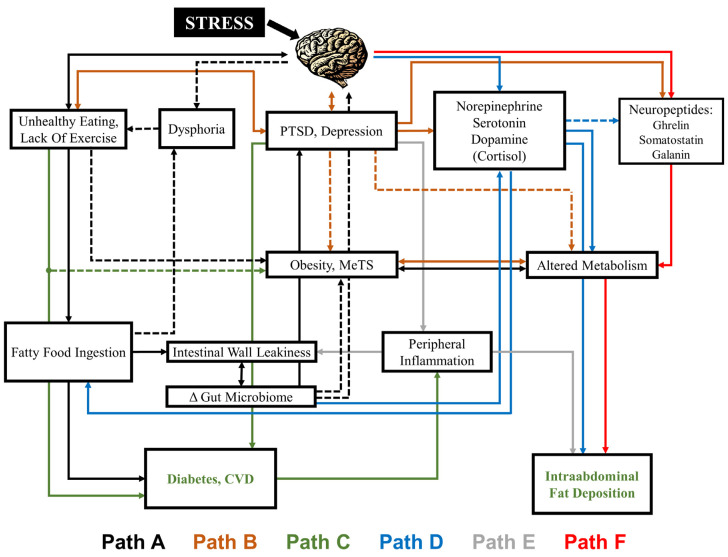
Figure 1.
The complex relationship between diet, obesity and behavior. Stress acts through the brain to both affect eating and exercise behaviors (Path A) and stress-related psychiatric disorders including posttraumatic stress disorder (PTSD) and depression (Path B), both of which can lead to changes in metabolism, metabolic syndrome (MetS) and obesity (Paths A and B). Binary relationships also exist between unhealthy eating and PTSD/depression and the brain (i.e., both in turn lead to changes in brain function). Unhealthy eating can result in diets high in saturated fat (fatty food ingestion) (Path A) that can affect mood (dysphoria) as well as leakiness of the intestinal wall (Path A), which can lead to changes in the gut microbiome which modulate obesity, MetS and metabolism (Path A), as well as feeding back on the brain (Path A) to influence mood (dysphoria). Physical disorders including cardiovascular disease (CVD) and diabetes (Path C) and physical factors such as intra-abdominal fat (Path C) are affected by stress and related to PTSD and depression. A complex system of neurotransmitters (norepinephrine, serotonin, dopamine) (Path D), inflammatory markers (Path E) and neuropeptides (ghrelin, somatostatin, galanin) (Path F) present in the gut and brain are also influenced by stress via the brain, influence the gut microbiota and physical disorders and factors in a binary fashion and in turn regulate both feeding behavior and psychiatric disorders. Within the figure, the line color indicates the path, with dashed lines indicating primary pathways and solid lines indicating secondary pathways.