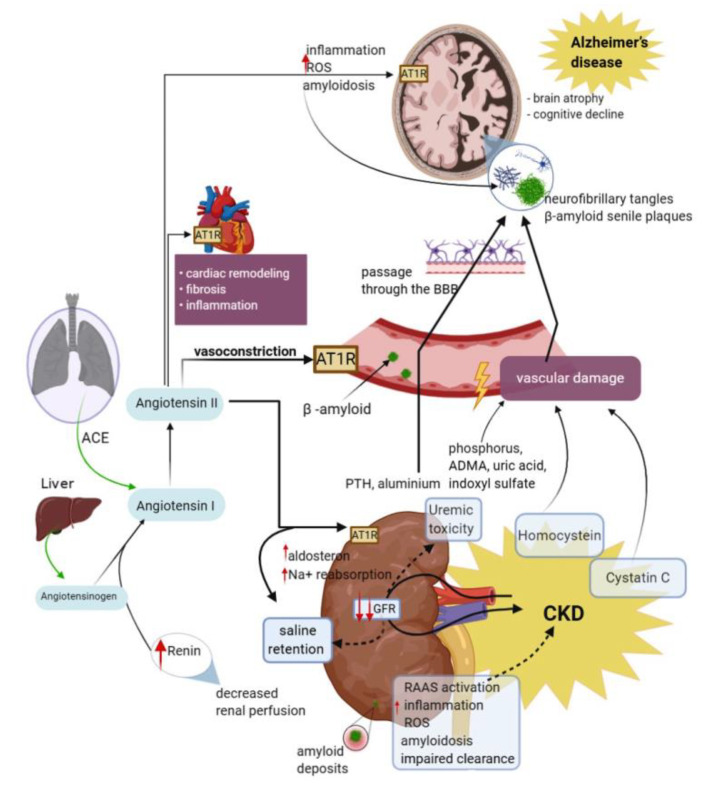
Figure 2.
Schematic representation of mechanisms implicated in cognitive decline and AD in CKD patients, comprising renin–angiotensin system, oxidative stress, vascular injury, and inflammation. Diminished glomerular filtration rate and renal perfusion affect renal clearance. Renal retention of oxidizing substances promotes the intensification of oxidative stress and inflammation, which together with a defective clearance, causes an increase in plasma concentrations of uremic toxins, homocysteine, Cystatin C, amyloid deposits, and other molecules. These substances exert their toxic action through various mechanisms. Low renal perfusion leads to increased renin synthesis, and in its presence, the angiotensinogen synthesized in the liver is transformed into angiotensin I, which in turn, in the presence of angiotensin converting enzyme passes into angiotensin II. Angiotensin II activates AT1 receptors and produces hydro-saline retention, cardiac remodeling, vasoconstriction, and the development of β-amyloid deposits. The consequences of kidney damage are also reflected in the vascular and cerebral level with the aggravation of the cognitive deficit present in AD. The potential mechanisms of kidney–brain crosstalk regarding inflammatory molecules are because cytokines frequently involved in the pathogenesis of CKD may influence remote organs, such as the brain. The pathogenesis of the oxidative stress in patients with CKD is exhaustive, uremia and dialysis being among the important and frequent factors. Moreover, in these patients, an excessive increase in ROS was linked to the inflammatory processes, as the presence of endogenous oxidants and uremic toxins in the plasma may be a source of oxidative stress. Nevertheless, vascular damage and the direct neurotoxicity of uremic toxins produced by renal altered function are the most reasonable pathways of the effects of CKD in AD patients. AD, Alzheimer’s disease; ANG I, angiotensin I; ANG II, angiotensin II; ACE, angiotensin converting enzyme; RAAS, renin–angiotensin–aldosterone system; BBB, blood–brain barrier; GFR, glomerular filtration rate; AT1R, angiotensin II receptor type 1; ROS, reactive oxygen species; Na, sodium; ADMA, asymmetric dimethylarginine; CKD, chronic kidney disease.