, Nakao LS, et al.: Does low-protein diet influence the uremic toxin serum levels from the gut microbiota in nondialysis chronic kidney disease patients? J Ren Nutr 28: 208–214, 2018 [DOI] [PubMed] [Google Scholar]
- 60.Derry MM, Raina K, Agarwal C, Agarwal R: Identifying molecular targets of lifestyle modifications in colon cancer prevention. Front Oncol 3: 119, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Montonen J, Boeing H, Fritsche A, Schleicher E, Joost HG, Schulze MB, et al.: Consumption of red meat and whole-grain bread in relation to biomarkers of obesity, inflammation, glucose metabolism and oxidative stress. Eur J Nutr 52: 337–345, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Joshi S, Shah S, Kalantar-Zadeh K: Adequacy of plant-based proteins in chronic kidney disease. J Ren Nutr 29: 112–117, 2019 [DOI] [PubMed] [Google Scholar]
- 63.Phinney S, Volek J, Volk B: How much protein do you need in nutritional ketosis, 2008. Available at https://blog.virtahealth.com/how-much-protein-on-keto/. Accessed June 6, 2020
- 64.Kasiske BL, Lakatua JD, Ma JZ, Louis TA: A meta-analysis of the effects of dietary protein restriction on the rate of decline in renal function. Am J Kidney Dis 31: 954–961, 1998. [DOI] [PubMed] [Google Scholar]
- 65.Kim H, Caulfield LE, Garcia-Larsen V, Steffen LM, Grams ME, Coresh J, et al.: Plant-based diets and incident CKD and kidney function. Clin J Am Soc Nephrol 14: 682–691, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Shu X, Calvert JK, Cai H, Xiang YB, Li H, Zheng W, et al.: Plant and animal protein intake and risk of incident kidney stones: results from the Shanghai men’s and women’s health studies. J Urol 202: 1217–1223, 2019. [DOI] [PubMed] [Google Scholar]
- 67.Tracy CR, Best S, Bagrodia A, Poindexter JR, Adams-Huet B, Sakhaee K, et al.: Animal protein and the risk of kidney stones: a comparative metabolic study of animal protein sources. J Urol 192: 137–141, 2014. [DOI] [PubMed] [Google Scholar]
- 68.Freeman JM, Vining EP, Pillas DJ, Pyzik PL, Casey JC, Kelly LM: The efficacy of the ketogenic diet-1998: a prospective evaluation of intervention in 150 children. Pediatrics 102: 1358–1363, 1998. [DOI] [PubMed] [Google Scholar]
- 69.Kang HC, Chung DE, Kim DW, Kim HD: Early- and late-onset complications of the ketogenic diet for intractable epilepsy. Epilepsia 45: 1116–1123, 2004. [DOI] [PubMed] [Google Scholar]
- 70.Shah P, Isley WL: Ketoacidosis during a low-carbohydrate diet. N Engl J Med 354: 97–98, 2006. [DOI] [PubMed] [Google Scholar]
- 71.Goraya N, Simoni J, Jo CH, Wesson DE: Treatment of metabolic acidosis in patients with stage 3 chronic kidney disease with fruits and vegetables or oral bicarbonate reduces urine angiotensinogen and preserves glomerular filtration rate. Kidney Int 86: 1031–1038, 2014. [DOI] [PubMed] [Google Scholar]
- 72.Siener R: Dietary treatment of metabolic acidosis in chronic kidney disease. Nutrients 10: 512, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tantisattamo E, Dafoe DC, Reddy UG, Ichii H, Rhee CM, Streja E, et al.: Current management of patients with acquired solitary kidney. Kidney Int Rep 4: 1205–1218, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Huang MC, Chen ME, Hung HC, Chen HC, Chang WT, Lee CH, et al.: Inadequate energy and excess protein intakes may be associated with worsening renal function in chronic kidney disease. J Ren Nutr 18: 187–194, 2008 [DOI] [PubMed] [Google Scholar]
- 75.Halbesma N, Bakker SJ, Jansen DF, Stolk RP, De Zeeuw D, De Jong PE, et al.: PREVEND Study Group : High protein intake associates with cardiovascular events but not with loss of renal function. J Am Soc Nephrol 20: 1797–1804, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Beasley JM, Katz R, Shlipak M, Rifkin DE, Siscovick D, Kaplan R: Dietary protein intake and change in estimated GFR in the cardiovascular health study. Nutrition 30: 794–799, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Malhotra R, Lipworth L, Cavanaugh KL, Young BA, Tucker KL, Carithers TC, et al.: Protein intake and long-term change in glomerular filtration rate in the Jackson heart study. J Ren Nutr 28: 245–250, 2018 [DOI] [PubMed] [Google Scholar]
- 78.Esmeijer K, Geleijnse JM, de Fijter JW, Kromhout D, Hoogeveen EK: Dietary protein intake and kidney function decline after myocardial infarction: the alpha omega cohort. Nephrol Dial Transplant 35: 106–115, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Jhee JH, Kee YK, Park S, Kim H, Park JT, Han SH, et al.: High-protein diet with renal hyperfiltration is associated with rapid decline rate of renal function: a community-based prospective cohort study. Nephrol Dial Transplant 35: 98–106, 2020. [DOI] [PubMed] [Google Scholar]
- 80.Flechtner-Mors M, Boehm BO, Wittmann R, Thoma U, Ditschuneit HH: Enhanced weight loss with protein-enriched meal replacements in subjects with the metabolic syndrome. Diabetes Metab Res Rev 26: 393–405, 2010. [DOI] [PubMed] [Google Scholar]
- 81.Yancy WS Jr., Westman EC, McDuffie JR, Grambow SC, Jeffreys AS, Bolton J, et al.: A randomized trial of a low-carbohydrate diet vs orlistat plus a low-fat diet for weight loss. Arch Intern Med 170: 136–145, 2010. [DOI] [PubMed] [Google Scholar]
- 82.Wycherley TP, Brinkworth GD, Clifton PM, Noakes M: Comparison of the effects of 52 weeks weight loss with either a high-protein or high-carbohydrate diet on body composition and cardiometabolic risk factors in overweight and obese males. Nutr Diabetes 2: e40, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tirosh A, Golan R, Harman-Boehm I, Henkin Y, Schwarzfuchs D, Rudich A, et al.: Renal function following three distinct weight loss dietary strategies during 2 years of a randomized controlled trial. Diabetes Care 36: 2225–2232, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Oosterwijk MM, Soedamah-Muthu SS, Geleijnse JM, Bakker SJL, Navis G, Binnenmars SH, et al.: High dietary intake of vegetable protein is associated with lower prevalence of renal function impairment: results of the Dutch DIALECT-1 cohort. Kidney Int Rep 4: 710–719, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.