Figure 3. Microbial regulation of oral immune tolerance to food and its breakdown in FA.
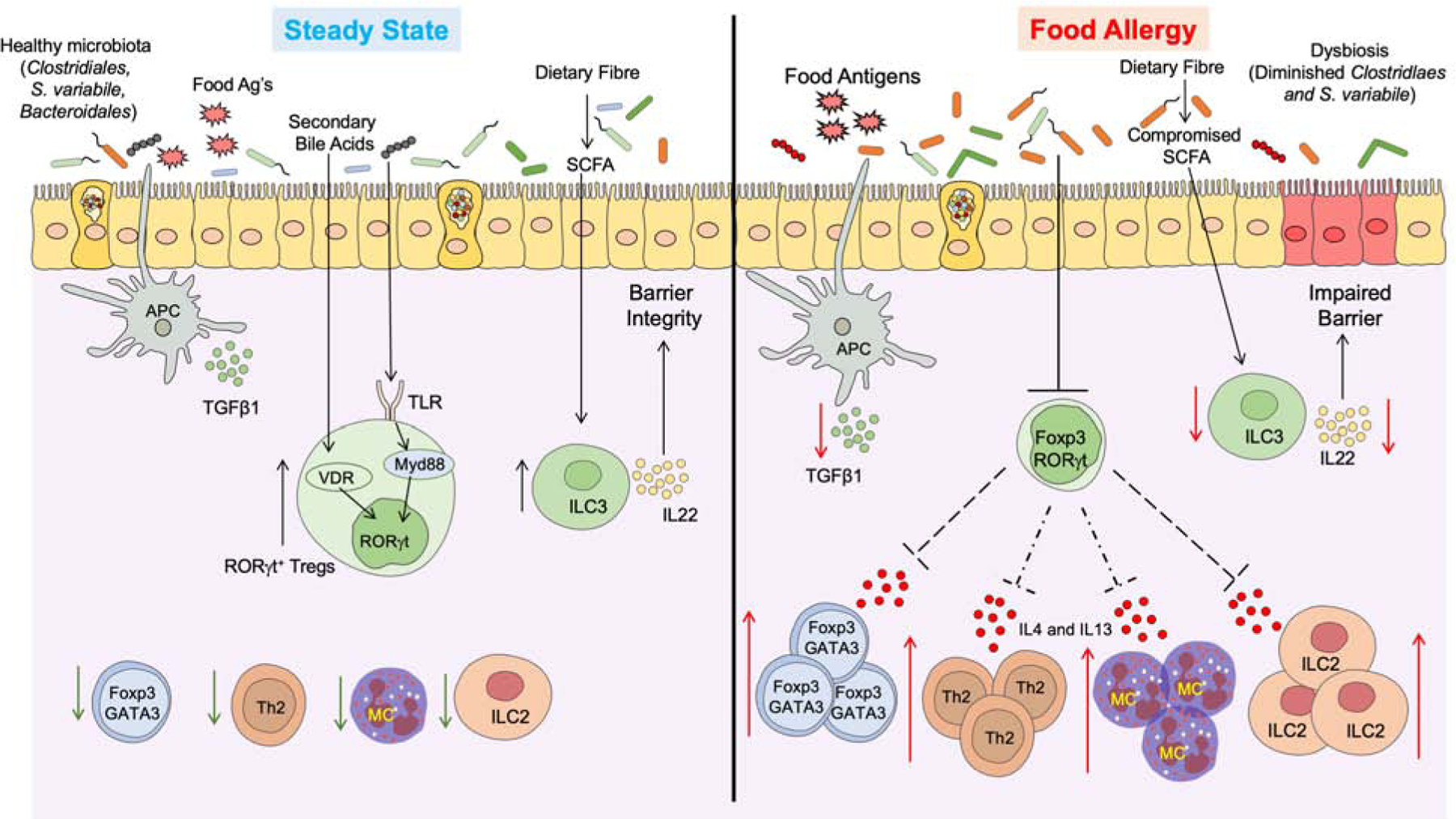
(Left) Under homeostatic conditions antigen presenting cells (classical CD103+ dendritic cells) sample the gut lumen and promote the formation of nascent dietary antigen-specific iTreg cells. Commensals, including Clostridiales and Bacteroidales species, deliver further signals via MyD88 in nascent iTreg cells to drive the expression of ROR-γt. Additionally differentiation signals include secondary bile acid metabolites, which promote the differentiation of ROR-γt by activating vitamin-D receptor in iTreg cells. ROR-γt+ Treg cells may regulate tolerance to dietary antigens by inhibiting antigen-specific helper Th 2 (Th2) cell responses, impeding the formation of pathogenic Th2 cell-like reprogramming of Treg cells, suppression of mast cells cell and innate lymphoid cell (ILC)-2 activation. SCFAs produced by the degradation of complex carbohydrates activates ILC3-dependent secretion of IL22 to promote barrier functions. (Right) The underlying dysbiosis in FA compromises barrier integrity and impairs the differentiation of ROR-γt+ iTreg cells, while augmenting the expansion of Treg cells with a Th2 cell-like phenotype that express GATA3 and IL-4. These pathogenic Treg cells license the gut tissue immune response by Th2 cells, Mast cells, and ILC2 to promote disease pathogenesis.
