Figure 4: Current and projected treatment modalities for FA.
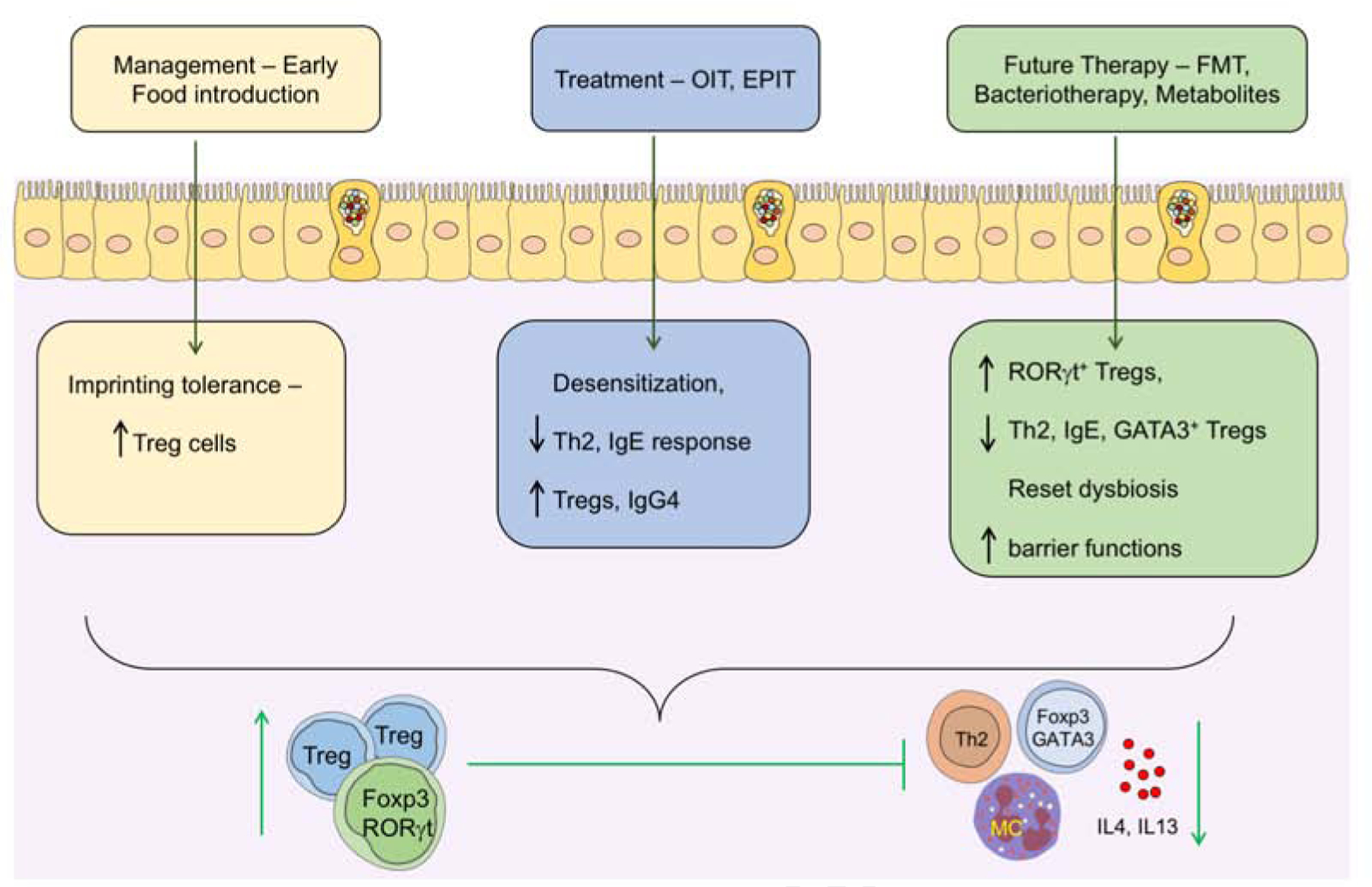
Introduction of common food allergens early in life leads to the development of tolerance possibly by coinciding with the weaning reaction and imprinting durable allergen-specific iTregs cells. In FA subjects who fail to imprint early life tolerance, treatment with either OIT or EPIT results in a state of desensitization that may evolve in some patients into sustained unresponsiveness or oral tolerance to the suspect food. Immunotherapy may act by several mechanisms including the induction of allergen-specific iTregs cells and the inhibition of mast cells and basophils by concomitantly augmenting allergen-specific blocking IgG4 antibodies while suppressing allergen-specific IgE responses. Immunotherapy may also promote the deletion of Th2 cells, and the reversal of pathogenic Th2 cell-like reprogramming of Treg cells. Because immunotherapy fails to induce sustained oral tolerance in many patients, alternate therapies targeting the gut microbiota and their metabolites are currently being explored, including FMT, rationally designed bacterial consortia and precision-based individual bacterial strains and microbiota-derived metabolites. These therapies have the potential to recapitulate early life imprinting by inducing ROR-γt+ Treg cells and, in the case of microbial therapies, to reset the underlying dysbiosis.
